Case Presentation
An asymptomatic 62-year-old male with obesity, hypertension, dyslipidemia, and diabetes was referred to an endocrinology consultation. The patient had a history of right adrenal carcinoma (11cm), diagnosed and resected 18-years before (first presenting as adrenal insufficiency and shock), and currently not undergoing follow-up. The clinical picture was otherwise irrelevant, and an abdominal MRI was requested by the endocrinologist.
The MRI (Fig.1) uncovered an incidental 7cm retroperitoneal mass, in the left perirenal space, partially circumscribed and heterogeneous. The mass had a small macroscopic fat component, as well as a bigger component with intermediate signal on T2-weighting, loss of signal in T1-out-of-phase, and contrast uptake. The left adrenal gland presented no abnormal findings. The right adrenal gland was absent (consistent with prior surgery) with no signs of local recurrence.
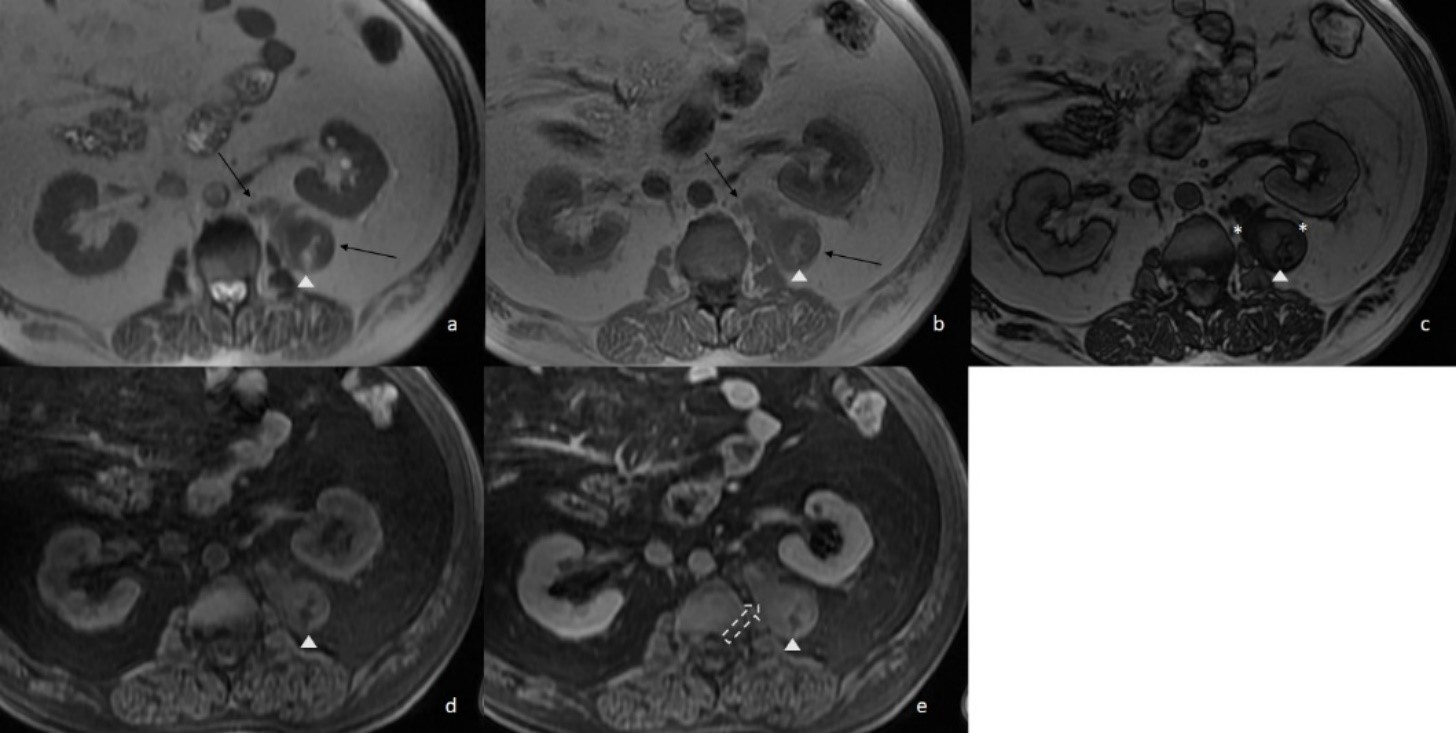
Figure 1: Perirenal Extra-adrenal Myelolipoma. T2FSE (a) and T1GRE in-phase (b) show a lobulated circumscribed mass at the left perirenal space, medially to the kidney, composed of a larger isointense component (arrows) and a hyperintense peripheral component (arrowhead). At T1GRE out-of-phase (c) there is signal loss across the isointense component (*) - suggestive of microscopic fat - and india ink artifact surrounding the hyperintense component. T1 Fat Saturated sequences before (d) and after (e) i.v. contrast administration, confirm the presence of macroscopic fat (arrowhead) and demonstrate mild enhancement of the solid component (dotted arrow). Percutaneous biopsy was compatible with myelolipoma.
