Introduction
According to World Health Organization’s epidemiology data, at the time of writing (October 2021), there have been 240 million cumulative confirmed cases of coronavirus disease 2019 (COVID-19) worldwide. Loss of olfactory function represents one of the most frequent and earliest symptoms of COVID-19.1 A sudden and newly onset of olfactory dysfunction, even in the absence of other symptoms, is suggestive of COVID-19 infection, as it is considered a cardinal symptom of this disease.2-4
Olfactory dysfunction (OD) may occur in the presence of different entities, with viral infections (including those caused by influenza, parainfluenza, rhinovirus and coronavirus) being one of the most common causes.4,5 Due to the frequency of reported anosmia/hyposmia in the context of the increasing number of COVID-19 confirmed cases an increase is expected in the number of patients with OD over the next years, related to COVID-19.2,6
Anosmia is often devalued, trivialized and poorly understood by clinicians, probably because it is not considered a severe symptom, with the focus being placed on transmissibility and the possible organ impairment caused by COVID-19. Despite this, OD can have negative effects with impact on patients’ quality of life, especially concerning the role of smell in detecting warnings and hazards (gas leaks, spoiled food, chemicals), and its influence in many emotional and social problems.6-11
The incidence of OD after COVID-19 recovery (post-COVID-19-related OD) is highly variable in the literature, because anosmia is a symptom frequently reported as subjective and not objectively assessed.12 Although the majority of patients recover spontaneously, current published data suggest that up to 10% of patients may have persistent COVID-19-related OD.1,13,14 Bearing in mind that most patients will recover within the first 2 weeks after the onset of symptoms, we consider persistent post-COVID-19-related OD to be longer than 14 days. We will include in post-COVID-19-related OD all kinds of OD (hyposmia, anosmia, parosmia and phantosmia), whose definitions are explained in Table 1.
Based on these last treatments, we hope to provide, with this review, an evidence-based recommendation for the handling of COVID-19-recovered patients with persistent OD.
Methods
A literature review was performed in July 2021 through a research in two medical databases: PubMed® and Cochrane Library®. The authors searched for articles published between June 2011 and June 2021, using the following key terms: “anosmia”, “hyposmia”, “dysgeusia”, “olfactory dysfunction”, “SARS-CoV-2”, “COVID- 19”. In this review, randomized controlled trials (RCTs), cohort studies, and, since it is a very recent condition, preliminary results of ongoing research were included.
