Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista Portuguesa de Enfermagem de Reabilitação
versão impressa ISSN 2184-965Xversão On-line ISSN 2184-3023
RPER vol.2 no.1 Silvalde jun. 2019
https://doi.org/10.33194/rper.2019.v2.n1.02.4571
Articles
Nursing Rehabilitation in the prevention of falls in the elderly people at home
1- ULSLA - Hospital do Litoral Alentejano, Serviço de Ortopedia
2- ULSLA - Centro de Saúde de Sines, UCC1
Objective:
To identify intrinsic and extrinsic factors associated with the risk of fall in the elderly people at home; To analyse the result of rehabilitation nursing care on decreasing the risk of fall in the elderly people at home.
Methodology:
Descriptive case study with three participants who are patients that are integrated into long-term care team unit integrated in the community care, with neurological and balance changes, targets of rehabilitation nursing care with potential for recovery.
Results:
During eight weeks of implementation of the rehabilitation nursing care program, there was a decrease in intrinsic risk factors for falls, related to balance, transfers and mobility. When evaluating the results obtained it is possible to observe that all the participants obtained gains. In all cases there were gains in the ability of the participants to perform your daily living activities the in 45 points and an increase in the Equilibrium of 42 points. The evolution in the degree of dependence occurred only in one case, and in the other two cases, severe dependence was maintained.
Conclusion:
The rehabilitation nursing care produce gains in balance and decreased dependency which consequently reduces the risk of fall in the elderly at home. The rehabilitation nursing at home in subacute phases of neurological disease can enhance these results.
Keywords: Rehabilitation nursing; Elderly people; Falls
Objetivo:
Identificar fatores intrínsecos e extrínsecos associados ao risco de queda em idosos no domicílio; Analisar o resultado de cuidados de Enfermagem de Reabilitação na diminuição do risco de queda em idosos no domicílio.
Métodos:
Estudo de caso descritivo com três participantes que são utentes integrados na Equipa de Cuidados Continuados Integrados de uma Unidade de Cuidados na Comunidade, com alterações do foro neurológico e com alteração do equilíbrio, alvos de cuidados de enfermagem de reabilitação, e com potencial de recuperação.
Resultados:
Durante oito semanas de implementação do programa de cuidados de enfermagem de reabilitação verificou-se a diminuição de fatores de risco intrínsecos para queda, relacionados com o equilíbrio, com as transferências e com a mobilidade. Ao avaliar os resultados obtidos é possível observar que todos os participantes obtiveram ganhos. De uma forma geral, em todos os casos houve ganhos na capacidade dos participantes executarem as AVD’s (IB) em 45 pontos e um aumento do Equilíbrio (EEB) de 42 pontos. A evolução no grau de dependência ocorreu apenas em um caso, sendo que nos restantes dois manteve-se a dependência grave.
Conclusão:
Os cuidados de enfermagem de reabilitação indiciam produzir ganhos no equilíbrio e na capacidade de execução dos autocuidados, o que consequentemente diminui o risco de queda em idosos no domicílio. A enfermagem de reabilitação no domicílio nas fases subagudas da doença neurológica pode potencializar estes resultados.
Descritores: Reabilitação; Idoso; Acidentes por Quedas
Objetivo:
Identificar factores intrínsecos y extrínsecos asociados a riesgos de caídas en ancianos en el hogar; Analizar el resultado de cuidados de enfermería de rehabilitación en la disminución de los riesgos de caídas de los ancianos en el hogar.
Métodos:
Estudio de caso descriptivo con tres participantes que son pacientes que están integrados en el equipo de Cuidados Continuados Integrados de la Unidad de Cuidados de la Comunidad, con alteraciones de origen neurológicos y con alteración del equilibrio, objetivo de cuidados de la enfermería de rehabilitación con potencial de recuperación.
