Introduction
Renal foreign body granuloma are infrequent findings, particularly those ones related to suture material. Despite being sometimes symptomatic, they are much more frequently an incidental finding in a radiological examination. Its differential diagnosis is hampered by the lack of specificity of its radiological features.
Case report
A 12-year-old boy is being followed after having been submitted to an Anderson-Hynes pyeloplasty 7 years before. During his follow-up, it is detected a 4 mm calculus in the left kidney as well as 10 mm cortical cyst in the right kidney. At this point, it is also described in a follow-up ultrasonography a solid nodular lesion, possibly in the dependence of the left kidney, with a hypoecogenic periphery and hyperecogenic center (Fig. 1).

Figure 1: . Ultrassonography: A solid nodule in close contact with the left kidney, 26 mm in diameter, hypoechogenic in the periphery, with a central hyperechogenic component, which suggested the presence of fine calcifications or fat.
Subsequently, magneticresonance imaging (MRI) is performed, which reports a lesion with non-specific features, measuring 3.6x2.2x3.1 cm, showing peripheral hyposignal in all sequences suggesting fibrous component and central hypersignal in T2, with discrete contrast enhancement (Fig.s 2A and 2B).
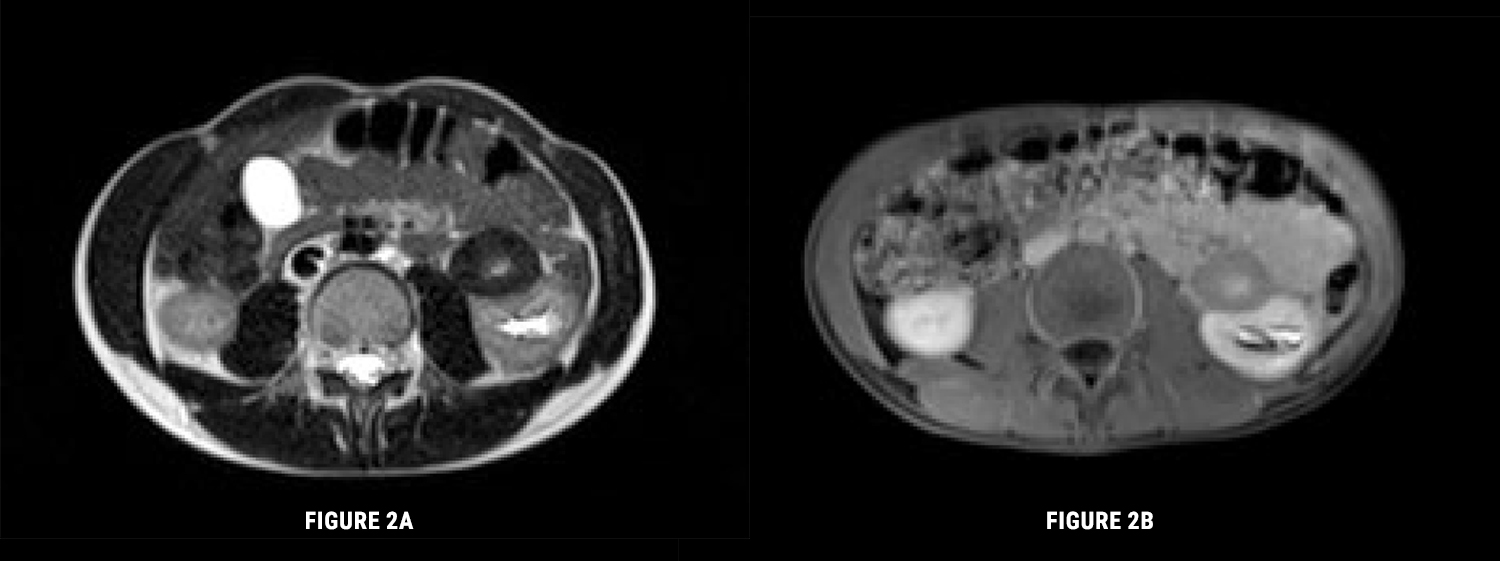
Figure 2: A) Magnetic ressonance imaging. Axial T2. Lesion of nonspecific characteristics, with a diameter of 3.6x2.2x3.1 cm, admitting to be a neoformation with fibrous component in the periphery. B) Magnetic ressonance imaging. T1FS Gd: After intravenous gadolinium. The lesion enhances less than the renal parenchyma and reveals slight central late enhancement.
