Introduction
Loss of functional capacity (physical and psychological) may be associated with the deterioration of a chronic disease condition, which may condition the person to functional dependence and self-care deficit, that is, to the need for someone to help in self-care activities. Self-care is considered the taking care of what is needed to maintain oneself, keep oneself going and handle basic individual and intimate necessities and activities in daily life (International Council of Nurses [ICN], 2019). Activities of daily living include eating, bathing, dressing and undressing, using the toilet, getting ready, getting out of bed, moving between bed and chair and turning in bed (ICN, 2019). Orem is an important reference for the development of the concept of self-care, having defined it as a practice of activities that individuals initiate and carry out to maintain life, health, and well-being (Orem, 1991). Her theory gives special emphasis on health deviations, which is when a person is not able to promote the necessary self-care activities and requires the help of another person.
Many nursing therapies aim to reverse functional dependence and self-care deficit as soon as possible. Assessing the self-care activities that the person is able or no to perform, facilitating the development of knowledge and new self-care skills, such as the assessment and reformulation of housing conditions, removing barriers to mobility, or putting handrailings in the bathroom, are of great use when the dependent person has the potential to improve (Lourenço, 2015). For people with functional dependence and a high level of commitment in self-care, nursing interventions aim to replace the person when performing self-care activities. In other words, the nurses' actions are predominantly of the type to execute; for example, position, bathe, dress, feed (ICN, 2019). The present study sought to identify the assumptions used by expert nurses when formulating the clinical judgment of self-care deficit versus the potential to improve self-care.
Background
Promote self-care is the first level of healthcare provided, and its scope includes health promotion, disease prevention, rehabilitation, and palliative care (WHO, 2019). Self-care activities in a person with several chronic conditions, in an advanced stage of the disease, and evidencing cognitive alterations are a current challenge (Jaarsma et al., 2017). Additionally, the influence of family, friends, and health professionals in developing self-care abilities needs to be further investigated (Riegel et al., 2017). Riegel et al. (2012), in the Middle-Range theory on self-care in the context of chronic illness, based on clinical practice, define self-care as a process of health maintenance and disease management rather. This process requires a person to be involved and actively engaged in their own health-illness transition. Therefore, self-care is understood as a polysemic concept and a dynamic process that depends on a person's will power. Is influenced by individual needs, capacities, previously identified disabilities, and a person’s perception of their new health condition. Hence, some self-care activities differ according to the person (Riegel et al., 2012).
After the acute phase of an illness, the onset of the functional dependence and the self-care deficit are considered priorities, meaning that a person must initiate their recovery process. Several factors can limit the ability of a person with functional dependence to recover self-care behaviors and actions at individual and social levels. As well age, health status, decision-making ability, physical ability to perform self-care actions, cognitive and emotional ability (Jaarsma et al., 2017), experience, motivation, beliefs, cultural values, habits, functional and cognitive abilities, support system, access to care and self-efficacy (Lourenço, 2015; Riegel et al., 2012, Vellone et al., 2016).
The current increasing need for healthcare responses associated with functional dependence and self-care deficit is a significant challenge for health services and, in particular, for nurses. The changes in a person's ability to perform self-care activities can be translated into two nursing diagnostic labels sustained on different decision-making bases. For the diagnostic label-impaired self-care a nurse prescribes nursing interventions that replace the person in self-care actions. For the diagnostic label-potential to improve self-care abilities a nurse can prescribe interventions that include assistance, information, and training to improve or regain the performance of self-care activities and promote autonomy. The designation of potential refers to “inherente capacity for coming into being” (ISO 18104, 2014, p.4) that is, the person's ability and the opportunity to develop new self-care abilities and, thus, become more autonomous. Queirós et al., (2021) states that there are two perspectives for diagnostic reasoning, given the universal self-care requirements: i) self-care deficit or ii) the individual's opportunity to develop skills and/or knowledge to deal with the self-care deficit. Highlighting the individual need to acquire knowledge and master skills for managing a new challenging condition (Queirós et al., 2021, p.6). In the long-term, these interventions will produce different outcomes with regards to a person's health condition. However, the question remains, which patients have recovery potential? Improving the ability of a person with functional dependence to perform self-care activities implies systematizing a professional approach in order to regularly and specifically assess the different impairments. Such as physical, psychological, and other constraints/limitations, related to the moment and context experienced by the person (Lourenço, 2015). The factors that positively and negatively influence the self-care behaviors of a person with functional dependence are well known (Schulman-Green et al., 2016). However, this evidence has had little transferability to clinical nursing practice (Lourenço, 2015). Despite the existence of several studies focused on identifying factors that influence self-care behaviors of a person with functional dependence (Jaarsma et al., 2017; Vellone et al., 2016), in the context of clinical practice, no assessment instrument exists to help nurses identify the differentiating indicators of the diagnoses, self-care deficit or potential to improve self-care abilities.
