Introduction
Disseminated peritoneal leiomyomatosis (DPL), also known as leiomyomatosis peritonealis disseminata, is a rare disease characterized by multiple tumors derived from smooth muscles disseminated throughout the peritoneal cavity. It was first described in 1952 by Wilson and Peale1 and until recently only around 200 cases have been reported in the English literature. However, as the majority are asymptomatic, this condition may be underdiagnosed, and it is usually found incidentally. Although typically benign, DPL may degenerate into malignancy.2
Differential diagnosis mainly includes peritoneal carcinomatosis or metastatic disease; the clinical and radiological features can help differentiate these entities, but only histopathological examination achieves the final diagnosis.3,4
Case Presentation
A 30-year-old woman proceeded to our institution due to a tumor with left para-uterine location found during a transvaginal ultrasound scan, during infertility workup. She had undergone laparoscopic broad ligament myomectomy
5 years previously. A broad ligament leiomyoma was suspected. However, there was an elevated level of CA 125 (50 U/ml), which required the exclusion of an adnexal tumor by ultrasound.
A Computed Tomography (CT) was requested and revealed three intraperitoneal soft tissue density masses in the pelvic cavity: one near the left para-uterine margin, and the other two located superiorly, one on the right and the other more central (Fig. 1).
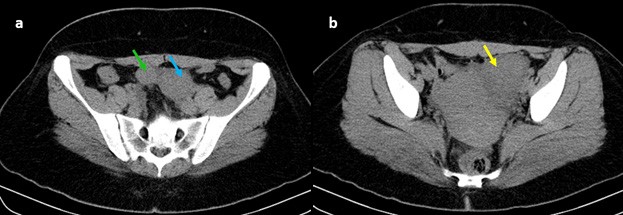
Figure. 1: Axial computed tomography without intravenous contrast administration shows three peritoneal soft-tissue density tumors in the pelvic cavity: one near the left para-uterine margin (yellow arrow), and the other two located supe- riorly, one on the right (green arrow) and the other more central (blue arrow).
Magnetic Resonance Imaging (MRI) was performed for better characterization and showed tree well-defined masses with heterogeneous and intermediate signal intensity on T2 weighted images (T2WI) (Figs. 2a-e) and low signal intensity on T1 weighted images (T1WI) (Figs. 2e-g). On T1W post-contrast image tumors presented strong and heterogeneous enhancement (Figs. 2h-j), particularly the one in the left para-uterine region, which was the biggest. They also showed restricted diffusion with high signal on DW images and low signal on ADC map (Fig. 3).
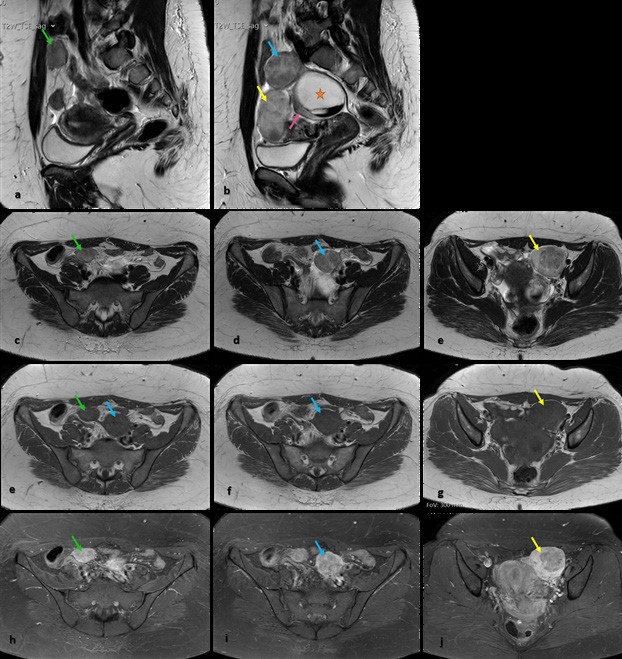
Figure 2: MRI shows tree well-defined and heterogeneous tumors, with intermediate signal intensity on sagittal (1a, 1b) and axial (1c-1e) T2WI, and with low signal intensity on T1WI (e-g): one near the left para-uterine margin (yellow arrow), and the other two located superiorly, one on the right (green arrow) and the other more central (blue arrow). Tumors present strong but heterogeneous enhancement on T1W post-contrast image (h-j), particularly the one who was in the left para-uterine region (yellow arrow). There is still a large high signal intensity cystic mass (orange star) with a level formed by a hypointense blood clot in the lower portion; cyst arises from the right ovary (pink arrow) - “positive beak sign” - well seen on sagittal T2WI (1b).