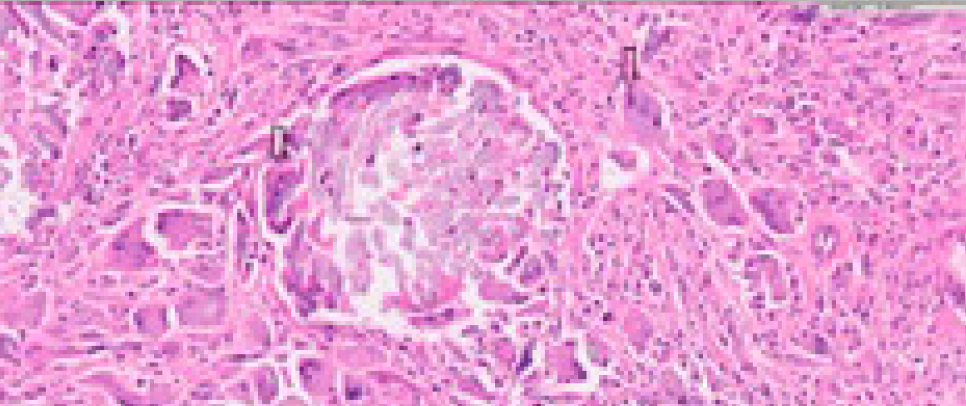
A percutaneous biopsy reveals a morphological picture compatible with chronic xanthogranulomatous inflammatory process. The lesion was submitted to surgical removal. After surgical removal of the lesion, anatomopathological examination describes histiocytic cells with frequent participation of foreign body type giant cells and granulomatous reaction in relation to exogenous suture-like material (Fig. 3).
The final diagnosis was renal granuloma due do foreign body material. The suture material used in the pyeloplasty was polydioxanone suture (PDS →), which a sterile synthetic absorbable monofilament suture is made from the polyester p-dioxanone.
The patient was discharged briefly after surgery and remains asymptomatic since then.
Discussion
Renal granulomas are very rare situations, most of which are due to surgical gauze left inadvertently inside the abdominal cavity1 or due to the ingestion of foreign material, causing erosion from the gastrointestinal tract through the urinary tract.1,2 The cases related to suture are even more exceptional and are due to the persistence or delay of absorption of the suture material used for closure of the pyelocalicial system and nephrostomies, being usually accidental findings.
This entity may present in a variety of forms, namely: purulent percutaneous fistula, pseudotumors and lithiasis.1 Clinical manifestations may appear early or late in the postoperative period, depending on the type of inflammatory reaction involved.1 There are cases described of surgical complication due to late persistence of suture, from 3 to 20 years after surgery.2-4 Its formation is due to a nodular, chronic reaction with cell-mediated inflammation to a persistent foreign agent such as suture material.3
The main differential diagnoses are tumors, abscesses, pseudo-cysts and hematomas.1
Although, computerized tomography and MRI are the elective imaging tests of choice for diagnostic approach, they may not be able to distinguish a foreign body granuloma unambiguously from other entities,1 especially from tumors,3 requiring a more invasive approach through percutaneous biopsy and surgical excision. Therefore, the diagnosis is usually established by the examination of the excised tissue.
Conclusion
Renal foreign body granulomas are a difficult entity to diagnose, given the lack of clinical specificity and imaging findings. The most relevant factor for diagnosis is a high index of suspicion, especially in patients with a history of nephro-urological surgery.3