Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Portuguesa de Enfermagem de Reabilitação
Print version ISSN 2184-965XOn-line version ISSN 2184-3023
RPER vol.1 no.1 Silvalde June 2018
https://doi.org/10.33194/rper.2018.v1.n1.06.4392
Articles
PULMONARY REHABILITATION IN PATIENTS WITH BRONCHIECTASIAS NON-CYSTIC FIBROSIS: QUALITY OF LIFE, ANXIETY AND RESPIRATORY FUNCTION
Bronchiectasis (BQ) are abnormal and irreversible dilations of the bronchi that increased production of secretions and respiratory infections and can interfere in the Quality of life (QOL).
The essay aimed to evaluate the effect of a pulmonary rehabilitation program (PRP) on QOL, Anxiety and Respiratory Function (RF) in people with BQ.
Prospective, quantitative and exploratory study including people with bronchiectasis admitted for pulmonary rehabilitation (PR). Data collection regarding QOL, Anxiety and RF performed before and after PRP.
It included 30 people (39.1% men); mean age of 53.3 years. Statistically significant improvements were found in the QOL, (p = 0.003, p = 0.005, p = 0.005) and anxiety (p = 0.001). No significant results were found in RF.
The results of this study allow us to conclude that RR improves QOL, reduces anxiety and does not alter PF in people with non-cystic fibrosis bronchiectasis.
Keywords: rehabilitation nursing; respiratory rehabilitation; quality of life; anxiety; respiratory function; bronchiectasis
Bronquiectasias são dilatações anormais e irreversíveis dos brônquios que condicionam aumento da produção de secreções e infeções respiratórias de repetição podendo interferir na Qualidade de vida (QV).
O objetivo deste estudo foi avaliar eficácia de um programa de reabilitação respiratória (PRR) na QV, na Ansiedade e na função respiratória (FR) em pessoas com BQ.
Estudo Prospetivo; quantitativo; exploratório que incluiu pessoas com bronquiectasias admitidas para reabilitação respiratória (RR). A Colheita de dados da QV, Ansiedade e FR foi realizada antes e após o PRR.
Incluiu 30 pessoas (39,1% homens); idade média de 53,3 anos. Encontradas melhorias estatisticamente significativas na QV, (Valor global p=0,003; Subescalas Sintomas p=0,065; Atividade p=0,005 e Impactos p=0,019), e na Ansiedade (p=0,001). Não foram encontrados resultados significativos na FR.
Os resultados deste estudo permitem-nos concluir que a RR melhora a QV, reduz a Ansiedade e não altera a FR em pessoas com bronquiectasias não fibrose quistica.
Palavras chave: enfermagem de reabilitação; reabilitação respiratória; qualidade de vida; ansiedade; função respiratória; bronquiectasias
Las bronquiectasias (BQ) son dilataciones anormales e irreversibles de los bronquios que condicionan aumento de la producción de secreciones e infecciones respiratorias de repetición pudiendo interferir en la Calidad de vida (QV).
El objetivo de este estudio fue evaluar el efecto de un programa de rehabilitación pulmonar (PRP) en la QV, la Ansiedad y la función pulmonar (FP) en personas con BQ no relacionada com fibrosis quistica.
Estudio Prospectivo; cuantitativa; exploratorio que incluyó a personas con bronquiectasias admitidas para rehabilitación pulmonar (RP). Los datos de la QV, Ansiedad y FR fueran recogidos antes y después del PRR.
Incluyó 30 personas (39,1% hombres); edad media de 53,3 años. (P = 0,003), y en la ansiedad (p = 0,001), y en la ansiedad (p = 0,001), se observó una mejoría estadísticamente significativa en la QV, (Valor global p = 0,003; Subescalas Síntomas p = 0,065; Actividad p = 0,005 e Impactos p = 0,019). No se encontraron resultados significativos en la FR.