Articles were limited to those having titles and abstracts available in English or Portuguese. Also excluded were case reports, letters to the editor, and book chapters, as well as studies whose main focus was olfactory loss secondary to etiologies, not including post infectious olfactory dysfunction (PIOD).
All the authors agreed on the article selection, doing so independently, though Covidence® app.
After duplication, the identified full-text articles were examined for original data. Further cross screenings of the references were performed in order to complement the initial search results. Comparative studies examining the management of patients with post-viral olfactory outcome loss were included.
Olfactory Dysfunction in Covid-19
The mechanism behind COVID-19-related OD is not still well-understood, but it seems to behave differently from typical post infectious olfactory dysfunction (PIOD) cases, with a more pronounced olfactory dysfunction, and a frequent association with dysgeusia (specifically loss of bitter taste, which has been identified as a discriminating feature).9,15 Current investigation on the mechanism of chemosensory dysfunction in COVID-19 suggests that it is caused by the entry of the virus via angiotensin-converting enzyme 2 receptors, highly expressed on nasal epithelial cells, which leads to infection and death of sustentacular cells in the olfactory epithelium.9 In the majority of cases, this does not necessarily lead to permanent damage or death of olfactory receptor neurons and, therefore, patients usually recover within 4 weeks of onset.7,15 However, current data suggest that around 10% to 17% of patients have persistent OD and do not recover spontaneously.13,14 This OD persistence may be related to the ability of the coronavirus to affect a larger area of the olfactory epithelium, with possible cellular death of a larger number of olfactory receptor neurons. Nevertheless, further investigation is required to support this theory.7,9
Diagnostic Approach
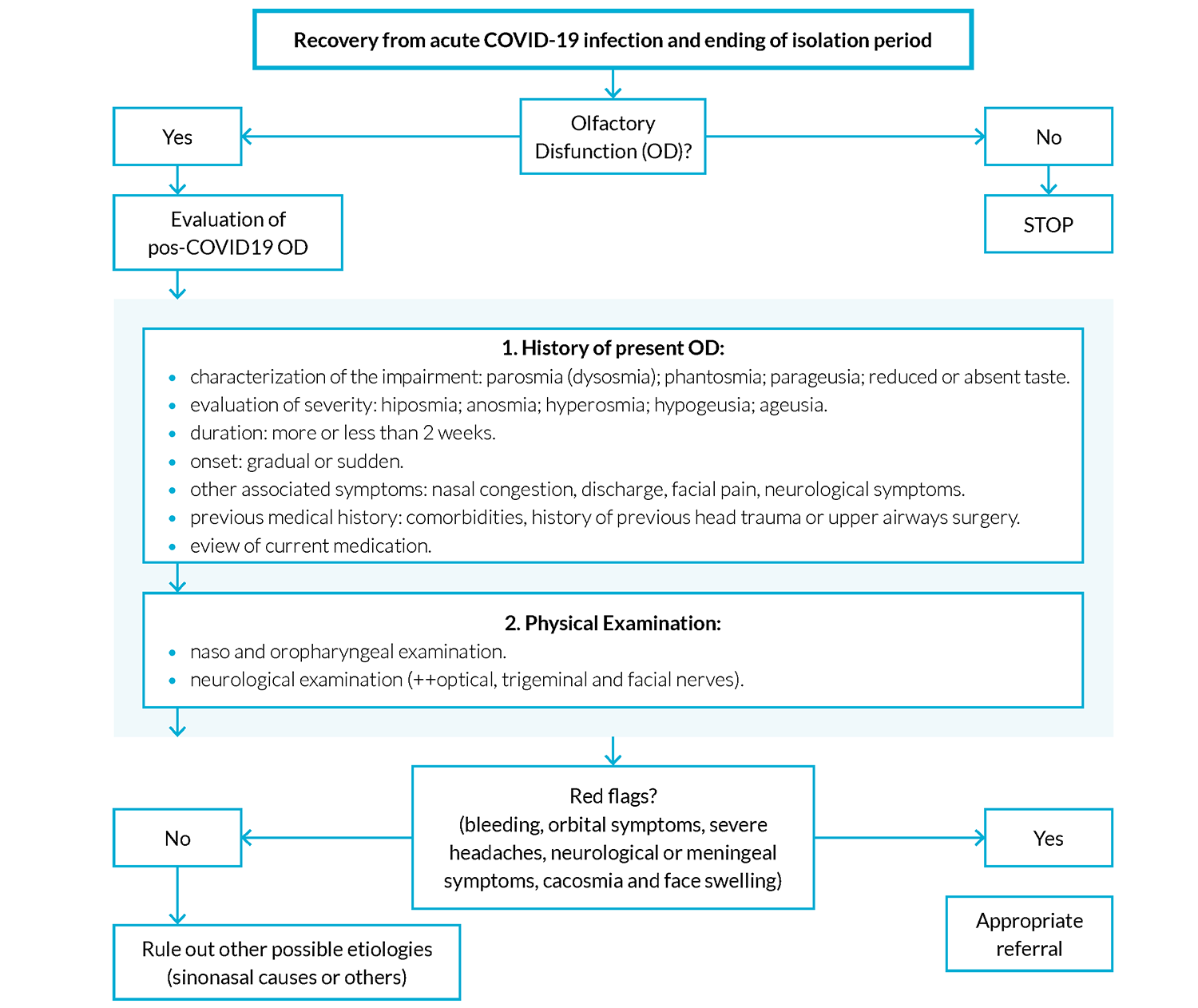
When a patient recovered from a COVID-19 infection presents with isolated OD for more than 14 days since the beginning of the infection, a detailed clinical history should be carried out.5,7,16 The goal is to identify possible red-flag symptoms and rule out differential diagnoses that may present with the same symptoms but require specific evaluation. Red flag symptoms that must be excluded comprise bleeding, orbital symptoms, severe headaches, neurological or meningeal symptoms, cacosmia and face swelling.
A possible approach to assessment is outlined in Fig. 1.
Clinical history is also important to evaluate the need for a second-level medical evaluation (otolaryngology).
