Introduction
Knowledge societies in the 21st century face the paradox of health decision making - while people are increasingly dared to make healthier choices, they are not being sufficiently prepared and supported by health professionals to make them (Kickbusch et al., 2013). The empowerment and accountability of people for their health is a significant challenge for nursing, particularly regarding the importance of Healthcare-Associated Infections (HAIs) prevention and control.
The importance of involving patients and their families in HAIs prevention and control has been established for years. Increasing discussions around safety culture highlight the need to create a collaborative environment between health team members, administrators, patients, and their families to overcome health barriers and strive for quality and efficient care (Joint Commission, 2009). However, despite significant advances in recent years, the risk of developing HAIs in healthcare institutions is yet to be overcome and therefore requires effective preventive measures. One crucial challenge in this scope is related to the recurrent transmission of pathogenic microorganisms through the hands of health professionals and hospitalized patients (cross-contamination)(Istenes et al., 2013). Equally relevant, hospitalized patients are likely to be exposed to pathogenic microorganisms in clinical settings through direct contact with contaminated devices and surfaces, commonly known as self-contamination (Istenes et al., 2013). Hand hygiene (HH) is considered one of the simplest and most effective practices in reducing HAIs, thereby contributing to the reduction of patient morbidity and mortality. The importance of HH among hospitalized patients dates to the 1980s, with the development of international quality improvement projects and dissemination through scientific publications. Although HH standards traditionally focus on health professionals (Graveto, Rebola, et al., 2018; Graveto, Santos, et al., 2018), it is essential to include and educate hospitalized patients and their families about the relevance of this practice, establishing them as active agents in HAIs prevention (Landers et al., 2012; World Health Organization, 2009). Nurses’ patient education plays a fundamental role in HH adherence, and the contributions of current technological aids associated with simple and innovative strategies cannot be overlooked (Park & Seale, 2017). Nurses’ patient education can more easily impact health outcomes if they include a definition of terms, examples, illustrations, reminders or suggestions (Kickbusch et al., 2013). Thus, we proposed to conduct a narrative review with two main goals: i) to synthesize the latest scientific evidence regarding nurse-led interventions focused on hospitalized patients’ adherence to HH; ii) discuss the impact of the found nurse-led interventions on the prevention of HAIs.
Methodological review procedures
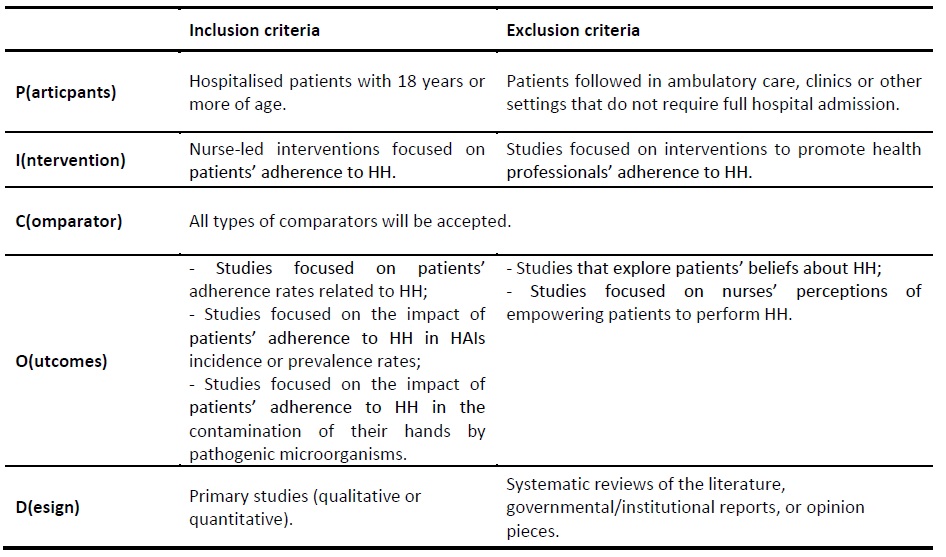
To address the review question “Can nurse-led interventions enhance hospitalized patients’ adherence to hand hygiene and its impact on the prevention of HAIs?”, a narrative literature review was conducted. To delineate the inclusion and exclusion criteria, the Participants, Interventions, Comparator, Outcome, Design (PICOD) mnemonic was used (Table 1)
The search strategy included published studies and was composed of three steps: i) restricted search in MEDLINE (via PubMed) to identify articles on this topic, followed by the analysis of text words in titles and abstracts and index terms used to describe these articles; ii) a second search using all keywords and index terms identified in the included databases; iii) the reference list of all articles and reports found in the search were analyzed to identify supplementary studies.
