A term neonate born through meconium-stained amni- otic fluid from instrumented delivery, (Apgar score 7/8), without need for resuscitation, presents with grunting, cyanosis and respiratory distress by the 5th minute of life, with pulse oximetry revealing a 70%-75% saturation which resolved with oxygenotherapy.
The neonate was admitted to the neonatal intensive care unit (NICU), requiring oxygenotherapy (maxi- mum FiO2 40%, incubator environmental servo-oxy- gen delivery) for a saturation >95%. Initial bloodwork included a venous blood gases analysis (pH 7.26, pCO2 49.9 mmHg, HCO3- 22.4 mmol/L, BE -4.7 mmol/L, lac- tate 4.3 mmol/L), non-elevated C-reactive protein and a normal hemogram.
A chest x-ray showed a small pneumothorax (left lung apex) and left hemithorax radiolucency (outlining the mediastinal structures) with extrapleural air sign, suggesting a large pneumomediastinum. On the right hemi- thorax, diffuse, asymmetric, patchy pulmonary opacities mixed with focal overinflation areas are suggestive of meconium aspiration syndrome (MAS) (Fig. 1).
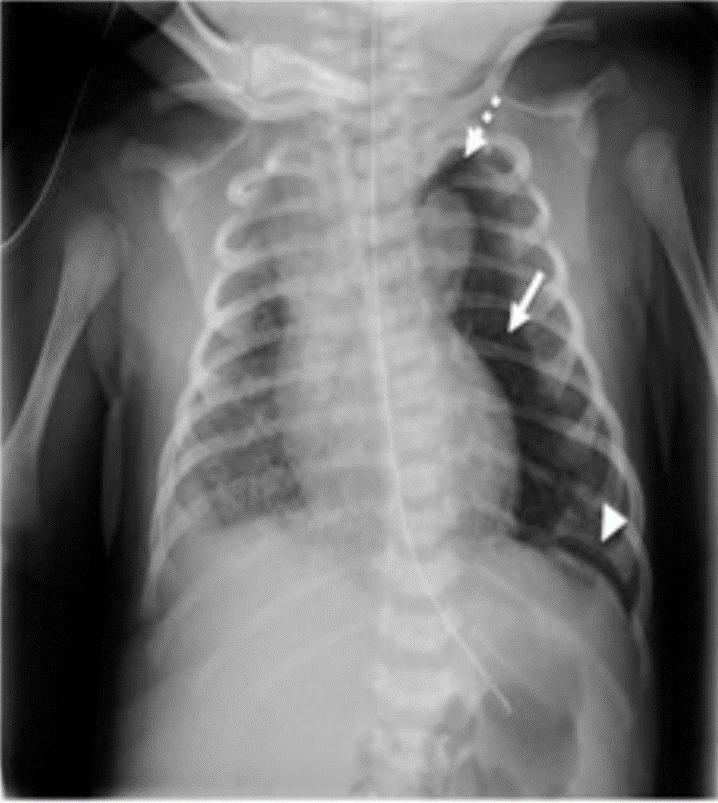
Figure 1: Chest x-ray at admission in NICU with a large pneumomediastinum (arrow) in the left hemithorax, with an extrapleural air sign (arrowhead) and a small linear pneumothorax (dotted arrow) on the left apex. Also visible are diffuse and asymmetric patchy opacities, mixed with focal areas of overinflation on the right pulmonary parenchyma, suggestive of MAS.
Oxygen was successfully weaned off, with no signs of respiratory distress by the second day. A subsequent chest x-ray on the sixth day, showed complete reabsorption of the pneumomediastinum and pneumothorax (Fig. 2), after which the neonate was discharged from the NICU.

Figure 2: Chest x-ray at sixth day of life showing complete reabsorption of the pneumomediastinum and pneumothorax.
Pneumomediastinum is uncommon in neonates (2.5:1000 live births) but should be kept in mind particularly in cases of preterm neonates, meconium aspiration, positive pressure ventilation or congenital pneumonia.1 Patients are usually asymptomatic, requiring no specific treatment, but should be monitored for evidence of cardio-respiratory compromise or development of other air leaks, especially pneumothorax. Infants with tension pneumomediastinum should be treated urgently with ultrasound-guided percutaneous drainage.
A chest x-ray should always be performed (lateral and anteroposterior views),2 although recent studies suggest a lung ultrasound can also help confirm the diagnosis.3
In the presence of a high index of suspicion, a correct and early diagnostic can prevent iatrogenic damage such as unnecessary insertion of a thoracic drain or prolonged antibiotherapy.