Resultados:
Durante ocho semanas de implementación del programa de cuidados de enfermería de rehabilitación se verificó la disminución de factores de riesgos intrínsecos para la caída, relacionados con el equilibrio, las transferencias y la movilidad. Al evaluar los resultados obtenidos es posible observar que todos los participantes obtuvieron ganancias. En general, en todos los casos hubo ganancias en la capacidad de los participantes para ejecutar sus actividades de vida diarias en 45 puntos y un aumento del Equilibrio de 42 puntos. La evolución en el grado de dependencia ocurrió sólo en un caso, siendo que en los restantes dos se mantuvo la dependencia grave.
Conclusión:
Los cuidados de enfermería de rehabilitación producen ganancias en el equilibrio y en la disminución de la dependencia, lo que disminuye el riesgo de caída en ancianos en el domicilio. La enfermería de rehabilitación en el domicilio en las fases subagudas de la enfermedad neurológica puede potenciar estos resultados.
Palabras clave: Enfermería de rehabilitación; Anciano; Caídas
INTRODUCTION
The Rehabilitation Nurse (RN) is the professional with scientific, technical and human competence to provide general and specialized care based on people's real and potential problems, as well as perform therapeutic interventions at the level of neurological, respiratory, cardiac functions, orthopedic and other situations that potentiate disability 1. In this way, the RN seeks to enable the elderly to reach their maximum potential so that they can perform their daily activities, previously limited by the incapacity resulting from the disease 2.
The aging of the population is a phenomenon that has been worsening annually, which is shown by the aging index since 1961 with a growth from 27.5 to 153.2% in 2017, which means that in the year of 2017 there were 153.2 elderly people for every 100 young people (people under 15 years-old) 3.
The aging process entails anatomical and physiological changes that contribute to an increased risk of falls in the elderly. Changes in the visual and vestibular systems; central nervous system; cardiovascular system and musculoskeletal system are the ones that most contribute to this increase. These physiological changes are manifested in, for example, deficit in maintaining body balance and postural control, muscle atrophy and weakness and changes in cognitive functions such as memory, learning and awareness, which contribute either to the increased risk of falling or to the decreased ability to perform activities of daily living (ADL)4. The elderly functionality study carried out in Alentejo (903 participants) concluded that the decline in functionality increases with age, with some functions being preserved until 75 years of age. The data revealed that about 25% of the elderly people had memory disorders that required therapeutic intervention, 15% needed care aimed at hearing deficits, 58% had mostly low back and lower limb pain, 11% needed help in carrying out daily routines and 32.2% needed help to move. Also in the same study, the need for help in self-care varied between 2.8% and 7.5% in activities of elimination and clothing, respectively 5.
In Europe, falls represent one of the main causes of injury in the elderly, with one in every three elderly people suffering a domestic accident each year and one in every two elderly people having a fall at least once a year. Approximately one in five of these falls requires medical care and one in twenty falls results in fracture6. Falls entail consequences responsible for autonomy loss, or even significantly disability which affect elderly people and their caregivers’ quality of life 7.
The General Directorate of Health and the MAPFRE Foundation8 classify the risk factors for falls into two: intrinsic and extrinsic risk factors. Intrinsic factors are related to the person and the physiological aging process and reflect their inability to maintain or recover balance when there is a change in the center of gravity. The extrinsic factors are, in turn, associated with home and leisure environment in which the person is found. At home, the presence of poor lighting, loose carpets, inexistence of handrails in bathrooms or stairs, and slippery pavement enhance the occurrence of accidents.
In this sense, it is essential that there is a set of preventive actions that promote a rehabilitation program with the elderly population with preventive measures for falls, suitable for each user and the respective physiological changes identified. A physical exercise program improves physical performance and reduces the risk of falls by 23% in an active elderly population9. This fact is also corroborated by the authors Daly et al 10, who demonstrate a reduction in falls through muscle strengthening and balance programs, hence why they suggest their implementation at the community level.
The application of this rehabilitation nursing program then emerged from the needs of the target population and the project objectives were: to identify intrinsic and extrinsic factors associated with the risk of falling in the elderly people at home; to analyze the result of rehabilitation nursing care in reducing the risk of falling in the elderly people at home.