A percutaneous biopsy was performed and was compatible with myelolipoma.
A conservative approach was initially adopted, and the patient began annual imaging follow-up, first with MRI and then with CT. At two-year follow-up, the CT results evidenced that the mass had grown to measure 9cm (Fig.2). It did not invade adjacent structures and was made of a hazy fat component and a nodular soft tissue component. There were no calcifications or hemorrhage.
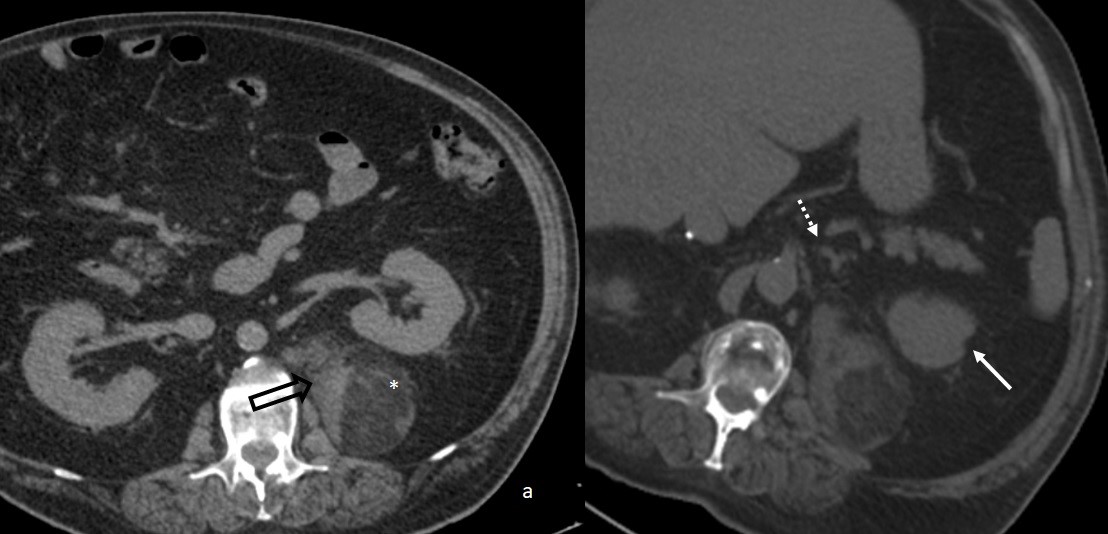
Figure 2: Extra-adrenal Myelolipoma Follow-up with CT after two years. An abdominal CT without i.v. contrast (a) shows the retroperitoneal mass and both soft tissue (arrow) and hazy macroscopic fat components (*); the mass had grown 2cm in the 2-year interval and had a more prominent fat element in relation to the previous MRI. A CT reformation (b) demonstrates the relationship of the mass with surrounding structures, namely the left adrenal gland (dotted arrow) and the left kidney (arrow).
Surgical resection was performed, due to continuous 2cm growth and fear for acute hemorrhage or coexisting malignancy. Giving the technical aspects of the surgery, the left kidney and adrenal gland were also excised, thus causing a lack of endogenous adrenal hormonal production and a consequent lifetime need of hormonal replacement.