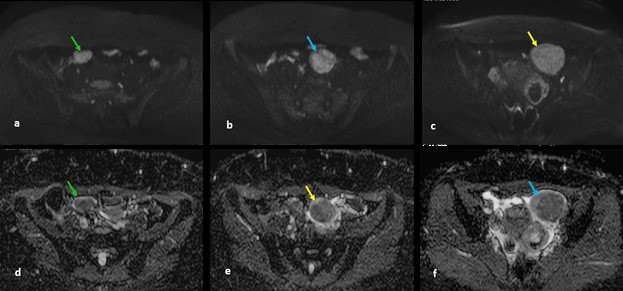
Figure 3: MRI shows three tumors with high signal intensity on axial diffusion-weighted imaging (b1000) (a-c) and low signal intensity on axial ADC map (d-f), corroborating the presence of restricted diffusion.
Three months later she underwent surgical resection. The histological diagnosis revealed three fasciculate and elastic tumors, well delimited, with no malignant features, compatible with DPL.
Discussion Conclusion
Disseminated peritoneal leiomyomatosis (DPL) is a rare disease characterized by multiple tumors derived from smooth muscles spread throughout the peritoneum.
There are several hypotheses about the etiology and pathophysiology of DPL. The two most consensual are hormonal and iatrogenic theories.
The hormonal theory suggests that DPL results from the metaplastic change of mesenchymal stem cells with exposure to high levels of endogenous or exogenous estrogens. This is convincing because, this entity occurs most commonly in women of childbearing age, during pregnancy, and after prolonged administration of oral contraceptive pills or hormone replacement therapy;5 however, there are also a few cases reported in postmenopausal women and in male patients.4,6,7
As occurred in this case, DPL may present even years after laparoscopic myomectomy or hysterectomy with tumor morcellation.8 According to the iatrogenic theory, these surgical techniques increase the risk of intra-abdominal dispersion of residual tumor debris, leading to peritoneal dissemination.9,10
There are reports of DPL without a history of uterine leiomyoma, suggesting that these tumors could originate from extrauterine spindle cell tumors.11 Our patient also had a previous history of one broad ligament leiomyoma. As many cases are asymptomatic, these tumors are usually found incidentally. Some patients may present with pelvic pain or pelvic and abdominal compression symptoms. Tumors can involve the bladder or an intestinal segment and lead to intestinal obstruction.10
At CT, DPL presents itself as multiple solid subcentimeter nodules or as large soft tissue density masses in the peritoneal cavity, homogeneous or heterogeneous, with variable enhancement pattern like uterine leiomyomas.
Pelvic MRI is the most accurate modality for detection, location and characterization of DPL due to its excellent soft-tissue contrast resolution and multiplanar imaging capability; it allows evaluation of disease extension and its relationship with surrounding structures. On T1 and T2 weighted images, these tumors usually present low to intermediate signal intensity compared with the normal myometrium; however, they may undergo degeneration showing variable appearances. Following intravenous administration of gadolinium, on T1 weighted images, variable enhancement may be seen but usually DPL shows homogeneous and strong enhancement.
Differential diagnosis mainly includes peritoneal carcinomatosis or metastatic disease; the clinical and radiological features can help to differentiate these entities, but only histological analysis can reveal the final diagnosis.3,4 The histopathological examination usually shows smooth- muscle cell proliferation with no atypia or necrosis. Malignant changes can be seen very rarely.2,12,13
Concerning the treatment of DPL there are no clear guidelines.1 It has been proposed that therapy should be individualized according to the patient’s condition, considering age, comorbidities and severity of symptoms.14 A conservative approach including hormonal treatment with gonadotrophin releasing hormone agonists or stopping the contraceptive pills seem good alternatives for women with reproductive desire.1,5 For postmenopausal women or without reproductive desire, or even in cases of a high risk of malignant degeneration, surgical approach (usually with total abdominal hysterectomy, salpingo- oophorectomy, omentectomy and debulking) is probably the best option.5
Although typically benign in nature, DPL may degenerate into malignancy.2 Therefore, regular follow-up is strongly recommended, especially for high-risk patients.11