METHOD
It is a multiple, descriptive case study 11. It was carried out in the final stage of the Master's Degree in Nursing, specialization area of Rehabilitation Nursing from September to November 2018 in a Community Care Unit (CCU), belonging to the Local Health Unit of the Alentejo Coast (Unidade Local de Saúde do Litoral Alentejano - ULSLA). The participants were selected according to the following criteria: being 70 years old or older, being the target of care by the RN of the CCU, presenting neurological disorders and altered balance.
The data collection was carried out between September 24 and November 16, 2018 and data on the sociodemographic characterization and the health condition/neurological changes of the users were collected in a grid prepared for this purpose by consulting the data from the clinical processes, observation and interview with the user and his/her caregiver.
In order to assess the intrinsic factors for falls, the following instruments were used: the Barthel Index (BI)12, which allowed us to assess the degree of dependence on ADL; the Berg Balance Scale (BBS)13 to assess the dynamic and static functional balance and to predict the risk of falling; and an observation grid drawn from the literature review that allowed for the assessment of existing changes in hearing, vision and elimination, and collection of data on regular medication and diagnosed pathologies that influenced the risk of falling.
The extrinsic risk factors for falls were identified by the Environmental Fall Risk Scale 14. This scale allowed an assessment of home safety based on the following parameters: indoor and outdoor lighting and the presence of obstacles in the bedroom, bathroom, kitchen and stairs.
Based on the diagnostic evaluation, therapeutic intervention was planned15. The rehabilitation nursing intervention program was implemented for 8 weeks in the patients' homes in sessions of 30minutes-1hour twice a week, all of whom entered the program at the same time. The plan consisted of interventions aimed at increasing muscle strengthening and balance and optimizing the physical space of the patients' homes, as explained below.
The evaluation of results was carried out using the instruments used for diagnosis.
The intervention project was approved by the sub-region Ethics Committee where the CCU is located16. The users were asked to consent for participation, in accordance with the principles of the Declaration of Helsinki and the DGS rule (15;16).
Three case studies were carried out below designated as A1, A2 and A3. The data were analyzed using descriptive techniques.
RESULTS
The participants are female aged 79, 86 and 90 years-old. Two of the women are married, live with their husband and receive support from informal caregivers. The case A3, widow, lives alone, receives support from her daughter and also from an informal caregiver. Low education is common to all participants. The two least elderly participants are those who have a history of falls and in both the accident occurred at home (Table 1).
Table 1 Sociodemographic Description of Participants
| A1 | A2 | A3 | |
|---|---|---|---|
| Age | 79 | 86 | 90 |
| Gender | Female | Female | Female |
| Nationality | Portuguese | Portuguese | Portuguese |
| Marital status | Married | Married | Widow |
| Family members | Lives with husband and has the support of an informal caregiver | Lives with husband and has the support of an informal caregiver | Lives alone with the support of her daughter and informal caregiver |
| Education level | 4th grade | 4th grade | No formal education |
| Profission | Retired | Retired | Retired |
| Fall history | 1 When transferring from bed to chair because it was not locked | 1 in the bathroom caused by imbalance | No fall history |
Study of A1Case
On October 20, 2017, the patient was admitted to the Emergency Department due to loss of strength in the right hemibody and aphasia when waking up. CT-brain (Brain Computed Axial Tomography) was performed, which revealed ischemic stroke of the left Middle Cerebral Artery. During hospitalization, she remained awake, apparently oriented, with right hemiplegia and aphasia monitored by Physical Medicine and Rehabilitation. On November 8th, she was discharged home where she waited until January 22nd, when she had a vacancy and joined the Medium Duration Continuing Care and Rehabilitation Unit, where she joined. Upon discharge home, the patient was dysarthric, without dysphagia and dependent on ADLs.
At home, the user is motivated for her rehabilitation process. She had right hemiparesis, with a severe decrease in strength in the right upper limb (1/5 Oxford Scale) and a slight decrease in the right lower limb (4/5 Oxford Scale). As intrinsic risk factors for falls, she had decreased hearing. She was undergoing sleep-inducing therapy and had a fall in the room because the wheelchair was not locked at the time of transfer.