Los resultados de este estudio nos permiten concluir que RP mejora la QV, reduce la Ansiedad y no altera la FP en personas con bronquiectasias no relacionada com fibrosis quistica.
Palabras clave: rehabilitación pulmonar; calidad de vida; ansiedad; función pulmonar; bronquiectasias
INTRODUCTION
Bronchiectasis is characterized by an abnormal, permanent and irreversible dilation of the bronchi caused by the destruction of the elastic and muscular components of its walls and deficient mucociliary clearance 1-2.
Associated with dyspnea, activity intolerance and coughing, bronchial hypersecretion is its main characteristic, presenting a high morbidity due to the recurrence of respiratory infections 3.
The progressive intensity of dyspnea, effort intolerance, presence of abundant secretions and the recurrence of infections lead to the need to change one's lifestyle, which is not always successful 4-5.
The impact of bronchiectasis in these people's lives does not only occur in the physical component. In addition to the inability, greater or lesser, to perform activities of daily living, the effect of the disease is also felt in the social and affective perspective, with anxiety being a very frequent finding with even more pressing effects on quality of life 6-7.
Respiratory Rehabilitation, a multidisciplinary approach in the treatment of people with chronic respiratory disease, is fundamental in the therapeutic management process of people with Chronic Obstructive Pulmonary Disease (COPD) 8-9)(8) (9. Although it is a clinical entity distinct from COPD, people with bronchiectasis are also characterized by an obstructive ventilatory pattern and by the possibility of dyspnea, fatigue, cough, bronchorrhea, and decreased exercise tolerance. These symptoms make respiratory rehabitation also recommended in the treatment of this disease 4,8-9.
Few studies have been carried out to study the impact of pulmonary rehabilitation and its benefits in patients with bronchiectasis, when compared with the high scientific production on COPD 7.
In this sense, having Nursing Care as the focus of attention, it reveals itself as an object of current interest for the Nursing discipline to assess the impact of its practice.
Only in this way will it be possible to sustain the importance of Nursing in general and specialized care in Rehabilitation Nursing, in particular, in clinical practice, in health policies and in teaching as a discipline of knowledge.
Thus, the present essay aimed to evaluate the effect of a Respiratory Rehabilitation Program on the quality of life, anxiety and respiratory function of people with non-cystic fibrosis bronchiectasis.
METHOD
The question that guided this study was: How does respiratory distress disturb and affect the lives of people with Bronchiectasis?
From this central question, three research questions were formulated, which we intend to answer:
How respiratory rehabilitation interferes with the quality of life of people with bronchiectasis;
How respiratory rehabilitation interferes with the anxiety of people with bronchiectasis;
How respiratory rehabilitation alters the respiratory function of those with bronchiectasis.
It was a prospective, quantitative and exploratory study, with intra-subject evaluation in two moments, carried out with a sample of people with non-cystic fibrosis bronchiectasis undergoing a respiratory rehabilitation program.
The sampling technique used was non-probabilistic and of convenience.
The inclusion criteria were expressing a desire to participate in the study and filling out an informed consent, being over 18 years-old, having communication skills, not being unable to practice physical exercise, and not having severe cognitive impairment.
Failure to fully comply with the PRP, inability to exercise, and psychiatric illness or cognitive dysfunction were exclusion criteria from the study.
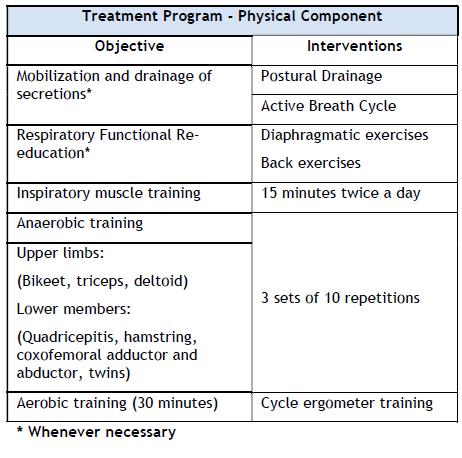
The respiratory rehabilitation program was carried out on an outpatient basis for 13 weeks and 3 times a week. It consisted of a physical component that included high-intensity exercise training, inspiratory muscle strengthening and respiratory functional re-education (figure 1) and an educational component (figure 2).