Pathology confirmed the diagnosis of extra-adrenal myelolipoma (EAMLP) (Fig. 3). There are no signs of recurrence after a 2-year follow-up.
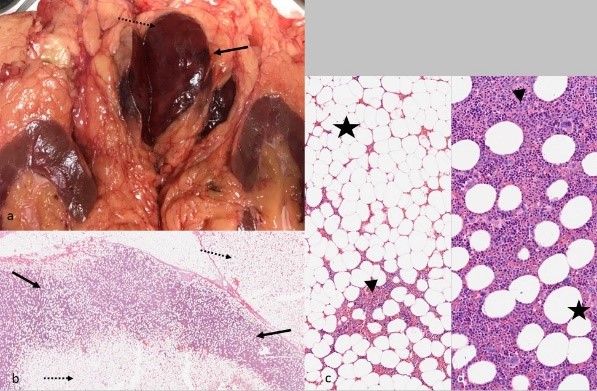
Figure 3: Extra-adrenal myelolipoma pathology. Gross pathology (a) shows a gray-brown capsulated lesion centered on perirenal fat tissue. At microscopy with low magnification (b) the tumor is shown to have dark stained areas (arrows) and light stained areas (dotted arrows). At high magnification (c, d) the lesion is shown to be composed of hematopoietic cells (arrowhead) admixed with mature adipocytes (star). Note the variable distribution of fat and hematopoietic elements across the lesion, contributing to low magnification (b) and gross pathology features (a).
Discussion
We present an EAMLP in a perirenal location detected incidentally on MRI in an asymptomatic patient, a rare case with typical radiological and anatomopathological features.
Myelolipomas are non-functional benign tumors, composed of adipocytes and hematopoietic cells. They have no malignant potential, despite their ability to reach larger sizes (over 30cm in some cases).1 Myelolipomas primarily occur in the adrenal gland (3-7% of all adrenal tumors),2,3but have also been described at several extra-adrenal locations,4,5most frequently the retroperitoneum, particularly the presacral region.6 Although they are typically solitary lesions, there are several case reports of multifocal disease.1 EAMLPs are rare, but their true frequency is unknown, as literature on the subject is mostly reliant on case reports.4 To our knowledge, the only data on EAMLPs’ relative frequency come from a series of myelolipoma cases submitted to the Armed Forces Institute of Pathology (1981-1997), in which 16% of all myelolipomas were extra-adrenal;6,7however, due to selection bias, there is likely an overrepresentation of the rarest types in this case series. EAMLPs have a slight female predominance and normally present at 50-70 years old.8
Myelolipomas etiology is not well established. They have been associated with increased adrenocorticotropic hormone concentrations (e.g.: Cushing syndrome, 21-hydroxylase deficiency, adrenal adenoma), or conditions like infection, stress, obesity, hypertension, and diabetes.1,2Current hypothesis suggests EAMLPs result from metaplasia of displaced adrenal cortical cells, embolization of bone marrow tissue, or metaplasia of fetal bone marrow remnants under pathological stresses.5,8
Our case is significant as it establishes a circumstantial association between an EAMLP and a previous contralateral adrenal carcinoma. The transient acute adrenal insufficiency and shock at the time of the carcinoma diagnosis imply adrenal hormonal dysregulation, probably preceding the development of the EAMLP; unfortunately, past medical records were unavailable. Of note, our patient’s metabolic and cardiovascular comorbidities (i.e., diabetes, dyslipidemia, hypertension, obesity) might have also been implied in his myelolipoma’s development.