The patient’s evaluation should focus on the correct symptom characterization: length, severity, coexistence of taste disturbance and presence of concomitant nasal discharge (mucous, purulent, cerebrospinal fluid).6,17
It is important to be acquainted with the previous medical history, including comorbidities, history of previous head trauma or upper airways surgery. Tobacco is a recognized irritant to the olfactory tract; therefore, the physician should question about the abuse of substances and the exposure to toxic agents.18,19
It is also important to review current medication, since OD can be a side effect of a wide variety of medications, especially antihypertensives, such as diuretics, calcium channel blockers, and statins.17
To rule out other etiologies, we need to assess the presence of other rhinologic symptoms, such as facial pain or pressure, epistaxis, and nasal obstruction. In the presence of neurological symptoms, such as headaches, seizures or symptoms of raised intracranial pressure, the patient should be referred to a second level of care for further investigation.6
Common causes, as well as those less common to olfactory disturbance but that should not be missed, are listed in Table 2.2,17
After a detailed anamnesis, the patient examination shall include a complete head and neck inspection. With regard to nose examination, signs of trauma and deformities (deviated septum) should be excluded and an inspection of nasal cavities performed, looking for nasal discharge, nasal polyps, masses, foreign bodies or other signs of inflammation.6
A neurological examination is the next step, with special focus on cranial nerves and particularly on optical, trigeminal and facial nerves.6,17
In selected cases, imaging of the paranasal sinuses and brain may be considered to exclude organic pathology (including malignancy), and to outline the olfactory bulb morphology.17
Ideally an olfactory assessment with a psychophysical test should be established due to the poor correlation between subjective questioning and test performance. These tests consist on the presentation of some odorants and assess odor threshold, odor discrimination and odor identification.3 However, we consider that for most general practitioners this is not feasible, due to short appointments and also because physicians are not familiarized with these tests, revealing lack of knowledge in this area.
Table 2: Differential diagnosis.
| Sinonasal Causes | Other causes |
|---|---|
| Rhinosinusitis | Head trauma |
| Nasal polyps or intranasal tumors | Other infections |
| Gross septal deformity | Secondary to medication or substances |
| OD secondary to nasal surgery | Neurological disease |
| Neurodegenerative disease | |
| Intracranial lesion |
Management and Treatment
Studies have shown that most patients presenting with postinfectious OD had spontaneous recovery of their sense of smell without any treatment. However, sometimes the cure may not occur, therefore being important to find a way to treat this condition.
Although there is still limited evidence, there are already a few studies evaluating the efficacy of specific treatments for patients with COVID-19-related OD.
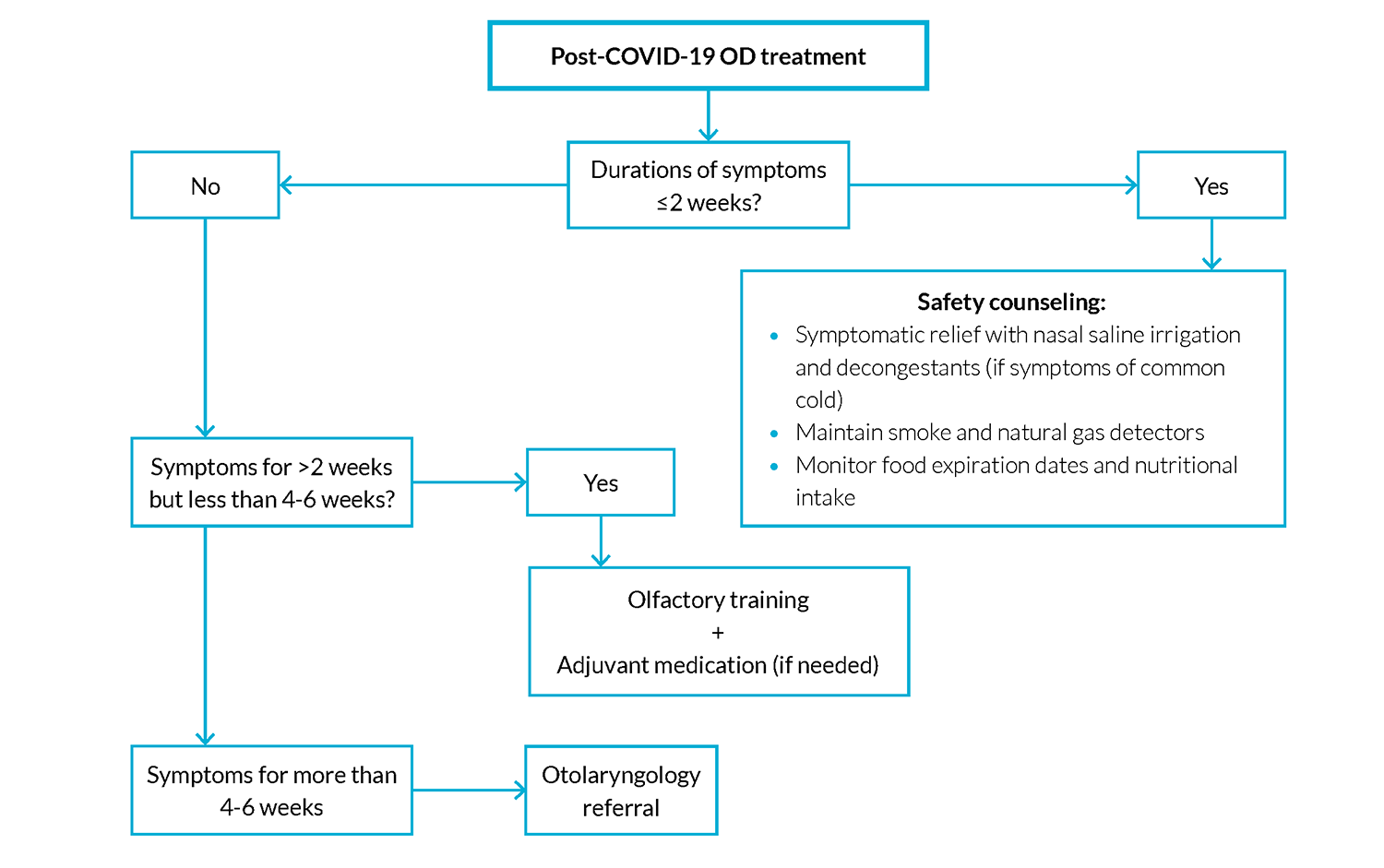
The vast majority of patients that present with COVID-19-related OD can be managed in primary care.6
