Case Presentation
A 49-year-old woman with history of bicytopenia (anemia and leukopenia) and monoclonal gammopathy (IgG
lambda) not fully clarified presents with portal hypertension and splenomegaly of unclear cause. Abdominal computed tomography (CT) and magnetic resonance imaging (MRI) were performed for further investigation.
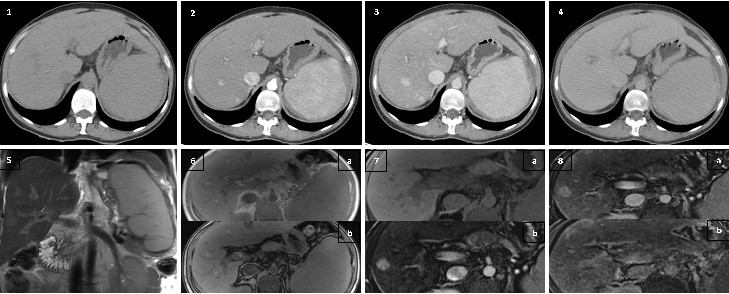
Figure 1: 1. Axial non-enhanced CT revealed no focal nodular lesions; 2. Axial contrast-enhanced CT (hepatic arterial phase) showing small hypervas- cular nodules (arrows); 3. Axial contrast-enhanced CT (portal-venous phase) showing small hypervascular nodules (arrows); 4. Axial contrast-enhanced CT (delayed phase) with no signs of washout; 5. Coronal T2-weighted MRI showing a nodule slightly hyperintense (arrow); 6. Axial T1-weighted gradient echo in-phase (a) and out-of-phase (b) MRI revealing isointense nodule without drop of signal (*); 7. (a) Axial unenhanced T1-weighted MRI showing isodense nodule (*); (b) Axial T1-weighted fat-saturated MRI after enhancement with gadoxetic acid (hepatic arterial phase) showing hyper- vascular nodule (arrow); 8. (a) Axial T1-weighted fat-saturated MRI after enhancement with gadoxetic acid (portal-venous phase) showing hypervascu- lar nodule (arrow); (b) Axial T1-weighted fat-saturated MRI after enhancement with gadoxetic acid (hepatobiliary phase) showing isodense nodule after 20 minutes delay (*).
The CT scan revealed multiple hyperdense nodular areas in both arterial and portal-venous phases, of variable sizes, with the largest one measuring 1,5cm. The lesions showed no signs of washout (Fig. 1(1,2,3,4). On MRI the lesions were slightly hyperintense on T2-weighted images (Fig. 1(5) and isointense on T1-weighted images (Fig. 1(7a)), showed no restriction on diffusion-weighted images or drop of signal intensity between in-phase and out-of-phase sequences (Fig. 1 (6)). Dynamic post-gadoxetic acid MRI revealed hepatic lesions with overlapping characteristics (hyperintense in arterial - Fig. 1 (7b) - and portal-venous - Fig. 1 (8a) - phases and isointense in delayed phases - Fig. 1 (8b)). The liver was enlarged with irregular contours suggesting chronic liver disease. There were signs of portal hypertension, namely contrast enhancement of paraumbilical vein, homogeneous splenomegaly (15cm) and ascites. No other focal lesions were identified in the spleen, kidneys or paravertebral region.
The liver lesions were considered dysplastic nodules - Liver Imaging Reporting and Data System (LI-RADS) 3 (intermediate probability for hepatocellular carcinoma). Further differential diagnosis including adenomas, focal nodular hyperplasia (FNH) and hemangiomas were not favored in the setting of cirrhotic liver. Hypervascular metastases or other atypical lesions were considered less likely based on imaging findings. The past medical history and the laboratory investigation did not reveal a cause for chronic liver disease. At this stage, the patient was diagnosed with cirrhosis, Child-Pugh score B (7 points) and Sodium Model for End-stage Liver Disease (MEDLD-Na) 11 points. After admission with decompensated cirrhosis, the patient was proposed for liver transplantation.
The histopathological analysis of the liver revealed extensive and diffuse extramedullary hematopoiesis. There were no liver tumors and it was not possible to determine the etiology of cirrhosis.
Discussion
Extramedullary hematopoiesis (EMH) is a compensatory mechanism for maintaining erythrogenesis in response to abnormalities in the production of red blood cells (RBC), either in response to continued RBC destruction (e.g. sickle cell disease, thalassemia, spherocytosis) or inability of normal RBC precursor to produce cells (e.g. iron deficiency, pernicious anemia, myelofibrosis, leukemia, lymphoma, diffuse osseous metastases). After birth hematopoiesis occurs only in the bone marrow and in the fetus the main sites are the yolk sac, spleen and liver.1 In the adult areas of hematopoiesis may appear in the liver, spleen and lymph nodes, as in the early stages of life, probably arising from multipotent stem cells, and are always abnormal. Although, almost all body sites may be involved by EMH.2,3
EMH is generally seen in the paraspinal region of the thorax, in the liver or spleen. Chest involvement is well documented. It usually presents as paravertebral fat-containing masses, easy to diagnose in the appropriate clinical environment, such as myelofibrosis or hemolytic anemia.3 The liver and spleen are usually the EMH abdominal locations, most commonly with diffuse involvement that manifests as organomegaly. In rare cases, the involvement can manifest as focal lesions.1
Very few cases of focal intrahepatic EMH have been reported,2,3,4,5 making our diagnosis and the differentiation from other focal liver lesions difficult. In most reports EMH lesions appeared hypodense on unenhanced CT and hypointense on T1-weighted and slightly hyperintense on T2-weighted images.1,4 In post-contrast scans, the lesions were described as nonenhancing or heterogeneously enhancing on both CT and MRI. Contrary to most previous reports, in a few cases, as in our case, the lesions exhibited homogenous enhancement in both arterial and portal-venous phases.5 We cannot exactly explain the discrepancy in the enhancement pattern of liver lesions. Although it cannot be directly related, it is reported that paraspinal EMH masses with homogeneous enhancement represent active EMH and masses with inhomogeneous enhancement represent non-active lesions.1
In the context of cirrhotic liver, hypervascular lesions are suspicious for hepatocellular carcinoma. In our case the lesions did not have typical characteristics, with no washout in delayed images. Adenomas and HNF generally demonstrate arterial enhancement and are isointense in delayed phases; in the hepatobiliary phase, post-gadoxetic acid, the enhancement persists in HNF and shows decreased signal intensity in adenomas. Hemangiomas normally “fill in” on delayed scans. Hypervascular metastases are usually hypointense in T1-weighted and moderately hyperintense in T2-weighted images. In addition, metastases are less likely in a cirrhotic liver.
When the diagnosis is uncertain, biopsy is considered. Regarding EMH, thoughtful consideration should be given to biopsy technique, as the lesions can be highly vascular and prone to hemorrhage.1
This report describes a rare case of focal intrahepatic EMH in a patient with liver cirrhosis. Considering the rarity of the EMH disease entity, this diagnosis was not included in the initial differential list of hypervascular hepatic lesions. Our case highlights the importance of the clinical setting and we believe that this diagnosis should be considered in patients with underlying hematological disorder.