Methodology
Design
This is an exploratory study, using a qualitative method comprising interviews with a focus group.
The Consolidated Criteria for Qualitative Research Reports (COREQ) checklist was used (Supplementary File 1). The study included two meetings held in 2019 with eleven nurses experienced in the care of persons with functional dependence and self-care defict. The meetings lasted about two hours and 30 minutes (Krueger & Casey, 2014).
Participants
Participants were selected by an intentional sampling method to obtain detailed descriptions of the work experience relevant to the study (Krueger & Casey, 2014). The selection criteria were: a) to be a nurse with advanced training in rehabilitation nursing, recognized by the National Order of Nurses; b) have at least three years experience in caring for people with functional dependency and commitment to self-care; and c) sign the informed consent form, voluntarily agreeing to participate in the study and authorize the dissemination of the results obtained in the scientific field. Two weeks before the focus group, participants were contacted by email, and the informed consent form was sent, clarifying the objectives of the study, participation criteria, study methods, and the estimated duration. Three days before the focus group was held, participants were contacted by telephone to confirm the meetings. The place where the meetings were held was accessible to all participants.
Participants were mostly women (82%), aged 36 years or older, with advanced training in rehabilitation nursing, and with 15 years or more of professional experience. Participants worked in long-term care units for functional rehabilitation and training in self-care activities.
Data collection
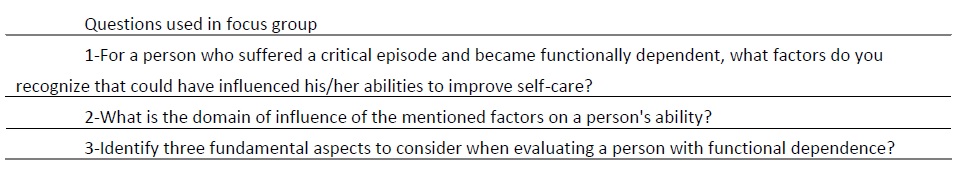
The interaction among the group produced important information relevant to the concepts studied, and participants were encouraged to discuss and comment on thoughts and experiences on the topics under discussion. Previously prepared questions were used in a semi-structured manner to facilitate discussions. Questions were prepared through collaboration and input of all the authors of the document (table 1).
The questions gave rise to valuable discussions and reflections among the participants. Participants were also allowed to raise questions during the focus group interviews.
The sessions were moderated by the first author of the paper, who presented the topics for discussion, kept an active role in conducting and maintaining the discourse, ensuring that each participant had the opportunity to expose his or her opinions. Post-its and a whiteboard were used to collect opinions about the first question presented by the moderator. The participants recorded on post-its factors that, in their opinion, influence the recovery potential of a person with functional dependence and self-care deficit. Subsequently, these concepts were grouped hierarchically into functional domains. The other authors of the paper assisted in this task. The moderator also presented the other questions. The participants discussed their opinions, which were audio-recorded. After data collection, the interviews were transcribed, and the information obtained was submitted to content analysis, following the Strauss & Corbin (2014) guidelines. The moderator performed the transcription because she had insider information about facial expressions, gestures, and tone of voice in which the speeches were delivered. Items that received favorable agreement from at least six (55%) of the eleven focus group participants were added to the results. The content analysis results were collated in a report that was returned to the participants at the second focus group meeting.