Study of A2 Case
On December 6, 2017, the patient was admitted to the Emergency Department due to loss of strength in the right hemibody, dysarthria and deviation of the labial commissure. CT-brain was performed, which revealed left frontotemporoinsular ischemic stroke. During hospitalization, the patient remained alert, oriented, dysarthric and with right upper limb plegia and grade 1/5 (Oxford scale) right lower limb paresis. Patient was monitored by Physical Medicine and Rehabilitation. On January 16, 2018, she was discharged to a Medium Term Continuing Care and Rehabilitation Unit. At discharge, the patient was dysarthric, without dysphagia, dependent on ADLs, with a slight decrease in functionality.
At home, the patient was motivated for rehabilitation process. She had right hemiparesis, with a severe decrease in strength in the right upper limb (2/5 Oxford Scale) and a moderate decrease in the right lower limb (3/5 Oxford Scale).
As intrinsic risk factors for falls, the patient had decreased hearing. She was undergoing sleep-inducing, diuretic and anti-hypertensive therapy and had a fall in the bathroom due to imbalance at the time of transfer, when trying to do it without help.
Study of A3 Case
On July 18, 2018, the patient was admitted to the Emergency Department with loss of strength in the left hemibody and aphasia. CT-brain revealed thalamic hemorrhagic stroke in the right hemisphere. During hospitalization she remained awake, oriented, dysarthric and with grade 3/5 left upper and lower limb paresis (Oxford Scale). On admission, she was followed up in the Physical Medicine and Rehabilitation specialty. On July 26, 2018, she was discharged home.
At home, the patient was motivated for rehabilitation process. She had left upper limb paresis, with a slight decrease in strength in the left upper limb (4/5 Oxford Scale) and normal strength in the left lower limb (5/5 Oxford Scale).
As intrinsic risk factors for falls, she had uncompensated hearing and vision impairment and was taking antihypertensive therapy.
Rehabilitation Nursing Intervention
The analysis of the initial assessment data led to the formulation of the RN diagnoses present in each user (Table 2):
Table 2 Rehabilitation Nursing Diagnoses
| Users | Identified diagnoses |
|---|---|
| A1 | Highly dependent on walking; Moderately dependent on Transferring; Compromised Body Balance; Decreased Muscle Movement; Present Falls Risk, in Moderate Degree |
| A2 | Highly dependent on walking; Moderately dependent on Transferring; Compromised Body Balance; Decreased Muscle Movement; Present Falls Risk, in High Degree |
| A3 | Highly dependent on walking; Highly dependent on Transferring; Compromised Body Balance; Decreased Muscle Movement; Present Falls Risk, in High Degree |
(Source: adapted from the Order of Nurses (17))
Regarding walking, all users had difficulty. In all cases, the use of a walking aid was encouraged and trained, namely the walking stick in cases A1 and A2 and walking frame in case A3. In addition to this, maneuvers such as turning, sitting and standing and overcoming obstacles present in their homes were also trained.
For the transfers, several techniques were trained, such as rolling and sitting in bed, static and dynamic seated balance, moving to an upright position, turning 180º and sitting with controlled descent in a wheelchair.
The participants had compromised body balance, and techniques were trained to recover static and dynamic balance, both in the sitting and upright positions. The training started in a sitting position with feet supported and trunk free for 1 min, followed by 10 repetitions with elevation of the upper limbs to the right and to the left, forward and upwards and 10 repetitions of trunk balance back and forth. Subsequently, static balance was trained in the upright position: without support for 20 seconds with eyes open, and then with eyes closed; with feet together for 30 seconds and with one foot in front of the other for another 30 seconds. In dynamic balance in the upright position, the following techniques were trained: from a sitting position to a standing position and vice versa; sit with your back unsupported, with your feet flat on the floor and lean forward with your upper limb extended. In all trained techniques, postural correction was always encouraged and the exercise time was gradually increased.