Boolean logic was used with search terms, adapting the strategy to each of the included databases. The natural language terms used were: nurs*; hand hygiene; hand washing; handwashing; hand disinfection; patient; and inpatient. Descriptors were also used according to each specific database, namely Medical Subject Headings (hand hygiene; hand disinfection; nurses; patients) and CINAHL Subject Headings (handwashing; nurses; patients). The search strategy was adapted to each of the included databases. Regarding the search strategy and study identification, the following online databases were searched: MEDLINE (via PubMed), CINAHL (via EBSCO), and the Cochrane Library. Studies written in English, Spanish, French, and Portuguese were considered for inclusion in this review, published between January 1st, 2016 and December 31st, 2018. The final database search was conducted on April 26th, 2019.
To assort study relevance, two independent reviewers confronted the information provided in the title and abstract with the inclusion criteria delineated. Every time the reviewers had doubts about the relevance of a study, the study was included for full-text analysis. Two reviewers independently revised the full-text version of the articles to comprehend if the inclusion criteria were met. Divergences between the reviewers
were decided through dialogue with a third reviewer. An identical approach was employed to the studies identified after the analysis of the reference lists. Data extraction was conducted by two independent reviewers using an instrument previously created by the authors. The instrument was designed to recover data consistent with this review’s question and objectives. This literature review followed the steps recommended in the Preferred Reporting Items for Systematic Reviews and Meta-Analyzes checklist (Moher et al., 2009).
Results
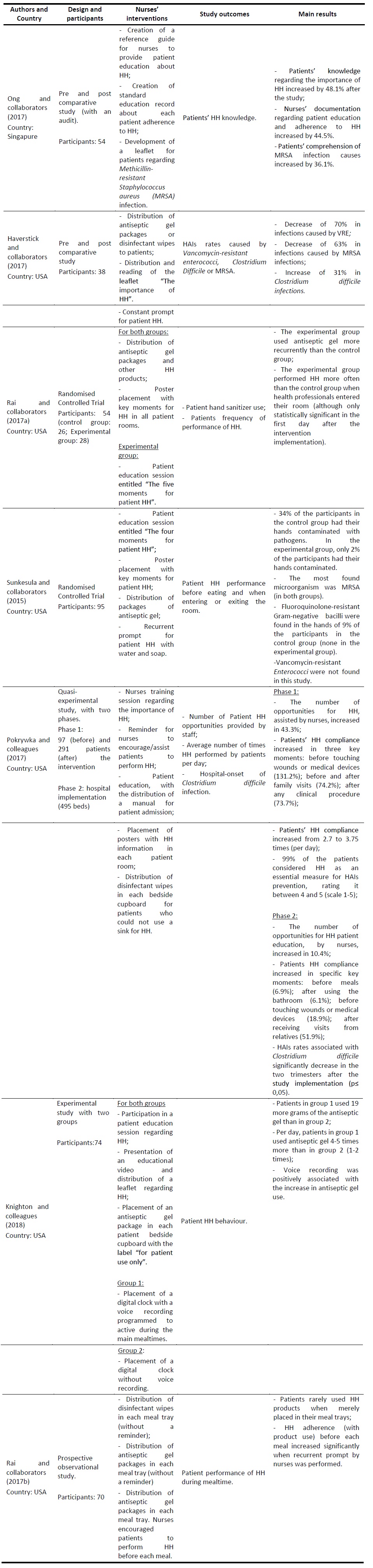
The search identified 691 potentially relevant studies. Of these, 202 were excluded for being duplicates. The remaining 489 articles were screened by title and abstract. Of these, 16 articles were included for full-text analysis by two independent reviewers. Overall, 9 studies were excluded, due to the type of participants (n = 5), intervention (n = 1) and outcome (n = 3) not matching the inclusion criteria. Therefore, seven studies were included for data extraction and synthesis (Table 2).
