Case presentation
A 78-year-old male with a medical history of laryngeal squamous cell carcinoma, cT4aN1M0 stage treated with radiotherapy, was referred to the emergency department of our institution due to exacerbated dyspnea, prompting the placement of a tracheostomy. In this setting, he underwent a contrast-enhanced computerized tomography (CT) which revealed diffuse soft-tissue post radiotherapy edema of the neck resulting in upper airway obstruction. Neither signs of locoregional recurrence nor significant pulmonary abnormalities were noted. However, a slightly enhancing oval and well circumscribed soft-tissue nodule was noted on the left breast measuring 25 mm (Fig. 1). It was considered indeterminate and further breast imaging evaluation was recommended.
The patient had a history of smoking and alcohol consumption. Besides bilateral breast enlargement due to gynecomastia, the patient had no breast pain nor nipple discharge. He denied family history of breast or ovarian cancer. On clinical examination, a small, soft and slightly mobile nodule was palpable in the upper outer quadrant of the left breast. The nodule was not attached to the chest wall. The mammogram revealed a well-defined hyperdense nodule in the left upper outer quadrant without microcalcifications or spiculations along with bilateral gynecomastia (Fig. 2A). The lesion appeared on ultrasound as an oval hypoechoic and slightly heterogeneous lesion with smooth margins and no posterior shadowing measuring 26 mm (Fig. 2B). There was no axillary lymphadenopathy. The imaging findings were consistent with a BI-RADS 4 score and an ultrasound-guided needle-core biopsy was performed. The histopathologic examination of the lesion was compatible with a cavernous hemangioma of the sinusoidal type (Fig. 3). The lesion remained stable after a 12-month follow-up.
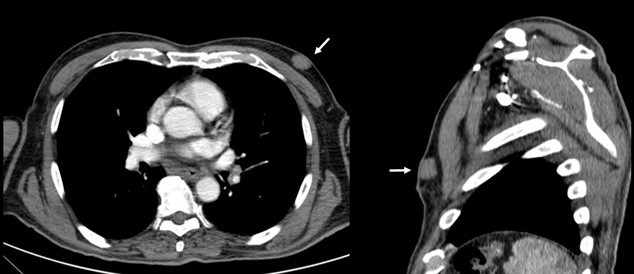
Figure 1: Contrast-enhanced chest CT showing a well-circumscribed, slightly enhancing, and homogeneous mass located in the upper outer quadrant of the left breast (white arrow).
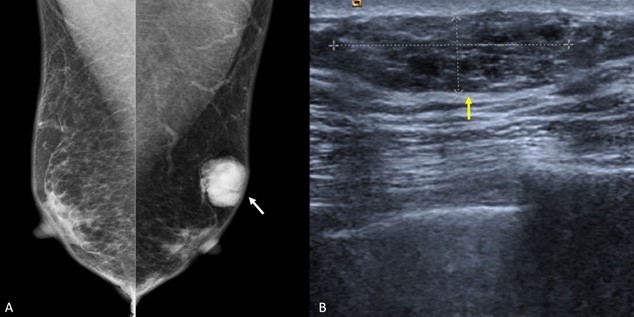
Figure 2: Mediolateral oblique views of the mammogram revealing bilateral gynecomastia and a well circumscribed and lobulated dense mass located at the upper outer quadrant of the left breast, without spiculations, calcifications, or skin retraction (A, white arrow). Left breast ultrasound images demonstrating a 26 mm oval solid mass with well-circumscribed margins and parallel orientation with slightly complex echotexture but without posterior acoustic shadowing (B, yellow arrow).
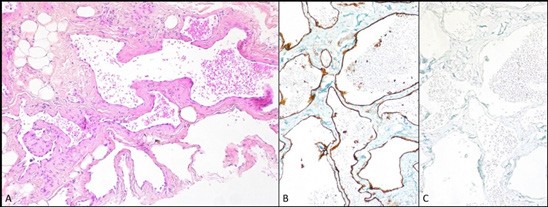
Figure 3: Hemangioma (A - hematoxylin-eosin, x100; B/C - CD31/Podoplanin, x100). The lesion was composed of thin-walled cavernous vessels that interconnect in a sinusoidal pattern (A). These vessels are lined by bland endothelial cells with no cytological atypia. The cells showed immunoreactivity for CD31 (B) and negativity for Podoplanin (C).
Discussion
Hemangiomas are benign vascular tumors that rarely develop in the breast. Perilobular hemangiomas are benign and microscopic lesions without clinical significance, generally smaller than 2 mm (not apparent on mammography).(1,2,3,4) Breast hemangiomas that are clinically and/or mammographically detectable are classified into cavernous, capillary, complex or venous types, depending on the size of their vascular channels. The cavernous type hemangioma is the most frequently encountered.
In a previous study comprising 1362 patients of both genders treated with lumpectomy, simple mastectomy or modified radical mastectomy for various primary breasts tumors, only 12 cases of hemangiomas were found (11 women and one man; 0,8% of total breast lesions).(4) As the number of male patients enrolled in the study population was not specified, the real incidence of male breast hemangiomas remains unclear. Although imaging features of breast hemangiomas are well described in women, male breast hemangiomas are exceptionally rare and only few cases have been previously reported.