Regarding muscle movement, it was reduced in all cases due to pathologies and associated limitations. Muscle and joint exercise techniques were trained, namely: assisted and resisted active mobilizations, sitting and standing up without leaning more than 6 times; flexion of the thigh-femoral joint 6 to 8 times; with feet supported, swing for more than 30 seconds; bending the trunk with hands on the waist to the right and left more than 20 times and therapeutic exercises in bed such as the bridge, rolling to the healthy side and to the affected side and controlled rotation of the hip. In all trained techniques, the exercise time was increased according to the users' capacity 18.
All techniques were trained in the presence of caregivers, so that they could perform and train with users safely and effectively.
The evaluations of the users' homes were included and the respective teachings were carried out to family members and caregivers so that they could understand the importance of organizing the space and maintaining free access to increase safety and reduce the risk of falls at home.
In A1 user’s home, the main external factor for falls identified was the building’s stairs, as it did not have a bilateral handrail or non-slip coating. The husband carried out adaptation works in the bathroom and optimized the rest of the physical space in the house.
Regarding the extrinsic factors present in the A2 user's home, the main problem was in the walking areas as it were not free from obstructions. The caregiver was encouraged to clear them, facilitating circulation in the house areas. Although the bathroom has undergone works, these were not carried out properly, since the handrail was placed on the opposite side and the shower cabin was raised relative to the ground, which prevented the user from transferring easily.
In the A3 user's home, the main problem was the bathroom, as it did not have support bars that facilitated its transfer and because it had a bathtub that prevented the user from being transferred easily. The family optimized the remaining physical space in the house, leaving the circulation areas unobstructed.
DISCUSSION
Following the case study methodology of Yin, Robert11, the phase of gathering the results obtained through the evaluation of users follows.
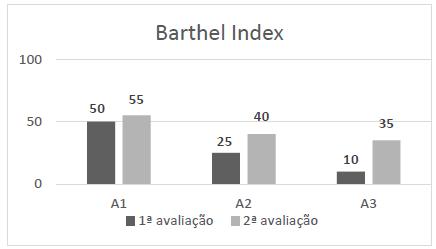
When evaluating the results obtained, it is possible that in all cases there were gains in the participants' ability to perform the ADL's (BI) in 45 points. The evolution between the first and second assessments is illustrated in Graphic 1.
User A1 continued to have a serious dependence on self-care, despite having obtained gains in transfers. User A2 also maintained the level of dependency as serious, despite having obtained gains essentially in transfers and mobility. In the case of user A3, it is possible to notice a positive evolution from total dependence to severe dependence, with the greatest evolution in mobility. Regarding walking self-care, all users were able to walk around the house with a walking aid, with supervision and occasional help. In case A2, the results were less evident due to the presence of joint knee instability of the affected hemibody, which made walking difficult. The results obtained in self-care transfer were independence in sitting with controlled descent and moving to a standing position in cases A1 and A2. Case A3 maintained the need for support to assume the standing position.
The results obtained in independence (BI) are corroborated by Hager et al19, who also concluded in their study that physical exercise programs at home to prevent falls are effective in reducing risk factors. Furthermore, they improve the balance, strength and functional capacity of the elderly.
Martinez-Velilla et al20 also demonstrated through their study with 370 elderly people that the implementation of a physical activity program prevents the functional decline of users, with an improvement of about 6.9 points in the BI in the intervention group (exercise program twice a day) when compared to the control group.
In another study carried out by Kato et al21, a physical exercise program was applied for 12 weeks, whose interventions were: sitting down and getting up from a chair and walking in the same place. At the end of the intervention, it was possible to obtain a gain of about 11.6% in the BI, when compared to the intervention group to the control group.