In most cases, EAMLP diagnosis is incidental, as the patients are usually asymptomatic.9 Nonetheless, depending on the size and location of the lesion, some individuals may present with vague flank or abdominal pain due to hemorrhage, mechanical compression, or tumor infarction.5,9
On pathological examination, myelolipomas are well circumscribed and heterogenous masses, with variable amounts of mature adipose tissue admixed with an extramedullary trilinear hematopoiesis.2 Occasionally, areas of degeneration (hemorrhage and calcifications) are also seen.4
Imaging features of EAMLPs are analogue to adrenal myelolipomas.6 The masses are typically well-circumscribed and may displace surrounding structures, but do not invade them.9 The proportion and distribution of myeloid and fat along the lesions is variable and influences cross-sectional imaging findings.6,7,10
On CT, the myeloid elements are represented by enhancing areas of soft tissue attenuation (homogenous cloudy pattern, solid strands appearance or solid nodule within the fat) with a variable, but generally low, mean density (20-30 H).2 In opposition, density of the macroscopic fat component is usually higher than that of retroperitoneal fat.7,10,11A minority of myelolipomas contains little fat tissue, not clearly visualized on CT.1
On MRI, hematopoietic elements have low-to-intermediate signal on T1 and intermediate-to-high signal on T2-weighted images, enhancing after i.v. contrast administration.10 Macroscopic fat has high T1 and T2 intensity, and loses signal on fat suppressing sequences. Characteristically, myelolipomas have microscopic fat within the myeloid component, identifiable by signal loss on T1 opposed-phased sequences, that corresponds to small foci of adipocytes.12,13
Hemorrhage and small calcifications are not uncommon and are more readily noticed on CT.9,11Scintigraphy with 99mTc sulfur colloid can detect erythroid cells in myelolipomas.9
A well-defined adrenal mass, containing mainly macroscopic fat, is characteristic and almost pathognomonic of myelolipomas.2,13A fatty mass within the retroperitoneal space represents a diagnostic challenge. Differential diagnosis includes extramedullary hematopoiesis, exophytic angiomyolipoma, retroperitoneal teratoma and liposarcoma.8 In our case, a primary exophytic adrenal neoplasm (adrenal carcinoma, pheochromocytoma) was also considered, due to the patient’s history and lesion location.
Mass-forming extramedullary hematopoiesis is difficult to differentiate from a myelolipoma solely based on imaging, but history of an underlying hematologic disorder helps in the differentiation. Patients with extramedullary hematopoiesis may have hepatosplenomegaly, and the disease may involve multiple sites, especially the mediastinum and paravertebral regions. Extramedullary hematopoiesis can present at any age and is more commonly diagnosed in men.9
Contrary to myelolipomas, teratomas usually occur in younger individuals and contain fluid-filled cystic components.4
Lipomas or liposarcomas can be encountered virtually anywhere in the body, at any age. Retroperitoneal liposarcomas can be asymptomatic and commonly occur in older patients (in the 5th-7th decades of life). Lipomas and liposarcoma may have areas of soft tissue attenuation. A predominant soft-tissue component, with adjacent organ invasion, should raise suspicion of a possible liposarcoma.11
Adrenal carcinomas may invade adjacent structures, the tumors tend to be large, lobulated, heterogenous (hemorrhage and necrosis) and have irregular margins; adrenal adenomas are homogenous and well-circumscribed masses and may be lipid rich (<10 HU) or lipid poor (>10HU); pheochromocytomas are usually large, heterogeneous masses with avid enhancement.14 Macroscopic fat on imaging is uncommon in adrenal adenomas, and very rare in adrenal cortical carcinomas and pheochromocytomas; moreover, the fat content in these lesions is normally small and not dominant.13
Despite advances made in imaging techniques, it is still difficult to diagnose an EAMLP based solely on radiological techniques, and pathology remains the gold standard diagnostic method.5
Giving their rarity, no management guidelines are established for EAMLPs, and treatment is either observational or surgical.5 Generally, surgery is indicated in symptomatic cases and/or larger mass size, which is correlated with bleeding risk.2,5Surgery may also be employed to reach a definitive diagnosis and/or when malignancy cannot be excluded. If the patient is asymptomatic and the mass is small, the lesion can be handled in a conservative fashion. When surgery is performed, follow-up is optional because surgery is curative.1
Conclusion
Myelolipomas are benign tumors, with no reported risk of malignant degeneration. Extra-adrenal myelolipomas are rare and can be a source of confusion because their imaging features overlap with other tumors containing fat. Imaging findings (such as a well-circumscribed mass without invasion of adjacent structures) and clinical features (including age, adrenocorticotropic hormonal excess and lack of coinciding hematologic disease) are helpful to exclude other neoplasms and may be suggestive of myelolipoma. Ultimately, pathology remains the diagnostic gold standard.