The variables under study were Quality of life, Anxiety, and Respiratory Function, and data collection was performed at the beginning and at the end of the respiratory rehabilitation program.
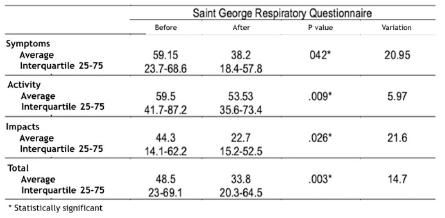
Data related to the variable Quality of life were obtained using The St. George's Respiratory Questionnaire (SGRQ), which is a specific questionnaire for people with chronic respiratory disease and consists of three subscales: symptoms, restrictions in daily activities and impact of the disease on the individual. Each subscale has a maximum possible score, with variations of 10% (relative to the standard) indicating a change in quality of life. Changes greater than 4% after an intervention indicate a significant change in quality of life 10.
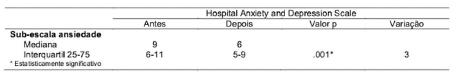
Anxiety variables were assessed using the Hospital Anxiety and Depression Scale (HADS). This scale consists of two subscales whose sum of scores identifies the level of anxiety and depression. A cut-point of eight was used, with higher scores showing anxiety and/or depression 11.
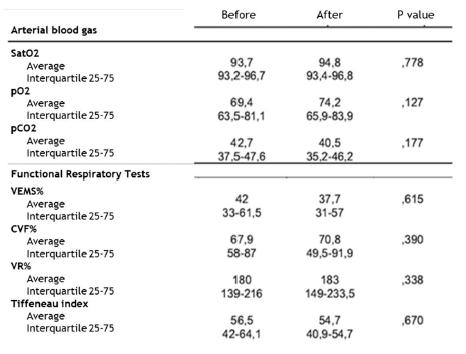
The Respiratory Function variable was evaluated by performing respiratory function tests and arterial blood gases.
Statistical analysis
In the statistical analysis of the data we used the IBM SPSS version 23.0 software.
In a first phase, with a view to describing and characterizing the sample under study, a descriptive analysis of the data was carried out according to the nature of the variables under study, performing an exploratory univariate analysis of the data, using measures of central tendency, of dispersion, flattening and symmetry, existence of outeliers and the normality of distributions.
In a second phase, in order to assess the effectiveness of the pulmonary rehabilitation program in "Quality of Life", "Anxiety” and "Respiratory Function", the nonparametric Wilcoxon test was used for two paired samples due to the small number of the sample in study.
All tests were applied with a confidence level of 95%.
Ethical aspects
In the methodological path, respect for all deontological presuppositions inherent to the ethics of research was guaranteed, as well as the guarantee of maximum confidentiality in the subsequent phases of collecting and processing information.
The study was presented, explaining the objectives, investigation time, the purposes of the results and the possibility of giving up at any stage, obtaining informed consent and guaranteeing data secrecy and confidentiality.
The application of the questionnaires was authorized by the ethics committee.
RESULTS
Thirty participants were included in the study, most of them female (60.9%), 39.1% male, with a median age of 53.3 (± 16.7) years-old.
For a better explanation of the results obtained, we will proceed with the individual analysis of each of the variables under study.
Total Scale
A difference of -14.7 points was observed after respiratory rehabilitation compared to baseline values (before value=48.5; after value a=33.8). Statistically significant differences were found in the total value of the scale (p=0.003) (Figure 5).
Score of the Subscales "Symptoms", "Activities", "Impact".
After the rehabilitation program, participants expressed statistically significant improvements in all dimensions evaluated.