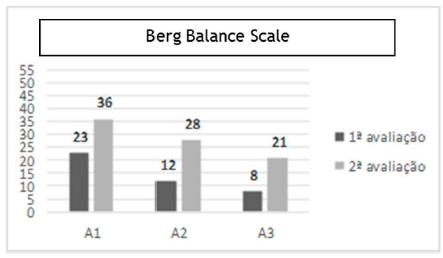
After the application of the program, there was a decrease in intrinsic risk factors for falls, related to balance, as shown in Graphic 2.
As for the results obtained from the BBS, the diagnostic evaluation classified two participants as being at high risk and one at medium risk of falling. Two participants went from high to medium risk, and only in one of the cases there was no reduction in risk. In users A1 and A2, the biggest gains were essentially at the level of moving from a sitting position to a standing position, going from minimal help to being able to stand independently with the help of the hands. Regarding the change from standing to sitting, users were able to sit with the use of their hands to control the descent, and at the end of the assessment they were able to do it with minimal use of their hands. Regarding the A3 user, the main gains obtained were in static balance, both in the sitting and standing position. Sitting without trunk support, the user increased the execution time from 10 seconds to 2 minutes with supervision. In the unsupported standing position with eyes closed, the user needed help to avoid falling and was able to do it autonomously for 3 seconds.
Also in the study by Hess and Woollacott, M (22 applied to the elderly people for 10 weeks through high-intensity exercise, it was possible to observe an evolution in the BBS score from 48.8 at the beginning of the program to 51.2 points in the end of period.
The results obtained through the evaluation by the BI and the BBS demonstrate the need for users with neurological disorders to have interventions aimed at promoting autonomy in self-care, in order to reduce the risk of falling associated during its execution, namely in walking and transferring. From these results emerges the reflection that the best response was found in the A3 user who had a stroke not so long ago.
CONCLUSION
The specific competences of the Rehabilitation nurses are to take care of people with special needs throughout the life cycle, in all contexts of care practice, to train the person with a disability, activity limitation and/or participation restriction for the reintegration and exercise of citizenship and maximize functionality by developing the person's capabilities.
Based on the identified needs, specialized and individualized intervention plans were designed in order to maximize their capabilities and reduce their limitations, thus allowing for better motor performance. The intervention plans included muscle strengthening and balance training programs in order to promote adaptation to the limitations resulting from the pathology, reduce the risk of falling and maximize autonomy, thus predicting repercussions on their social reintegration and quality of life at home. These training programs were designed according to the users' objectives and taking into account the pathology and individual needs of each one, in order to promote their rehabilitation.
The implementation of the intervention program by the RN indicates that it has benefits in obtaining gains in balance and in the ability to carry out self-care, which consequently reduces the risk of falls in the elderly at home.
As limitations of the work, the reduced number of study participants can be pointed out, with a larger number having a greater representation of the population. In the future, more research studies in this area are suggested that can corroborate the data presented and that can value the work and the impact that RNs interventions have on the users' quality of life.
REFERÊNCIAS BIBLIOGRÁFICAS
1 Ordem dos Enfermeiros. Regulamento das Competências Especificas do Enfermeiro Especialista em Enfermagem de Reabilitação. [Online] 2010. https://www.ordemenfermeiros.pt/arquivo -de-p%C3%A1ginas-antigas/regulamento-das-compet%C3%AAncias-comuns-do-enfermeiroespecialista-e-regulamentos-das-compet%C3%AAncias-espec%C3%ADficas-das-especialidades-em-enfermagem/. [ Links ]