The main indication for referral to secondary care is the presence of previous mentioned red flag symptoms, which can lead to the need of a nasoendoscopy to exclude other pathologies. In addition, the absence of response to the initial treatment is also an indication for referral to an otolaryngologist.5,6
As mentioned above, the treatment should be considered if olfactory impairment persists beyond 2 weeks.3,5
Potential treatment options and their evidence will be now presented and discussed.
Additionally, a possible management scheme for treatment of post-COVID-19 OD in primary care can been seen in the Fig. 2.
Olfactory Training and Support
Olfactory training (OT) is one of the therapeutics with stronger evidence concerning the improvement of olfactory dysfunction. It consists in the exposure to various odors, conducting modulation and regeneration of the olfactory neurons.7,12 These phenomena of neuroplasticity apparently play an important role in the recovery of olfactory function. Nonetheless, molecular and cellular mechanisms behind them still remain uncertain. Despite this, olfactory training is the only current therapeutic option for post-infectious OD with a strong scientific base.3,6,15
Two types of OT are described in the literature: classic and modified.7
Classic OT consists of a five-minute exposure to 4 different odorants (phenyl ethyl alcohol, euctol, citronalypella, and eugenol) twice a day for at least 12 weeks.7
Modified OT differs from the classic OT, since it uses three sets of different odors and lasts longer in time (36 weeks).7 The first set is the same as the one used in classic OT and it lasts for 12 weeks. It is followed by a second set of different odorants (menthol, thyme, tangerine, and jasmine) for a further 12 weeks, and then followed by a third set of odorants (green tea, bergamot, rosemary, and gardenia) for the final 12-week period.
There are already OT kits that can be used by patients at home, which is more convenient.
Patients should be advised about some cautions regarding OT: they must inhale naturally, slowly, and gently, because sniffing too quickly can result in not being able to detect the smell; each odor must be sniffed for about 20 to 30 seconds. Recent evidence suggests that modified OT has better results than classical training.7
This therapy has the advantage of being low-cost and having negligible adverse effects, which makes it safe.3 Another positive aspect related to this therapy is the fact that it can be associated with pharmacological therapeutics, such as corticosteroids.
In August/2020, British Rhinological Society (BRS) published a guideline for the management of new onset loss of sense of smell after a COVID-19 infection. BRS consensus guidelines recommend olfactory training (OT) for patients with COVID-19-related OD which lasts more than 2 weeks.5
Corticosteroids
Corticosteroids have been pointed as a treatment with high potential benefit in the approach of patients with COVID-19-related OD and, therefore, some studies have been exploring the use of different formulations, doses and routes of steroid administration in these patients.4,20,21 The beneficial effect of corticosteroids in COVID-19-related OD may be related to their anti-inflammatory activity, which can possible resolve the inflammation of olfactory neuroepithelium.12,21 Oral and topical steroids are cheap and widely available, making their use very practical in most settings.