Clinically significant improvement (score variation greater than 4) was also found in the Total Scale and in all subscales.
Anxiety
The results show that regarding “Anxiety”, statistically significant differences were found (p = 0.001) when comparing the results of the questionnaires before and after the rehabilitation program. The variation between the two evaluations being 3 points. (Figure 6)
DISCUSSION
This study aimed to evaluate the effect of a respiratory rehabilitation program on quality of life, anxiety and respiratory function in people with bronchiectasis.
The global interpretation of the data collected by this investigation demonstrated the achievement of clear benefits, namely in terms of reducing levels of anxiety and increasing quality of life. On the other hand, regarding the respiratory function, the data collected show that there is no statistically significant improvement.
To facilitate the discussion, we will go to the research questions formulated:
1. How does pulmonary rehabilitation interfere with the quality of life of patients with bronchiectasis?
Bronchiectasis has been described as an orphan disease of the airways.1,12 Two decades later, very little investigation was carried out into the efficacy of most treatments performed, including pulmonary rehabilitation.3,6,13
On the other hand, respiratory rehabilitation that initially emerged as a treatment recommendation for people with chronic obstructive pulmonary disease is now mandatory in the treatment of other chronic respiratory diseases including bronchiectasis.8,12
Exercise patterns combined with self-care constitute an effective and highly effective intervention, leading to a reduction in exacerbations with a subsequent reduction in hospitalization and an increase in quality of life.5,14
Although different entities, bronchiectasis and COPD have considerable similarities, both in terms of pulmonary involvement and also in terms of peripheral muscles, tolerance to effort, nutritional status and impact on quality of life.3,12-13
Santomato in 2012 confirms the effectiveness of pulmonary rehabilitation programs in people with bronchiectasis and states that their impact on quality of life is as effective as in patients with COPD.14
In a retrospective study in 2011 Ong et al. demonstrates that respiratory rehabilitation in people with bronchiectasis significantly increases exercise tolerance as well as quality of life, being comparable with the group of patients with COPD undergoing the same rehabilitation program.15
Different levels of respiratory dysfunction can be found in patients with bronchiectasis, which can be translated into obstructive, restrictive or mixed.16 According to the results obtained, the sample presented mild obstruction in the large airways and severe obstruction in the small airways. These results suggest that data on the respiratory function of patients with bronchiectasis show that there is airflow limitation, probably due to chronic inflammation or destruction of the bronchial wall.3,12
In our study, respiratory dysfunction translated a moderate obstructive pattern with mean values at the beginning of the treatment of FEV1 and the Tiffeneau index of 47.2 and 53.7, respectively.
The quality of life assessment revealed a clinically significant improvement (( greater than 4 points) in the total scale score of 8.73, as well as in the scores of each of the three subscales: symptoms 9.40; activity 9.01 and impacts 8.40.
The data obtained reveal a total score of 48.4 (± 23.1) and partial scores of 62.9 (± 24.9) for the Activity subscale, 49.4 (± 25.3) for the Symptoms and subscale 39.7 (± 23.8) for the Impact subscale.
These values are globally lower than those reached by Martinez-Garcia in 200517 This variation can be explained by the mean value of FEV1 in this study (60 ± 19.4) being much higher than that presented in our study (FEV1 47.2 ±19.9) reflecting a lower degree of obstruction.17
The inclusion of inspiratory muscle training in our rehabilitation program is in line with the work of Newall in 2005, who concluded that people undergo respiratory rehabilitation programs simultaneous to inspiratory muscle training did not show advantage, but may however be importante in the longevity of the training effects. The result of this study was a very significant improvement in quality of life, translated into an average increase of 7.7 points in the total score, maintaining these results for a period of 3 months after the end of the program.18
2. How does pulmonary rehabilitation interfere with the anxiety of patients with bronchiectasis?
The results obtained in our study show a statistically significant reduction in anxiety values between the beginning and the end of the respiratory rehabilitation program.