The second focus group meeting started with the participants reading the report for 40 minutes. This was followed by a discussion of opinions about the validation of the information. This focus group meeting was also audio-recorded. All suggestions for change were faithfully carried out in the final report by the moderator. All rights related to data protection were respected in the study.
Data analysis
The data gathered from the participants' discussion were at the center for the coding work from an inductive perspective. The knowledge emerged progressively and was marked by the clinical expertise of the professionals. The coding process was the first phase of the analysis, where the substantive codes, properties, and dimensions were identified. This phase was followed by axial coding. The previously grouped data were regrouped into concepts to identify the categories present. The selective coding, which was the last phase of the analytical process, included the refinement of the categories and subcategories previously identified. These were compared and analyzed continuously, integrating some data, and a central category emerged (Strauss & Corbin, 2014).
Results
Within the group of eleven expert rehabilitation nurses, nine were women. The average age was 42.27 years. More than half the experts (six) had over fifteen years of work experience, three had ten years, one nurse had twelve years, and another nurse had six years. All experts worked on functional rehabilitation units in either inpatient or community contexts and were recognized by their peers as having an outstanding nursing resume.
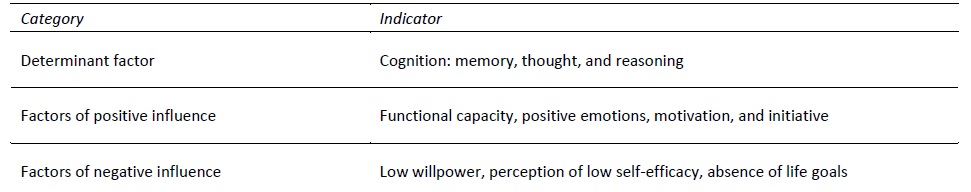
From the participants’ perspective, the nursing diagnostic labels that were indicative of the need for care for a person with functional dependence included self-care deficit or potential to improve self-care abilities. Moreover, nurses’ decision-making was dependent on 1) factors influencing the potential to improve self-care abilities of a person with functional dependence, 2) the domain of influence of these factors, and 3) three fundamental aspects to consider when evaluating a person with functional dependence The factors that influence a person with functional dependence to improve self-care abilities are (a) functional capacity that includes cognitive and physical issues, (b) emotional factors, and (c) support system, which includes family members, health professionals, time, and environment (table 2).
Table 2 Factors that influence the potential to improve self-care abilities of a person with functional dependence
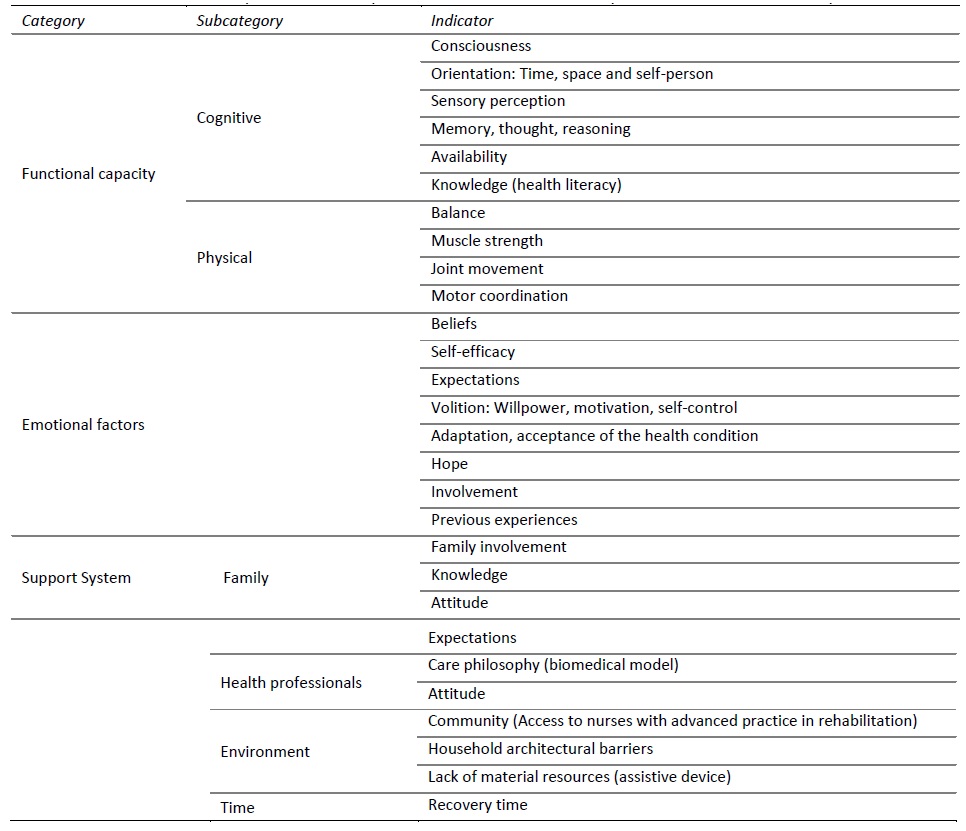
The presence of severe cognitive impairment (caused by memory, thought, or reasoning alterations) is a determining factor for nurses’ clinical decision-making processes, leading them to opt for the diagnostic label self-care deficit. Unaltered functional capacity, positive emotions, motivation, and initiative, positively influence the recovery process of a dependent person's self-care abilities. These indicators suggest that a nurse should opt for the diagnostic label potential to improve self-care abilities. Low willpower, perception of low self-efficacy, and the absence of life goals were considered factors that negatively influence a person's recovery process. These indicators reflect the reduced potential for the recovery of self-care abilities and are likely to lead to deficit in self-care, leading to nurses deciding on interventions that often replace the person in self-care actions (table 3).