Despite all this, there are no large randomized controlled trials (RCTs) focused on patients with COVID-19-related OD7 and different studies show conflicting results.7,22
Intranasal corticosteroid sprays
Nasal steroids’ side effects profile is better than that of systemic steroids, which makes them potentially safer compared to oral corticosteroids.7 Although topical steroids are currently used in many conditions, they still have some possible disturbing effects, such as nasal irritation, epistaxis or other more serious local complications (e.g., ischemia). Thus, weighting potential benefits versus risks of this therapy is crucial.12
As stated before, results of different studies are not consensual. Abdelalim et al studied, in a prospective, randomized, controlled trial, the effect of topical corticosteroid (mometasone furoate) in the treatment of anosmia/hyposmia in patients recovered from COVID-19 infection. This study concluded there was no advantage in intranasal corticosteroid therapy versus placebo, regarding odor scores, anosmia length and recovery rates.11 Similarly, Rashid et al concluded there was no benefit in the use of intranasal betamethasone, in a randomized, double-blind, placebo-controlled clinical trial with 276 patients recovered from COVID-19 infection and with anosmia for more than 15 days.4 In other studies, such as the one by Singh et al, patients reported a significant improvement of anosmia with fluticasone nasal spray.20 In a multicenter randomized case-control study, Vaira et al assessed the effect of corticosteroid therapy in the treatment of patients with COVID-19 with anosmia or severe hyposmia, for more than 30 days. The treatment group received systemic prednisone, nasal irrigation with betamethasone and ambroxol - a mucolytic and a decongestant - reporting significantly higher and faster improvements of olfactory scores compared to the control group, which had not received any therapy.1
Despite the contradicting results in this area, as described above, BRS consensus suggests the optional use of topical steroids in patients with anosmia lasting more than 2 weeks, associated with nasal symptoms.5
Oral corticosteroids
BRS consensus does not recommend the prescription of oral corticosteroids for patients with OD lasting more than two weeks, with persistent COVID-19 symptoms, and recommends its optional prescription for patients with OD lasting more than 2 weeks, as an isolated symptom.5
Le Bon et al conducted a study to measure the efficacy and safety of oral corticosteroids along with olfactory training, and they concluded that this therapeutic association has better results on the olfactory recovery than olfactory training by itself.23
Saussez et al in a prospective observational controlled study, with 152 patients, in four hospitals, compared different treatments for post-COVID related olfactory dysfunction: olfactory training (OT) alone, oral corticosteroids plus OT or nasal corticoids plus OT. They concluded that, after one month, patients treated with oral corticosteroids plus OT showed significantly higher rates of improvement (normosmics), but after two months of evaluation there were no significant differences between the groups, admitting that corticosteroids merely accelerate the recovery.21
A systematic review published in May 2020 analyzed 36 studies on post-viral olfactory dysfunction, six of which using systemic steroids as the treatment approach, assigning a strength of recommendation class C. Thus, providers should consider the benefits versus risks of systemic corticosteroids in the setting of their patients’ medical comorbidities.8
Vitamin A drops
Studies show that metabolites of vitamin A may play a role in the regeneration of the olfactory epithelium and the olfactory bulb. Based on this assumption, vitamin A intranasal drops may be used as adjuvants in the treatment of individuals with post-viral olfactory loss.7,12 However, due to the conflicting results of studies conducted in this area and the lack of strong evidence about its benefits, vitamin A is not formally recognized as a treatment option for COVID-19-related OD.3,5,15
α-lipoic acid
α-lipoic acid is a fatty acid that stimulates the expression of nerve growth factors, and it seems to have antioxidative and neuroprotective effects.7,24
Although some studies show the potential benefit of this treatment, they involved small populations and are non-randomized as well as uncontrolled, so there is a need for placebo-controlled studies in large groups for conclusions to be reached.15,24
BRS does not recommend α-Lipoic acid for patients with COVID-19-related OD lasting more than 2 weeks.5,24
Smoking cessation
Smoking has been appointed as a risk factor for OD in the general population, but specific data about the effects of smoking in COVID-19-related OD are sparse.7,18,19
Nevertheless, smoking cessation has a positive effect on olfactory function; thus, undertaking it may be helpful for some patients.7,19
Theophylline
Theophylline mechanism of action on the olfactory neuroepithelium is not fully understood, but it seems to help on olfactory neuroepithelium regeneration.7,25