However, no significant difference was found between the degree of pulmonary obstruction (measured by FEV1%) and anxiety, which suggests that the severity of the lung disease, regarding the impact on anxiety, is related to subjective aspects and individual experiences of each person.19
Anxiety as a clinical entity has been included in the main studies carried out in patients with chronic pulmonary pathology carried out in recent years, since it was found that the prevalence of anxiety disorders among people with chronic respiratory pathology is higher than that of the general population. 20 The explanation may lie in situations of hyperventilation and dyspnea symptoms that are characteristic of panic attacks and lack of control, as well as respiratory pathology with an obstructive pattern.19
Dyspnea is the most limiting symptom in people with obstructive pulmonary pathology and may also be considered the most important to determine the impact of the disease on quality of life. In fact, there is a close relationship between dyspnea, or rather, the fear of triggering an episode of dyspnea and anxiety.21-23
There is a broad base of consensus about the fundamental role of respiratory rehabilitation in the management of chronic obstructive respiratory disease, not only because it reduces anxiety, but especially because it reduces dyspnea and fatigue, increases exercise tolerance, thus increasing the quality of life.
Coventry published in 2007 a systematic review which concluded that pulmonary rehabilitation programs with three sessions per week that include physical exercise programs and educational programs reduce mild to moderate anxiety in patients with COPD GOLD C.24
Our investigation concluded that there is a significant improvement in anxiety after the pulmonary rehabilitation program, with an average reduction of approximately two points in the HADS scale, placing the total result in the sample at a value lower than the cutoff point of the scale.
3. How does pulmonary rehabilitation interfere with the respiratory function of patients with bronchiectasis?
Bronchiectasis is the pathological expression of a wide variety of diseases.1
They are characterized by airflow obstruction, coughing, sputum, recurrent respiratory infections, dyspnea associated with decreased quality of life and reduced exercise tolerance.14 As in COPD, the causes of dyspnea and reduced exercise tolerance they are multifactorial, including ineffective gas exchange, loss of muscle mass, and the presence of large amounts of mucus.13,16
Since bronchiectasis is characterized by a deficiency in mucociliary clearance, airway clearance techniques are widely advocated as a fundamental part of these people's daily routine.2
Airway impaction with considerable amounts of sputum is associated with atelectasis, as well as deterioration of respiratory function and blood gas values, which improve with the mobilization of secretions or aspiration. However, the relationship between the removal of bronchial secretions and the improvement in respiratory function is not fully established yet.25
There is very little scientific evidence that proves the change in respiratory function caused by respiratory rehabilitation programs before increasing the amount of mucus expelled, not changing the FEV1 values.4,15
Mandal et al., in 2012, published a study of 30 patients with bronchiectasis of non-pulmonary fibrosis etiology, undergoing an 8-week, bi-daily program of pulmonary rehabilitation and concluded that there was no improvement in the values of FEV1, FCV, IT.26
Murray in 2009 concluded in a study of 20 patients with bronchiectasis of non-pulmonary fibrosis etiology that there was no variation in the values of FEV1, FVC, FEF25-75%, MIP, MEP or exacerbations when undergoing a 12-week rehabilitation program. However, this program was slightly different from the one presented in our study as it included sessions twice a day.27
Newall, in 2005, studied 32 patients with bronchiectasis of idiopathic etiology and concluded after an 8-week rehabilitation program, 3 times a week, that there were no statistically significant changes in the values of FEV1, FVC, IT, RV, TLC.18
Santomato published a study with a very small sample (3 patients) and a pulmonary rehabilitation period of 20 weeks, 3 times a week, also reaching the conclusion that there are no significant differences between the spirometric values.14
Van Zeller, in a cohort of 41 patients over a 12-week period, 3 times a week, concluded that there is a positive impact of pulmonary rehabilitation on lung function in certain groups of patients with bronchiectasis.25
Our study does not find statistically significant gains in respiratory function after the pulmonary rehabilitation program; it did not find statistically significant differences in the values of FEV1%, FVC%, VR%, IT%, TLC%.