Expert nurses consider that the assessment of the ability of a person with functional dependence must take into account three of the following aspects (a) the timing of the assessment, with the results guiding the level of assistance in health care; (b) the indicators for assessment, which inform the rigor of nurses' decision-making and monitor the effectiveness of a person's response during the autonomy recovery process; and (c) systematic in the evaluation, which facilitates the readjustment of nursing interventions and respective expected outcomes.
Discussion
The present study sought to identify the assumptions used by expert nurses when formulating the clinical judgment of self-care deficit versus the potential to improve self-care. Evaluating whether or not a person has the potential to improve self-care ability involves specific criteria. A preserved cognitive function is essential to receive, decode, and retain information (Bidwell, 2015). Duff et al. (2007) demonstrated that impaired functional and cognitive capabilities negatively affect a person's ability and interest to be involved in self-care activities, which may make the assessment particularly challenging.
Functional capacity reflects the difficulties that a person may experience when performing a task or action that requires a specific cognitive status, which includes awareness, orientation, sensory perception, memory, thought, reasoning, and knowledge (information acquired and/or perceived). According to Jaarsma et al. (2017), a person needs to have specific functional and cognitive skills to become involved in self-care, including making choices, identifying care needs, and knowing how to contact a healthcare professional when necessary. Hence, a person needs to have a certain degree of involvement in their care process and commit to their health and well-being. Functional capacity also includes physical status, a category identified in our study. Thus, muscle strength, motor coordination, balance, and joint movement “[...] are body processes that, after being evaluated, are used to determine whether or not a person will evolve to independence” (N1). However, “[...] it was more important to understand the difficulties a person faces when performing self-care activities (washing the back, dressing from the waist down, oral hygiene) [...] despite impairment [...]" (N9). “People with these types of deficits, experiencing them for a long time due to chronic disease situations, often adopt strategies to perform self-care activities different from those they had before [...]” (N4).
Emotional factors were a category that emerged from this study and included multiple indicators showing how a person goes through the rehabilitation process of functional capacity. Most of the expert nurses reported that functional capacity conditions the process of self-care recovery of a dependent person. Moreover, hindering beliefs, or changes in the perception of self-efficacy and demotivation, can indicate a state of “[...] I can, but I do not want to, because I am in a denial phase [...]” (N5). On the other hand, having expectations, motivation, and being involved is essential “[...] for the adaptation of the current health condition and improvement in self-care autonomy” (N9). Being focused on the recovery of their individual capacities helps a person in the recovery process. These opinions corroborate the results of several studies that demonstrate the influence that emotional factors have on a person's involvement during the process of regaining self-care abilities (Chang et al., 2017; Silva, 2019). Hope is also a type of emotion that, once present, allows a person to deal with a stressful situation more effectively (Pinto et al., 2012). It assumes a therapeutic role, stronger than optimism, and is a relevant coping strategy with influence over a person's well-being.
