Case Presentation
A 68-year-old woman with a history of arterial hypertension and Gilbert´s syndrome was referred to a Gastroenterology consultation due to adenomyomatosis of the gallbladder. Additionally, laboratory results reveal elevated transaminase levels. An abdominal CT was
initially performed and revealed a homogeneous soft tissue nodule with a flat-ovoid shape and ill-defined microlobulated margins located in the wall of the second part of the duodenum, measuring 22 x 17 mm (figure 1A), with avid homogeneous enhancement after intravenous contrast material administration, on arterial (figure 1B) and venous phases (figure 1C).

Figure 1: Axial soft tissue window, 2.5 mm slice thickness, non-enhanced CT (A), contrast-enhanced CT in arterial phase (B) and portal venous phase (C). The arrow points to the lesion.

Figure 2: A- Axial T2 haste image; B- Diffusion weighted sequence on b700 image (DWI); C- Apparent diffusion coefficient map (ADC). The arrow points to the lesion.
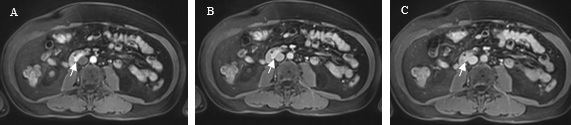
Figure 3: Axial contrast-enhanced T1-weighted fat suppressed MRI in arterial (A), portal (B) and equilibrium phases (C). The arrow points to the lesion.
Then, the upper digestive endoscopy did not reveal any significant abnormality.
An abdominal MR was performed for further investigation of this lesion and showed the same solid intramural oval mass with T1 hyperintensity and intermediate signal in T2 (figure 2A), no restriction on diffusion-weighted imaging (DWI)) (figure 2B e C) and early avid enhancement after intravenous gadolinium-based contrast material administration (figure 3).
Subsequently, a PET scan did not reveal any hypermetabolic alteration suggestive of neoplastic lesions with a high metabolic rate, including at the duodenum.
Some diagnoses were included in the differential list: gastrointestinal stromal tumor (GIST), leiomyoma, gastrointestinal neuroendocrine tumour (gastrinoma or carcinoid tumour), ectopic pancreas or metastasis.
Due to a diagnostic dilemma, a surgical option was contemplated. Histological analyses of the dissected duodenal mass confirmed the diagnosis of ectopic pancreatic tissue located in the submucosal layer of the duodenum.
Discussion
Ectopic pancreas (EP) is a congenital anomaly in which pancreatic tissue is anatomically separate from the main gland, without vascular or ductal continuity. It is also referred to as heterotopic, aberrant or accessory pancreas, pancreatic choristoma or adenomyoma. The most common locations of this displacement include the upper gastrointestinal tract - the stomach (25-52%), duodenum (27-36%), and jejunum (15-17%). Less common sites include the ileum, esophagus and Meckel's diverticulum, but also occasionally in the mesentery, hepatobiliary system, spleen, lung, mediastinum and umbilical foramen.1,2,3It most frequently occurs in the submucosa (75%), but can also be present within the muscularis propria or the serosa.4
The true incidence of EP is difficult to determine, as most affected patients are asymptomatic. They are typically discovered incidentally during surgery or autopsy with an incidence at upper abdominal surgeries of 0.2% and 0.9% at gastrectomies. Autopsy results reveal the incidence of EP to be 0.5-13.7% approximately.1,2
Nevertheless, the same pathology that affects the normal gland may also be seen at this ectopic site. Some patients with this condition develop complications such as pancreatitis, insulinoma, pseudocyst and pancreatic cancer, which cause clinical symptoms such as abdominal pain, obstruction and gastrointestinal bleeding.3
The disease is most often seen in males, and the incidence peaks in the 4th, 5th and 6th decades of life.2
However, many patients are misdiagnosed at the time of surgery or are thought to have other pathological changes. Zhang et al. reported that over 54% of patients with EP were misdiagnosed preoperatively.5
Ectopic pancreas is essentially analogous to the normal pancreas in terms of gross and histological specimen. It typically appears as a solid intramural mass with a micro-lobulated border that is not clearly demarcated from the surrounding tissues. EP is mostly solitary (80%), and its diameter is mostly less than 3 cm, but the size also varies from 0.2cm to 5.0cm.2
CT images show an intramural oval mass with ill-defined or microlobulated margins and an enhancement pattern similar to normal pancreas. They are usually small (<3 cm) and tend to exhibit an intraluminal growth pattern. The CT attenuation and enhancement characteristics of the lesion reflect its microscopic composition. Heterotopic tissue that is predominantly composed of acini shows homogeneous avid enhancement that is greater than or equal to that of the orthotopic pancreas. Hypoenhancing lesions are composed mostly of ductal structures and hyperplastic muscular layers.1,2
It is important to differentiate from the most common gastrointestinal submucosal tumors such as gastrointestinal stromal tumor (GIST) and leiomyoma. A flat shape, lobulated contour, and endoluminal growth are most indicative of ectopic pancreas.4
Kim, J.Y. et al described a list of CT findings that can differentiate EP from GIST and leiomyoma namely: the typical location (prepyloric antrum and duodenum), endoluminal growth pattern, ill-defined microlobulated margins, prominent enhancement of overlying mucosa, and a flat or ovoid shape with a long diameter-to-short diameter ratio higher than 1.4. The authors established that when at least two of these five criteria were present in combination, the sensitivity and specificity for diagnosing heterotopic pancreas were 100% and 82.5%, respectively. When four of these criteria were present, a sensitivity of 42.9% and a specificity of 100% were achieved.3
This case had three of these features: the location on the duodenum, the ill-defined borders and the flat-ovoid shape with a LD/SD ratio>1.4.
On MR, the appearance, enhancement degree and signal intensity of EP resembles that of the orthotopic pancreas in all sequences. EP shows characteristic discriminatory high signal on T1-weighted images and exhibits marked enhancement in the late arterial phase. Some EP may even display more pronounced enhancement than the normal pancreas. MR cholangiopancreatography (MRCP) plays an important auxiliary role in identifying the rudimentary ductal system. The dilated duct of EP, also known as the “heterotopic duct sign,” is more easily manifested on T2-weighted images and MRCP images, a specific sign that helps to distinguish EP from other submucosal lesions and may preclude the need for surgical excision to establish a definitive diagnosis.2,6
However, in our case, the presence of ducts within the tissue was not evident.
In conclusion, although ectopic pancreas is rare, it should be always considered in the differential diagnosis of extramucosal duodenal lesions. Despite the development of modern diagnostic modalities, its recognition remains challenging and the preoperative diagnosis has traditionally not been accurate. Surgical excision is recommended especially if diagnostic uncertainty remains.















