A 4-year-old girl presented with multiple asymptomatic nodules on the back and lower limbs, which progressively appeared over the last year. Skin examination revealed more than ten, firm, erythematous to flesh-colored, grouped nodules, tending to coalesce, ranging 10-15 mm in diameter. They were asymmetrically distributed over the right lumbar region, left thigh (Fig. 1) and anterior aspect of legs. The patient's mother had similar lesions in the lumbar region and thighs, which had remained stable since childhood. Both were otherwise healthy.
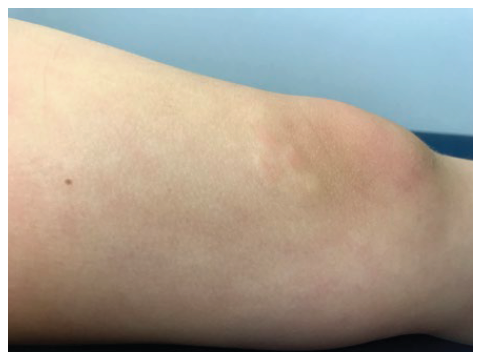
Figure 1 Four grouped, erythematous nodules, with 10-15 mm in diameter, on the upper-inner aspect of the left knee.
Thyroid function, antinuclear antibodies and serum protein electrophoresis were unremarkable. Skin biopsy showed increased mucin deposition between collagen fibers in the mid and deep re-ticular dermis, with slight proliferation of fibroblasts (Fig. 2). Mucin stained positive with colloidal iron (Fig. 3), suggesting the diagnosis of nodular lichen myxedematosus.
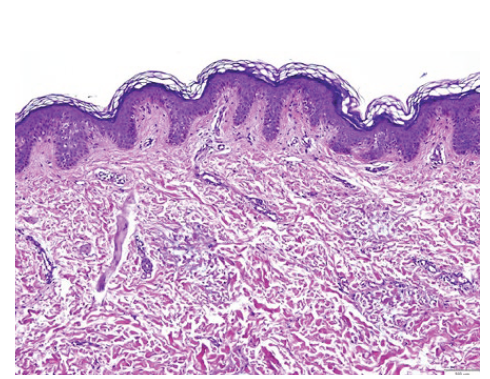
Figure 2 Photomicrograph showing increased mucin deposition in dermis with separation of collagen fibers (hematoxylin and eosin, x100).
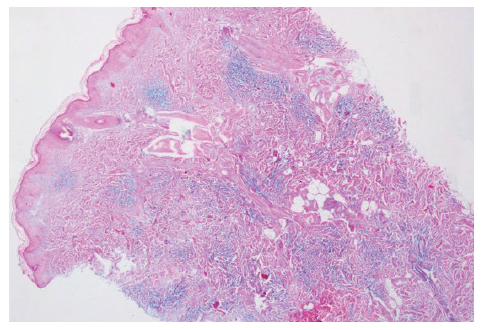
Figure 3 Colloidal iron stain highlighting the interstitial deposition of mucin in reticular dermis (x40).
Lichen myxedematosus (LM), also known as papular mucinosis, is characterized by lichenoid papules, nodules and plaques due to dermal mucin deposition and variable degree of fibrosis, without thyroid dysfunction.1 It is uncommon in children.2 LM is divided into two main clinicopathologic subsets: generalized papular and sclerodermoid form (scleromyxedema), associated with monoclonal gammopathy and systemic manifestations; and localized form, which presents no sclerotic features, paraproteinemia or systemic involvement.1
Localized LM is further classified into: (1) discrete papular form, characterized by multiple symmetrically distributed, 2-5 mm, waxy papules on the trunk and limbs, that rarely resolve spontaneously; (2) acral persistent papular mucinosis, which develops exclusively on the dorsal aspect of the hands and extensor surface of the distal forearms, without spontaneous resolution; (3) cutaneous mucinosis of infancy, a pediatric variant of the two previous subtypes, occurring at birth or in the first months or years of life; and (4) nodular LM, characterized by multiple nodules on the limbs and trunk, with mild or absent papular component.1-3
Histologic features of localized LM are less characteristic than those of scleromyxedema, with variable fibroblast proliferation and scarce fibrosis. Mucin deposits between collagen bundles can be highlighted with Alcian blue and colloidal iron stains. In acral per-sistent papular mucinosis, mucin accumulates focally in the upper dermis sparing a subepidermal zone, with a regular number of fibroblasts. In cutaneous mucinosis of infancy, mucin is very superficial, but a deeper involvement may occur in the nodular subtype.3,4
Our case was diagnosed as nodular LM based on clinicopathological correlation, and absence of thyroid disorder, paraproteinemia or systemic manifestations. A limited number of small nodules randomly distributed on the lumbar region and lower limbs is not consistent with cutaneous mucinosis of infancy. Mucin deposition extending into the deep dermis also supports our diagnosis.
The pathogenesis of localized LM is unclear, without apparent relation to mucin production stimulated by autoantibodies, immunoglobulins, pro-inflammatory cytokines or infectious agents.1,2In our case, clinical similarities between the mother and the patient’s lesions raised the hypothesis of a familial association, although rare cases of familial localized LM have been described, suggesting a genetically mediated pathogenesis.3,5
The differential diagnosis of nodular LM in childhood encom-passes other dermatosis presenting with nodules or plaques, namely self-healing juvenile cutaneous mucinosis (SHJCM), collagenomas and subcutaneous granuloma annulare. SHJCM is another primary cutaneous mucinosis distinguished by an acute eruption of papules and nodules, with possible involvement of the face and periarticular areas, in addition to systemic symptoms and spontaneous resolution. A differentiating histologic feature of the latter is the remarkable increase in the number of fibroblasts, with bands of fibrosis.2
Treatment for localized LM is not required. Topical application of moderate to high potency corticosteroids or tacrolimus has been used with variable success,6 as well as local injections of triamcino-lone acetonide or hyaluronidase.7 In our case, lesions stabilized without treatment after 1-year follow-up.
Presentations/Apresentações
This work has already been presented as an oral communica-tion in the XIX Congress of the Portuguese Society of Dermatology and Venereology, 6-8th December 2019, Porto.















