Introduction
“Saturday night palsy”, also known as “lovers’ paralysis”, is a neuropathy of the radial nerve, that occurs from prolonged and direct pressure onto the upper medial arm, resulting in compression of the radial nerve at a certain point in its path along the humerus, usually at the level of the spiral groove.1 These designations are based on the fact that this compression occurs, frequently, after excessive alcohol intake - which is associated with an incorrect position of the upper limb during sleep, namely by placing the arm on hard surfaces (chair or table, for example) - or after having fallen asleep with the companion's head resting on the person’s arm. However, this pathology can have other causes besides extrinsic compression, including: fractures of the humerus, nerve compression due to neoplasms, bone spur or cysts, demyelinating diseases, lead poisoning or consumption of neurotoxic substances, among others. The radial nerve originates from C5 to T1 nerve roots, and paralysis of this nerve causes loss of sensitive and/or motor functions, depending on where the nerve was injured.2 This palsy is thought to be the fourth most common mononeuropathy worldwide, affecting about 2.97 per 100 000 men and 1.42 per 100 000 women.3) The following case refers to a patient observed in an acute consult in a Primary Care Unit, after waking up with a wrist drop.
Case Report
We hereby report the case of a 44-year-old Caucasian male with no relevant medical history or usual chronic medication intake. The patient resorted to the Primary Care Unit 8 hours after waking up with a wrist drop, numbness, tingling and a feeling of heaviness in the right upper limb, having immediately found that he was unable to perform active wrist extension and stated difficulty grasping objects. He also referred pain and loss of sensation on the back of the hand and feeling of discomfort with pronation/supination movements. The patient denied other symptoms, alcohol ingestion or other consumption of potentially neurotoxic substances, although he stated that he fell asleep with his 6-year-old son's head resting on his right arm. Upon objective examination, the patient was unable to perform active extension of the wrist or metacarpophalangeal joints (Figs. 1 and 2). He presented changes in muscle strength (grade 4/5 in the right upper limb on wrist and finger extension, as opposed to grade 5/5 in the left upper limb) and loss of sensation in the lateral portion of the back of the hand, specifically near the tenar eminence and in the posterolateral aspect of the third finger. The tricipital and bicipital reflex was present and maintained, but the brachioradialis reflex was absent on the right limb. Since the patient maintained the ability to perform abduction and extension of the arm, we were able to conclude that the injury occurred distally to the branching of the axillary nerve (which will innervate the deltoid muscle).
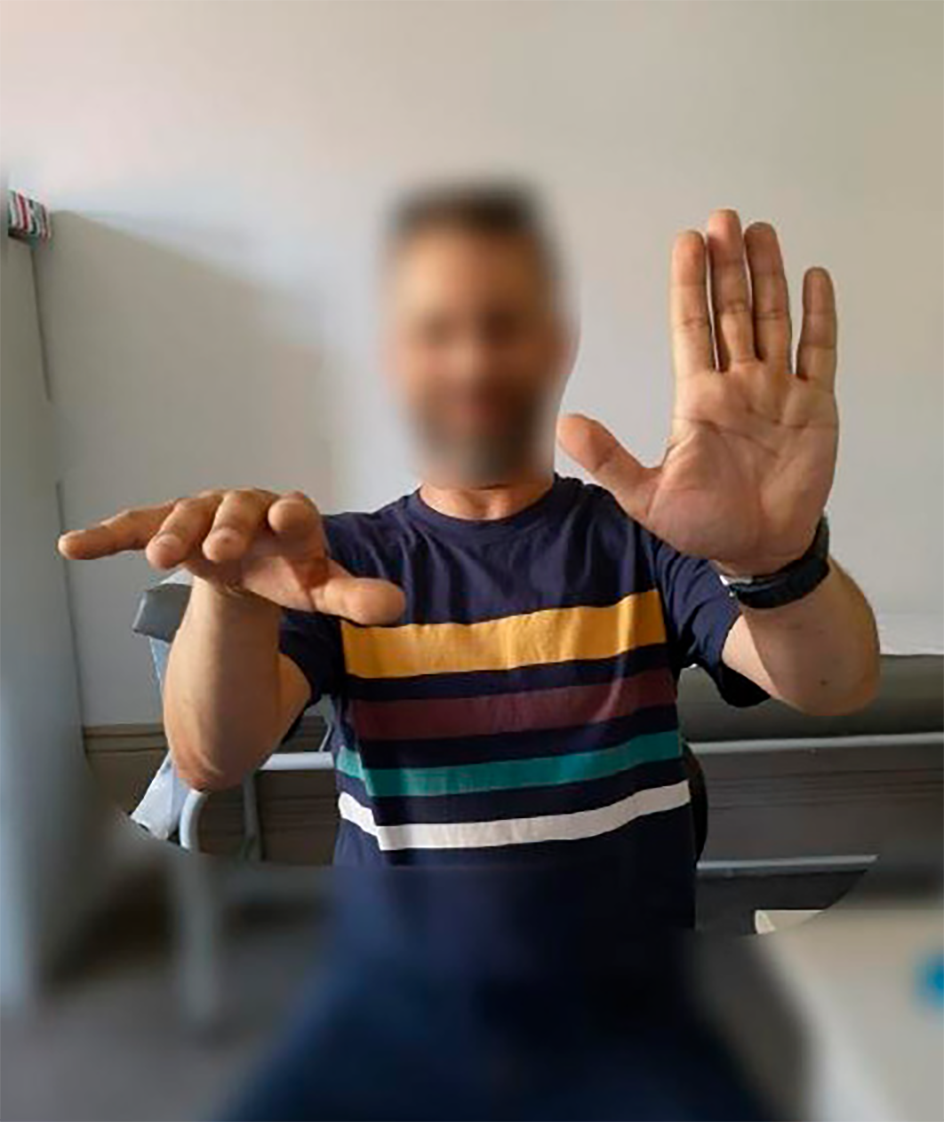
Figure 1 Front view of patient unable to perform active extension of the right wrist and metacarpophalangeal joints.
