A 12 month-old male infant was referred to the paediatric pulmonary unit of our tertiary hospital for further investigation.
At the age of 4 months-old, he had been referred by his family doctor to a secondary hospital because of respiratory distress since the first month of life and failure to thrive. At that time, clinical observation revealed an increase in the anteroposterior diameter of the chest, elevated respiratory rate, and subcostal and supraclavicular retractions. On auscultation, crackles were heard in both lung bases without wheezing. Peripheral blood oxygen saturation was 92% in room air. Laboratory investigations, which included alpha-1 antitrypsin levels and sweat test, were within in the normal range. Chest x-ray (not shown) revealed bilateral lung hyperinflation and no further remarks. He was treated with supplemental oxygen and inhaled corticoids with mild clinical improvement.
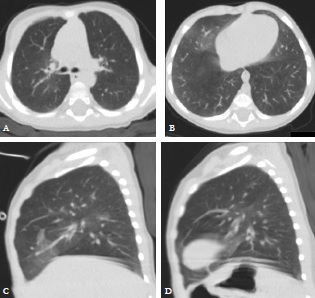
A high-resolution chest computed tomography (CT) was performed at our department.(Fig. 1)
Chest CT revealed bilateral ground glass opacifications, centrally located and most prominent in middle lobe and lingula, with no other airway or parenchymal abnormalities. These features were highly suggestive of neuroendocrine cell hyperplasia of infancy (NEHI). The patient needed supplemental oxygen till 27 months old and he has been asymptomatic since then. Years later, a follow up CT confirmed nearly complete resolution of lung opacifications. These findings are consistent with the diagnosis of NEHI.
NEHI, originally known as persistent tachypnea of infancy, is a rare form of children interstitial lung disease (ChILD) involving the small airways and was first described in 2005 by Deterding.1 Its name was given by the characteristically histological findings at lung biopsy showing increased bombesin-immunopositive pulmonary neuroendocrine cells in a normal lung structure.1
NEHI typically presents in full-term infants within the first year of life with tachypnea, chest wall retractions and hypoxemia, with no significant cough, and associated with failure to thrive.1,2,3,4 Auscultation can be normal or reveal scattered crackles without wheezing.1,3 Chest radiographs are nonspecific and often may suggest viral airway disease.5 On the other hand, high-resolution CT findings are distinctive.6 The characteristic imaging pattern in NEHI patients was described by Brody et al. and include geographic central ground-glass opacity in the right middle lobe and lingula, and diffuse air trapping in a mosaic attenuation pattern, without other airway or parenchymal abnormalities.5
High-resolution CT is the most reliable noninvasive imaging test that can point to the diagnosis of NEHI and allows differentiation from other types of interstitial lung disease with a sensitivity and specificity of at least 78% and 100%, respectively.6 Based upon these data, presently, the consensus is that the typical clinical and chest CT findings are sufficient for diagnostic purposes,7 without the need for a lung biopsy,8,9 thus the importance for the paediatricians and radiologists to be aware of this condition. The most important high-resolution CT findings to correctly diagnose NEHI are ground glass opacities involving at least four lobes, confined to the middle lobe, the lingula, and the parahilar and paramediastinal distributions.6,9 Ground-glass opacities in other locations and other findings, such as, pleural effusion, bronchial wall thickening, bronchiectasis, architectural distortion, honeycombing, interlobular thickening, focal consolidation, and parenchymal cysts, are considered atypical.9
NEHI is unresponsive to steroids and treatment is largely supportive and focused on preventing hypoxemia with supplemental oxygen.1,8 Long-term outcomes have been excellent with no reported deaths.1,4,5,9