Case presentation
We present a 78-years-old male patient with a normal digital rectal exame, showing progressive PSA elevation (currently 14.2 ng/ml). The patient had previously performed ultrasound guided biopsy (TRUS) with negative results. He was then referred to JCC - Hospital Particular de Viana do Castelo to undergo a prostate MRI scan (3T) and subsequent MRI guided biopsy (in-bore system).
On T2 weighted imaging we could depict a nodular hypointense lesion with 10 mm of greater diameter, in the anterior gland, at the apex level (Figure 1). The lesion showed restricted diffusion (b 1600) (Figure 2) and reduced ADC value (Figure 3). It was classified PI-RADS 4 (PI-RADS 2.1).
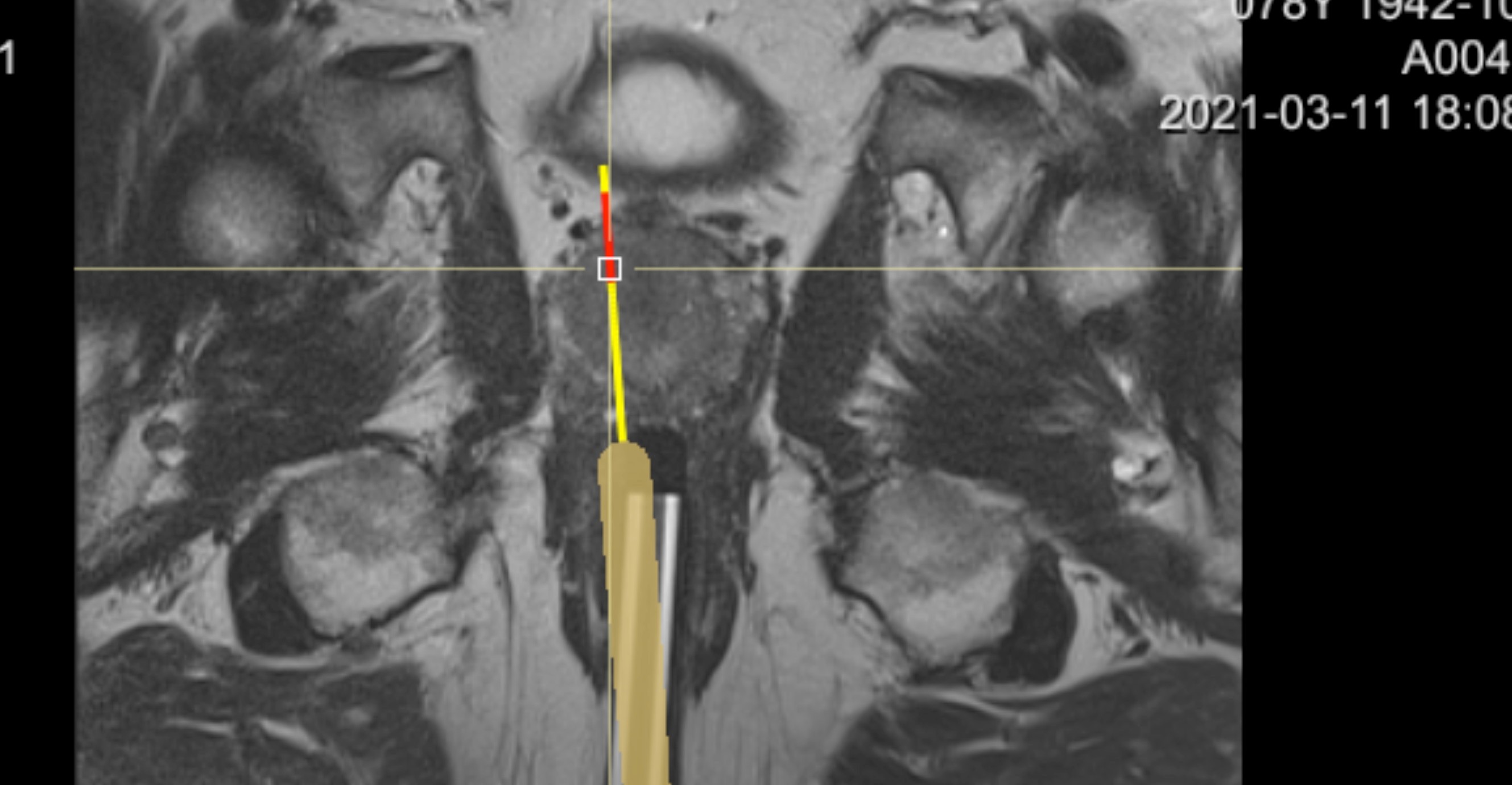
The patient was then submitted to MRI guided biopsy (in- bore system), and two samples of the lesion were taken (Figure 4). The histology proved the presence of clinical significant prostate cancer PCa (Gleason 3+4).
Discussion
MRI guided in-bore biopsy is a target biopsy method that enables a real-time feedback with needle placement, allowing better accuracy with fewer samples, providing higher rates of cancer detection.(1,2) Although TRUS remains the gold standard method for primary PcA diagnosis, about 20% of the lesions remain undiagnosed in the first biopsy, specially those with anterior and appical location which are almost inaccessible by this method.(3)
Several studies have been demonstrating the better outcome of MRI guided biopsies in the detection of Pca with anterior and central glandular location(4) and currently, the European Association of Urology recommends this procedure in men with clinical suspition of PCa and a first negative TRUS biopsy. Studies have also been showing other advantages of MRI guided biopsy over a second TRUS biopsy, such as the lower probability of detecting low risk Pca (not clinical significant) reducing overtreatment, and therefore reducing costs and improving patients’ quality of life.(2)
More studies are needed to access the role of MRI in-bore biopsy as a first-line diagnostic tool.