We requested an electromyography that revealed significant lesion on the right radial nerve, over the distal third of the arm, affecting the motor branch. There was evidence of recent and accentuated neurogenic changes in its dependent muscle territory on the right forearm, without denervation, but with a 37% blockage, typical of a “Saturday night paralysis”. We also requested a soft tissue ultrasound of the right elbow, that showed no abnormal signs. Given the pain referred by the patient, we prescribed pregabalin 25 mg (initial dosage) and ibuprofen 600 mg. The patient initiated physical therapy the same week his symptoms began, and, at the end of the first month, he was already able to perform partial extension of the wrist. The patient made a full recovery, three and a half months after the onset of his “Saturday night palsy”.
The patient provided written consent, which was filed in the patient’s medical process.
Discussion
The motor and sensory deficits shown by the patient allow us to infer the location of the radial nerve injury. Since the patient maintained the ability to perform abduction and extension of the arm, we were able to conclude that the injury to the radial nerve occurred distally to the branching of the radial nerve into the axillary nerve (which will innervate the deltoid muscle). Otherwise, it would be advisable to also request a magnetic resonance imaging (MRI) of the brachial plexus and cervical spine. When first evaluating a patient with a “Saturday night palsy”, a thorough assessment should be performed to rule out other differential diagnosis, such as traumatic causes (incorrect use of clutches and humeral fractures, for example) and iatrogenic injuries (namely surgeries or injections). Internal compression by growing cysts, masses, tumors, muscle hypertrophy and neurologic diseases can cause isolated palsies as well.4-6 Additionally, a central nervous system lesion, namely in the motor hand area, can mimic a radial nerve palsy, and this should be suspected either in acute cases without clear history of compression or subacute cases without changes in the nerve conduction studies. It is also important to exclude associated illnesses that can increase the susceptibility to compression, namely diabetes and alcohol overuse, as previously stated.
The treatment of “Saturday night palsy” consists mainly on physical rehabilitation, often requiring a wrist splint to help extend the wrist. If the patient is in pain, the treatment can include pharmacological measures, with the prescription of non-steroidal anti-inflammatory drugs, systemic corticosteroids, steroid injections, pregabalin or gabapentin. In this case, the patient only took ibuprofen during the first month of the recovery, and did not feel the need to continue with pregabalin. Surgical approach is usually only required in severe injuries of the radial nerve, or in cases in which the compression results from an intrinsic process, such as a fracture, mass or cyst.1 “Saturday night palsies” usually have a favorable prognosis, but rehabilitation can be an extensive process, with minor cases resolving at the earliest in 2-4 months, and being able to take up to 6 months in many cases.4) The recovery depends on the extent of the injury, which is determined by the intensity and duration of compression.1 Mild damage usually results in a transient conduction block, without nerve degeneration, frequently showing a full recovery. Greater damages can result in nerve degeneration, which lower the odds of a complete recovery. In all cases, patients should be given realistic expectations of their recovery process, which may not meet their objectives or desires.1 The mild cases of this neuropathy can be managed in Primary Care Units, trough the requisition of adequate exams, and the prescription of analgesic treatment and physical rehabilitation to increase the chance of recovery. Patients should be advised to follow up regularly with their doctors to check the progress timeline, and to promptly refer to a surgeon or a neurologist if needed.
