Thus, intranasal theophylline may influence the perception of smell and taste through a direct action on the brain. At the same time, it is associated with few side effects, in contrast to the use of oral theophylline.15,26
However, there is a need for stronger evidence in this area, specifically about the effects of intranasal theophylline in COVID-19-related OD. Therefore, it is still not recommended.15
Omega-3 supplements
Omega-3 polyunsaturated fatty acids are essential components of membrane phospholipids, with significant influence on gene expression.3
A cross-sectional study with a 5-year follow-up showed that older adults with a diet rich in fatty acids had reduced odds of having olfactory dysfunction.27 This may be caused by the possible neurodegenerative and anti-inflammatory effects of omega-3 on the olfactory mucosa. The exact mechanism behind these effects has yet to be elucidated. To include its use in generalized OD treatment guidelines, further investigation is required.5
Bearing this in mind, BRS consensus suggests the optional use of omega-3 in patients with COVID-19-related OD lasting more than 2 weeks as an isolated symptom or following resolution of any other COVID-19 symptoms.5
Sodium citrate
Intranasal sodium citrate, due to its ability to sequester calcium ions, is thought to reduce free mucosal calcium, causing a reduction in negative feedback and increasing sensitivity of the nasal mucosa to odorants.7
From the studies conducted so far, intranasal sodium citrate seems to be a low-risk intervention, with demonstrated temporary improved olfaction. However, long-term benefits are unclear. Data for intranasal sodium citrate spray are very promising in initial studies, but more definitive data with clinically relevant long-term outcomes are needed. Taking this into consideration, there is not enough current evidence to assure the recommendation of this treatment for COVID-19-related OD.7,8,15
Referral to Secondary Care
Patients with COVID-19-related OD can be referred to a secondary care if they have isolated loss of smell lasting more than 3 months, despite the established treatment; if OD is associated with other nasal symptoms and lasts for more than 4-6 weeks; and if patients present with red flag symptoms. In these cases, patients should be referred to an otolaryngologist for consideration of a face-to-face consultation and a nasendoscopy to exclude other pathologies.5
Discussion
The main goal of this review was to define a guideline protocol for patients recovered from COVID-19, who present with olfactory dysfunction.
To date, the literature agrees in the general approach to these patients. It tends to follow the same approach as in other OD related to viral infections. The diagnosis of viral-associated olfactory loss is made primarily via patient history. A detailed history would also rule out other causes of ongoing olfactory loss or symptoms that are indicative of more worrisome pathology. Imaging is rarely performed unless symptoms and examination suggest an alternative diagnosis.
However, since post-COVID-19-related OD is a relatively new entity, treatment options available lack the scientific evidence necessary for a sustained treatment guideline. In fact, most of the evidence base considered is not COVID-19-specific, which poses a limitation to this review.
Nevertheless, olfactory training has emerged as the most efficacious treatment and daily practicing with three odorants has become standard recommendation for post-COVID-19-related OD.
Despite smell training, different centers studied the effect of cortisone - intranasal as well as oral - on the outcome regarding OD. Despite encouraging safety profile of topical steroids application, the existence of heterogeneous data makes conclusions regarding their use challenging. Even so, BRS consensus suggests the optional use of topical steroids in patients with anosmia lasting more than 2 weeks, associated with nasal symptoms.5
There are several other treatments presented in the literature. Overall, there is no strong evidence for any pharmacologic treatment of post-COVID-19-related OD.
Conclusion
This pandemic has renewed the interest in post-viral olfactory dysfunction. Currently, the natural history of post-viral OD cannot be accurately predicted. There are cases in which some patients experience a period of transient anosmia, followed by a full recovery of the olfactory function, while others experience permanent OD. We anticipate that both family medicine and otolaryngologists will see an increase in the number of patients presenting with this condition, considering the recent rise in COVID-19-related OD.
Olfactory training is considered an efficacious and safe treatment option. Further studies are required to validate its efficacy and indications for oral or topical use of corticosteroids. The medical community is rapidly accruing information, and standards are likely to change quickly, bringing additional results.
We hope that the newfound spotlight on OD will drive clinical research and lead to the development of novel treatment options for patients with COVID-19-related OD.