Discussion
The included studies addressed nurse-led interventions that promote patients' HH adherence. Patient education on the importance of HH stands out as the most chosen nurse-led intervention, with a significant impact on patients’ knowledge in this domain. As an example, after the implementation of an educational nurse-led intervention (with distribution of an informative leaflet), Ong and colleagues (2017) identified a 48.1% increase in patient awareness of the importance of HH and a 36.1% increase in their knowledge of MRSA infections. This result was also obtained by other study authors who implemented traditional nurse-led educational interventions (Pokrywka et al., 2017; Rai et al., 2017a). In the study by Pokrywka and colleagues (2017), 99% of the participants highlighted the importance of HH in the prevention of HAIs and increased the daily frequency of HH from 2.7 times to 3.75 times. This positive trend continued after the institutional implementation of the study, with significant increases in patients' adherence to HH, especially after receiving visits (51.9%). Similarly, Rai and associates (2017a) identified an increased frequency of HH, with greater consumption of antiseptic gel in the experimental group, especially at specific times like the entry of health professionals into their room. However, this result was only statistically significant for the first day after the implementation of the nurse-led intervention (Rai et al., 2017a).
Such results reinforce the need to constantly promote patients' adherence to HH during their hospital admission, especially during mealtimes. For example, Rai and colleagues (2017b) found that the mere distribution of HH products like disinfectant wipes or antiseptic gel did not correlate into greater patient adherence. In their study, patients who used HH products more often were the ones who were constantly prompt by nurses. Likewise, Knighton and associates (2018) found that through a pre-established voice recording during mealtimes, patients increased their adherence to HH. This result indicates the potential of technology as a tool that helps nurses to recurrently remind patients of the need for HH.
Impact in the prevention of HAIs
The nurse-led intervention implemented by Sunkesula and collaborators (2015) was comprised of an education session for the promotion of HH, placement of posters in patients’ rooms, frequent encouragement of HH and distribution of antiseptic gel packages contributed to the reduction of contamination of the hands of the hospitalised person. After its implementation, 2% of the patients in the experimental group had their hands contaminated with MRSA versus 30% in the control group. Fluoroquinolone-resistant gram-negative bacilli were also found in the hands of 4% of the control group participants, whereas in the hands of the experimental group participants this pathogen was not found (Sunkesula et al., 2015).
In another study, after the implementation of a similar nurse-led intervention, that also included the provision of disinfectant wipes to patients, the incidence of HAIs caused by Clostridium difficile decreased (Pokrywka et al., 2017). Haverstick and colleagues (2017), identified that an increase in patients’ HH adherence was associated with a 70% decrease in the incidence of HAIs caused by VRE and 63% by MRSA. However, the authors identified a 31% increase in HAIs caused by Clostridium difficile, which could be attributed to the incorrect use of specific HH products such as disinfectant wipes. This result highlights the need to select HH products not only based on patients' preferences and capabilities but also based on current known outbreaks of multiresistant microorganisms in hospital settings.