Other influencing factors reported by the participants were previous experiences. Previous experiences are used as effective pattern identifiers that provide relevant clues, suggest expected outcomes associated with specific responses, and point to reasonable objectives and actions in certain situations (Jaarsma et al., 2017). However, they may also be potent inhibitors of the development of the ability to improve self-care, as described by one experienced nurse, “I am dealing with a person who, due to a previous negative experience, does not currently want to be trained on how to transfer from bed to chair, because he fell during their previous hospitalization” (N11). The challenge for nurses is to identify whether previous experiences facilitate other moments of assessment and the develop the ability to perform self-care. These professionals “[…] have a field of action that allows them to understand the experiences and adapt them to improve individual performance abilities [...]” (N5). Within this domain of emotional factors, moral principles and beliefs have also emerged, attributing more meaning to life, organizing, and mentally building a balance of reality (Lourenço, 2015).
The support system category was structured into four subcategories: family, health professionals, environment, and time factors. Family is considered cardinal support for a dependent person (Chen et al., 2017). Family support increases participants' involvement and confidence in the process of regaining autonomy and proves to be a facilitating resource to develop appropriate self-care abilities and behaviors (Lourenço, 2015; Riegel et al., 2017). Caring for a family member with functional dependence is a lingering, painful reality within the family context (Chen et al., 2017). Often “[...] the lack of family resources affects the underutilization of health services due to the prolonged delay of a patient's discharge [...]" (N1). However, “[...] the type of family caring for the dependent person has a strong influence” (N8). Within their caregiver role, family members must get actively involved, be empathetic, and available to improve their knowledge. “Sometimes we are faced with family caregivers who do not want the dependent person to be autonomous [...] often replacing them in their activities, like dressing, bathing, eating and even choosing their clothes. These family members consider that the best way to show affection is for them to replace their family member in his/her daily life activities [...]” (N8).
According to expert nurses, the philosophy of care and healthcare professionals' attitude can influence a person with functional dependence to develop self-care abilities. When guided by a biomedical model, nurses consider that the maintenance of body processes, management of signs and symptoms, and therapeutic prescriptions are priority areas. “What we want is for the person to keep the body processes functioning and not develop pressure ulcers, for example” (N6). However, a person-centered care model should guide experts’ decision-making. The psychological and emotional aspects must be included and should be considered significant areas in the recovery process of a person with functional dependence (Dineen-Griffin et al., 2019; Lourenço, 2015). This is confirmed by one nurse (N8) participating in our study “[...] in addition to the domain of body processes, other equally important factors such as emotional aspects, need to be considered when formulating a diagnostic judgment of a person with the potential to improve self-care abilities.” According to the nurses in our study, it is essential to adopt a motivating attitude when caring for a person with functional dependence, promoting self-efficacy and empowerment to regain autonomy. Nurses must be available, attentive, and curious to explore the person's perspectives, interests, and needs. The study experts considered language and attitude extremely important: "The language we use with [people with functional dependence] cannot be pressing, vigorous or focused exclusively on obligations or even on guilt [...]" (N4). “The nurse with advanced training is more confident in the therapeutic relationship they establish with a person.” (N1). "It is important that each of us choose attitudes that help a person improve their self-efficacy [...]" (N11).
The environment also influences the ability of a person with functional dependence to improve self-care. Architectural barriers that interfere with accessibility at home can negatively impact a person’s rehabilitation process, hindering the recovery of autonomy (Lee et al., 2018). The lack of material resources such as assistive devices was found to hinder the process of a healthy transition to improve autonomy in self-care (Roelands et al., 2002). Residency areas covered by regular nurse home visits increased “[...] the perception of patients and family caregiver regarding the home-care formal support of health professionals” (N9). Sharing experiences within peer groups, the patient's contact with people who have lived similar situations and the results achieved, were found to increase involvement in the process of acquiring skills because people felt that it was possible to overcome the situation (Lourenço, 2015). Nurses participating in this study also considered that recovery time was associated with the opportunity for recovery varying according to each person. “We sometimes are in such a hurry that we do not give people with functional dependence a chance to carry out activities of daily living autonomously” (N10). “The worsening of the disease and the functional capacity means that a person needs more time to perform self-care actions” (N5).