Regarding arterial blood gas values, there were no statistically significant variations in PaO2, PaCO2, SatO2 values.
CONCLUSION
The data obtained in this study allow us to conclude that pulmonary rehabilitation improves quality of life, significantly reduces anxiety and does not alter respiratory function in people with bronchiectasis.
In conclusion, the results achieved allow us to clearly infer that a respiratory rehabilitation program, in which the principles of exercise prescription and behavioral change were derived from COPD, is a valid approach also for people with non-cystic fibrosis bronchiectasis, and may represent one of the few treatments available with the potential to modify the course of the disease and its prognosis, being an unexpensive addition to existing medical care.
However, further investigations, namely randomized controlled trials, are needed to optimize training programs while maintaining long-term benefit.
REFERENCIAS
1 Amorim A, Róldan JG. Bronquiectasias: será necessária a investigação etiológica?. Rev Port Pneumol. 2011 Jan 1;17(1):32-40. [ Links ]
2 Zanini A, Aiello M, Adamo D, Cherubino F, Zampogna E, Sotgiu G, Chetta A, Spanevello A. Effects of pulmonary rehabilitation in patients with non-cystic fibrosis bronchiectasis: a retrospective analysis of clinical and functional predictors of efficacy. Respiration. 2015;89(6):525-33. [ Links ]
3 McShane PJ, Naureckas ET, Tino G, Strek ME. Non-cystic fibrosis bronchiectasis. Am J Respir Crit Care Med. 2013 Sep 15;188(6):647-56. [ Links ]
4 Pasteur MC, Bilton D, Hill AT. British Thoracic Society guideline for non-CF bronchiectasis. Thorax. 2010 Jul 1;65(Suppl 1):i1-58. [ Links ]
5 Lee AL, Hill CJ, McDonald CF, Holland AE. Pulmonary Rehabilitation in Individuals With Non-Cystic Fibrosis Bronchiectasis: A Systematic Review. Arch Phys Med Rehabil. 2017 Apr 1;98(4):774-82. [ Links ]
6 Niksarlioglu EY, Özkan G, Günlüoglu G, Uysal MA, Gül S, Kilic L, Yeter A, Çamsari G. Factors related to depression and anxiety in adults with bronchiectasis. Neuropsychiatr Dis Treat. 2016;12:3005-10. [ Links ]
7 Kelly C, Spencer S, Grundy S, Lynes D, Evans DJ. Self-management for non-cystic fibrosis bronchiectasis. The Cochrane Library. 2017 Jan 31. [ Links ]
8 Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, Hill K, Holland AE, Lareau SC, Man WD, Pitta F. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013 Oct 15;188(8):e13-64. [ Links ]
9 Ferreira D, Teodoro A, Gaspar L, et al. Guia Orientador de Boa Prática - Reabilitação Respiratória. Lisboa: Ordem dos Enfermeiros. 2018. [ Links ]
10 Jones PW. St George's Respiratory Questionnaire Manual. London: St George's, University of London. 2009 Junho. [ Links ]
11 Pais-Ribeiro J, Silva I, Ferreira T, Martins A, Meneses R, Baltar M. Validation study of a Portuguese version of the Hospital Anxiety and Depression Scale. Psychol Health Med. 2007 Mar 1;12(2):225-37. [ Links ]
12 Maiz Carro L, Diez M. Manual de Bronquiectasias. Neumo. 2009; 1: 9-17. [ Links ]
13 Holland AE, Wadell K, Spruit MA. How to adapt the pulmonary rehabilitation programme to patients with chronic respiratory disease other than COPD. Eur Respir Rev. 2013;22(130):577-86. [ Links ]