Promotion of patients’ self-care
Despite its recognised importance in the prevention of HAIs, some hospitalized patients do not have the opportunity to perform HH due to their functional status and dependence (Haverstick et al., 2017). Moreover, patients’ lack of dexterity or cognitive abilities were also identified as key factors that influence HH adherence (Pokrywka et al., 2017). According to Okada and collaborators (Okada et al., 2016), the degree of contamination of the hands of hospitalised patients is higher in individuals with physical limitations. Since dependent people have difficulty in mobilising and performing basic needs (e.g., showering or using the bathroom), nurses and healthcare assistants often replace them in their self-care. Such scenarios reduce the opportunities to prompt patients to perform HH actively (Pokrywka et al., 2017).
Nurses must be aware of the suitability of HH products for each patient’s health condition and preferences (Knighton et al., 2018). Certain materials may not be compatible with the person's motor and cognitive abilities, such as the use of disinfectant wipes and antiseptic gel packs. As an example, in one study, patients who select antiseptic gel packs stated that it is easier, quicker, and more convenient to use (Rai et al., 2017b). However, patients who prefer disinfectant wipes indicated that they could be used more than once in a single moment (e.g., meal) and have a mechanical action that increases HH efficiency when hands are visibly soiled (Rai et al., 2017b).
Promoting hospitalised patients' HH encompasses their capacity and active role in contributing to the prevention of HAIs and, consequently, to their safety when using health services (Seale et al., 2016). Given that nurses are the health professionals who have continuous contact with admitted patients, they are in a privileged position to promote HH (Okada et al., 2016). However, several challenges can hinder nurses' role within this scope, such as: the lack of time to encourage and assist patients; nursing ratios; architectural barriers (e.g., existence of bathrooms in each patient room or the adaptability of washbasins for wheelchair use); and availability of individual HH products for patient use due budget constraints (Srigley et al., 2016).
The found nurse-led interventions and strategies considered most effective for the promotion of HH in hospitalised patients are similar to the WHO recommendations for health professionals’ adherence to HH (Kickbusch et al., 2013; World Health Organization, 2009). These educational interventions must include visual clues, the provision of HH products and conduction of active vigilance and verbal reinforcement (Haverstick et al., 2017; Pokrywka et al., 2017; Srigley et al., 2016). Nurse-led interventions can contribute to patients’ health literacy, empowering them to make the most appropriate health decisions and improve their self-care skills (Kickbusch et al., 2013).
As limitations of this review, the significant heterogeneity of studies found concerning their objectives, methodological design, and sample, may have limited data analysis, comparison, and synthesis. Thus, we believe that future experimental studies with larger samples are required, focusing on a set of pre-defined outcomes in light of recent international recommendations for HH. In the same line of thought, the inclusion of studies published in English, Portuguese and Spanish may have limited the number of results that met the inclusion criteria. Also, studies accessible through other international databases could add contributions to the research question. Future literature reviews must address the weaknesses acknowledged to develop more comprehensive research in this scope.
Conclusion
Through this review, it was possible to identify nurse-led interventions that positively contribute to patients’ adherence to HH. Out-of-the-way nurse-led interventions are not enough to generate behavioural changes. Although simple educational sessions are essential to increase patient knowledge about the importance of HH as a form of HAIs prevention, the included studies in this review show that multimodal interventions prove to be more effective in medium to long-term modifications. To achieve better patient outcomes in this scope, nurses can combine traditional educational sessions with other resources and strategies such as distributing HH products, handing out information leaflets or placing posters in patient rooms. Moreover, nurse-led educational intervention must be phased, creating recurrent opportunities for patient engagement and encouragement in respect to HH.
Equally important, the included studies also highlighted the impact of such nurse-led interventions on HAIs prevention, with fewer studies analysing the positive impact of such interventions in the contamination of patients’ hands with pathogenic microorganisms. The importance of person-centered care when encouraging patients’ self-care in this domain was a recurrent concern of the included study authors. Nurses must be aware of patients’ preferences when choosing appropriate HH products, as well as their capabilities and functional status to create effective opportunities for HH.