Three domains of influence of the mentioned factors in the improvement potential of a person with functional dependence were identified: the determinant factor, positive influencers, and negative influencers. Self-care is a learned process, and cognition is a determinant factor. Therefore, self-care is limited to focused attention, memory, and reasoning abilities to understand and process the information given before making a decision. In other words, self-care in chronic illness should be reasoned (Riegel et al., 2012). Self-care is consensually considered an activity acquired throughout the lifespan and oriented toward improving a person's well-being. Self-care is also influenced by age, gender, culture, education, and socio-economic status (Jaarsma et al., 2017). In people with chronic illness, self-care becomes limited and influenced by other factors, which can be divided into two dimensions -positive influencers and negative influencers (Schulman-Green et al., 2016). For example: “[...] functional capacity, positive emotions, motivation, and initiative [...] are factors that support the recovery process of self-care abilities [...]” (N2). On the other hand, “[...] low willpower, perception of low self-efficacy, reduced life goals [...], are hindering factors [...]” (N5). However, these factors should not prevent the potential to improve self-care abilities as this is one of nurses’ main priority, “[...] somehow, we can help a person to manage negative emotions [...]” (N2).
As mentioned above, the experts enunciated three of the following essentialas aspects to be considered when assessing a person with functional dependence: time of assessment, assessment indicators, and systematic in the evaluation. The timing of the evaluation is crucial since health conditions change. "A person that currently has the capacity for recovery, might, after a few days, have another [...]” (N6) assessment outcome. The ideal moment for recovery is after the acute phase of the disease has stabilized. The recovery process is drawn and indicates the need for another level of assistance in healthcare. The first assessment must not be hastened. Getting an indicator of the absence of functional capacity at any given time can be discriminatory for a person and may delay the recovery process. This decision must be subject to more than one assessment and based on result indicators. “We often have to argue on after how long do we go back to reassess?” (N8). The definition of outcome indicators is critical to guide and standardize nurses’ decision-making during the process of recovering the capacity of a person with functional dependence. Experts also consider the systematic in the evaluation as an essential aspect and also emphasize the importance of monitoring the response patterns during the process of regaining autonomy in self-care of a dependent person allowing the emergence of a strategy for targeted care management to be identified (Voils et al., 2012).
Conclusions
The systematic in the evaluation of the self-care abilities of a person with functional dependence is fundamental, mainly due to the complexity of the diagnosing recovery potential and the multiplicity of factors that influence the recovery process. The present study sought to identify the assumptions used by expert nurses when formulating the clinical judgment of self-care deficit versus the potential to improve self-care . It is crucial to understand that support in self-care recovery comprises a set of factors that involve neuromuscular, psychological, social, and contextual aspects. These factors could have positive or negative influence to initiate and/or to continue the recovery process. This study stresses the importance of not focusing only on the physical domain but on wider personal factors that influence the recovery process, as shown by the identified categories-emotional factors and support systems. Our results also emphasize the analysis of all these components as important indicators to the self-care improvement process.
On the one hand, this process implies that a person is motivated, has willpower, and believes in their self-ability to develop adaptive strategies. Of the author's opinion, professionals need to be guided by a person-centered model and not a model that replaces the dependent person in self-care activities. The systematic in the evaluation has emerged as another key factor as it enables us to determine the necessary conditions and monitor the progress of a person's potential to acquire, develop, and/or improve the ability to perform self-care activities. The health professional must consider whether the person needs more time to perform self-care activities. Additionally, the family plays a vital role within this team and, consequently, in the reshaping the dependent person’s autonomy. Their active role in the recovery process and the adoption of a new mindset are determinants for the development of self-care abilities and behaviors. New studies are recommended to consolidate the results obtained.