14 Santamato A, Ranieri M, Panza F, Frisardi V, Marvulli R, Filoni S, Cisari C, Fiore P. Pulmonary rehabilitation for patients with bronchiectasis. Eur J Phys Rehabil Med. 2012 Jun;48(2):293-8. [ Links ]
15 Ong HK, Lee AL, Hill CJ, Holland AE, Denehy L. Effects of pulmonary rehabilitation in bronchiectasis: a retrospective study. Chronic Respir Dis. 2011 Feb;8(1):21-30. [ Links ]
16 Drain M, Elborn J. Assessment and investigation of adults with bronchiectasis Monograph ER, editor.; 2011. [ Links ]
17 Martínez-García MA, Perpiñá-Tordera M, Román-Sánchez P, Soler-Cataluña JJ. Quality-of-life determinants in patients with clinically stable bronchiectasis. Chest. 2005 Aug 1;128(2):739-45. [ Links ]
18 Newall C, Stockley RA, Hill SL. Exercise training and inspiratory muscle training in patients with bronchiectasis. Thorax. 2005 Nov 1;60(11):943-8. [ Links ]
19 Gao YH, Guan WJ, Zhu YN, Chen RC, Zhang GJ. Anxiety and depression in adult outpatients with bronchiectasis: Associations with disease severity and health-related quality of life. Clin Respir J. 2018 Apr;12(4):1485-94. [ Links ]
20 Moreno RM, Vasconcelos GF, Cisneros C, Gómez-Punter RM, Calvo GS, Ancochea J. Presence of anxiety and depression in patients with bronchiectasis unrelated to cystic fibrosis. Arch Bronconeumol. (English Edition). 2013 Oct 1;49(10):415-20. [ Links ]
21 Yohannes AM, Junkes-Cunha M, Smith J, Vestbo J. Management of Dyspnea and Anxiety in Chronic Obstructive Pulmonary Disease: A Critical Review. J Am Med Dir Assoc. 2017 Dec;18(12):1096-e17. [ Links ]
22 Olveira C, Olveira G, Gaspar I, Dorado A, Cruz I, Soriguer F, Quittner AL, Espildora F. Depression and anxiety symptoms in bronchiectasis: associations with health-related quality of life. Qual Life Res. 2013 Apr 1;22(3):597-605. [ Links ]
23 Halpin D, Hyland M, Blake S, Seamark C, Pinnuck M, Ward D, Whalley B, Greaves C, Hawkins A, Seamark D. Understanding fear and anxiety in patients at the time of an exacerbation of chronic obstructive pulmonary disease: a qualitative study. JRSM open. 2015 Nov 18;6(12):2054270415614543. [ Links ]
24 Coventry PA, Hind D. Comprehensive pulmonary rehabilitation for anxiety and depression in adults with chronic obstructive pulmonary disease: systematic review and meta-analysis. J Psychosom Res. 2007 Nov 1;63(5):551-65. [ Links ]
25 van Zeller M, Mota PC, Amorim A, Viana P, Martins P, Gaspar L, Hespanhol V, Gomes I. Pulmonary rehabilitation in patients with bronchiectasis: pulmonary function, arterial blood gases, and the 6-minute walk test. J Cardiopulm Rehabil Prev. 2012 Sep 1;32(5):278-83. [ Links ]
26 Mandal P, Sidhu MK, Kope L, Pollock W, Stevenson LM, Pentland JL, Turnbull K, Mac Quarrie S, Hill AT. A pilot study of pulmonary rehabilitation and chest physiotherapy versus chest physiotherapy alone in bronchiectasis. Respir Med. 2012 Dec 1;106(12):1647-54. [ Links ]
27 Murray MP, Pentland JL, Hill AT. A randomised crossover trial of chest physiotherapy in non-cystic fibrosis bronchiectasis. Eur Respir J. 2009 Nov 1;34(5):1086-92. [ Links ]
Received: May 29, 2018; Accepted: June 20, 2018; Published: June 23, 2018











 text in
text in