Breast hemangiomas tend to be larger in men (mean diameter of 5.4 cm) than in women (mean diameter of 1.1 cm).(5) Apart from size, the other radiologic features of male breast hemangiomas show no differences from those reported in women.(5,6,7,8) Breast hemangiomas usually appear as superficial, oval and well circumscribed nodules or masses and, in some cases, can be slightly lobulated. They commonly have a density similar to that of fibroglandular breast tissue in mammograms and lack spiculations.(5,6,7,8) Although uncommon, cases presenting with fine or coarse calcifications have been reported.(9) Variable echo patterns are seen on ultrasound. Around one-third of hemangiomas exhibit hyperechoic echotexture and the remaining may show an isoechoic, hypoechoic or a complex echo pattern. A common feature is the absence of a posterior acoustic shadow.(6,7,10) Vascular poles may be seen with Doppler ultrasound.(10) Magnetic Resonance Imaging (MRI) usually demonstrates a lesion isointense to the surrounding fibroglandular tissue on T1-weighted images and hyperintense on T2-weighted images.(7) Peripheral arterial enhancement and delayed central enhancement may be seen on contrast-enhanced images - a useful imaging feature that may aid in differentiating it from malignant tumors.(7)
The differential diagnosis of breast hemangiomas in men is broad but should include angiosarcoma, metastasis (particularly in patients with a known primary cancer), breast cancer and pseudoangiomatous stromal hyperplasia (PASH).(9,10,11,12,13)
Angiosarcoma, although extremely rare, is considered the main differential diagnosis since this vascular malignant tumor frequently mimics the imaging appearance of a breast hemangioma on mammography and ultrasound.(6) MRI may provide some helpful clues in some cases. Indeed, high-grade angiosarcomas tend to present rapid enhancement and washout with frequent visualization of large draining vessels and multiple unenhanced areas within the tumor.(11) However, histopathologic analysis remains mandatory for correct diagnosis. Microscopically, both can be composed of thin-walled capillaries lined by low nuclear grade endothelial cells and both are typically positive for vascular markers such as CD31 and CD34 but negative for lymphatic endothelium marker, podoplanin.(8) However, angiosarcomas are positive for the S-phase kinase-associated protein 2, show a higher Ki-67 proliferation index and other features of architectural and/or cytological atypia normally absent in breast hemangiomas, as well as a frequent previous history of chest irradiation, usually in the context of breast cancer treatment. In contrast to angiosarcomas, hemangiomas also usually present well-circumscribed vascular channels surrounding the ducts and lobules rather than invading them.(8) Currently, it is considered that with clinical, radiologic and pathologic correlation, core needle biopsies allow for a reliable histopathological diagnosis. Thus, further surgical excision is no longer mandatory and a follow-up may be preferred, especially in the case of frail patients that would not be good candidates for surgery,(11) such as ours.
Metastases to the breast are extremely rare, representing 0.5%-3% of all malignant breast tumors concerning both genders.(8) The most common primary malignancies that metastasize to the breast are melanoma, non-Hodgkin’s lymphoma, and carcinomas of the lung, stomach, kidneys, prostate and ovaries.(8) Breast metastasis from squamous cell carcinoma from the head and neck is highly uncommon, with only a few cases reported.(14) Hematogeneous breast metastases are frequently multiple or bilateral round masses with circumscribed or microlobulated margins and no associated calcifications on mammography.(8,13) Nevertheless, single irregular masses with spiculated margins and calcifications may also occur.(15) Posterior acoustic enhancement is a common finding on ultrasound, with variable vascularity on Colour Doppler.(15) Metastatic lesions are typically isointense on MRI in both T1 and T2-weighted images, with homogeneous enhancement on post-contrast images.(15) Lymphatic spread presents as diffuse oedema with skin and trabecular thickening and is commonly accompanied by pathologic axillary lymph nodes.(8,13,15)
Male breast cancer is rare, accounting for <1% of male cancers and <1% of all breast cancers.(13) Invasive breast carcinoma of no special type (NST) is the most frequent histological type.(8,13) As no cancer screening program exists for men, male breast cancer is frequently diagnosed at an advanced stage.(13) Contrary to breast hemangiomas, breast male cancers usually present with suspicious imaging features such as irregular, spiculated or indistinct margins on both mammography and ultrasound, and they are frequently located in the subareolar region or eccentric to the nipple.(8,13) Contrary to women, the concept of benign calcifications does not apply to a male breast mass and should always be considered suspicious for breast cancer.(14) PASH is a frequent benign entity (found in 50 % of male breast biopsies) consisting of a hormonally-dependent proliferation of fibroblasts and myofibroblasts, being highly associated with gynecomastia.(8,13) Although variable, the most common imaging finding is a non-calcified oval, circumscribed mass at mammography and an ovoid homogenously hypoechoic mass at ultrasound.(8,13) Hemangiomas are extremely rare and benign in male breasts but share similar imaging features with those appearing in women. While ultrasound and MRI may provide useful clues that aid in the differential diagnosis, a histopathological examination remains mandatory for proper diagnosis and management.