2 Marques-Vieira, C, Amaral, T e Pontifice-Sousa, P. Contributos para um Envelhecimento Ativo. [autor do livro] C Marques-Vieira e L Sousa. Cuidados de Enfermagem de Reabilitação à Pessoa ao longo da Vida. Loures : Lusodidacta, 2017: 525-34. [ Links ]
3 Instituto Nacional de Estatistica. Indicadores de envelhecimento. [Online] 2018. https://www.pordata.pt/Portugal/Indicadores+de+envelhecimento -526. [ Links ]
4 Esquenazi, D; Silva, S e Guimarães, M. Aspectos fisiopatológicos do envelhecimento humano e quedas em idosos. Revista HUPE. 2014; 13 (2): 11-20. [ Links ]
5 Lopes, M. A avaliação da funcionalidade dos idosos: uma forma de diagnosticar o estado de saúde e avaliar a eficácia dos cuidados. Conferência Internacional sobre Enfermagem Geriátrica. Livro de Atas. Lisboa. 2012 [ Links ]
6 Petridoou, ET; Dikalioti , SK; Dessypris, N; Skalkidis, I; Basbone, F; Fitzpatrick, P et al. The evolution of unintencional injury mortality among elderly in Europe. s.l. : J Aging Health. 2008; 20: 159-82. [ Links ]
7 Verbrugge, IM e Jette, AM. The disablement process. s.l. : Soc. Sci. Med. 1994; 38 (1): 1-14. [ Links ]
8 Direção-Geral da Saúde e Fundação MAPFRE. Prograna Nacional de Prevenção de Acidentes. Projeto: Com Mais Cuidado - Prevenção de acidentes domésticos com pessoas idosas. Manual de Apoio e Formulário. Lisboa : s.n., 2012. [ Links ]
9 Freiberger, E; Menz, H; Abu-Omar, K; Rütten, A. Preventing Falls in Physically Active. Gerontology. 2007; 53: 298-305. [ Links ]
10 Daly, R; Duckham, R; Tait, J; Rantalainen, T; Nowson, C; Taaffe, D et al. Effectiveness of dual-task functional power training for preventing falls in older people: study protocol for a cluster randomised controlled trial. Daly et al. Trials. 2015; 16:120. [ Links ]
11 Yin, Robert K. Estudo de Caso: Planejamento e Métodos. 4ªed. Porto Alegre : Bookman. 2010. [ Links ]
12 Araujo, F; Ribeiro , J; Oliveira, A; Pinto, C. Validação do Índice de Barthel numa amostra de Idosos não Institucionalizados. Qualidade de Vida. 2007; 25 (2): 59-66. [ Links ]
13 Ordem dos Enfermeiros. Instrumentos de colheita de dados para a documentação dos Cuidados Especializados em Enfermagem de Reabilitação. [Online] 2016. https://www.ordemenfermeiros.pt/arquivo/colegios/Documents/2017/InstRecolhaDadosDocumentacaoCuidEnfReabilitacao_Final_2017.pdf. [ Links ]
14 Victorian Quality Council. Minimising the Risk of Fall & Fall - related injuries. Sub-acute and Residential Care. [Online] 2004. http://www.networkofcare.org/library/Guidelines%20for%20Fall%20Prevention%20in%20Acute,%20Sub acute%20and%20Residential%20Care%20Settings.pdf. [ Links ]
15 Lopes, M. A relação entre enfermeiro-doente como intervenção terapêutica: proposta de uma teria de médio alcance. Coimbra : Formasau. 2006. [ Links ]
16 Norma 015/2013. Consentimento Informado, Esclarecido e Livre Dado por Escrito. DGS. 2013. [ Links ]
17 Assembleia Geral da WMA. Declaração de Helsinque da Associação Médica Mundial. Princípio éticos para pesquisa médica envolvendo seres humanos. outubro de 2013. [ Links ]
18 Ordem dos Enfermeiros. Padrão Documental dos Cuidados de Enfermagem da Especialidade de Enfermagem de Reabilitação. [Online] 2015. https://www.ordemenfermeiros.pt/arquivo/colegios/Documents/2015/MCEER_Assembleia/PadraoDocumental_EER.pdf. [ Links ]
19 Hager, A; Mathieu, N; Lenoble-Hoskovec, C; Swanenburg, J; Bie, R; Hilfiker, R. Effects of three home-based exercise programmes regardings falls, quality of life and exercise adherence in older adults at risk of falling: protocol for a randomized controlled trial. BMC Geriatrics. 2019; 19(13): 1-11. [ Links ]
20 Martinez-Velilla, N; Casas-Herrero, A; Zambom-Ferraresi, F; Lopez, M; Lucia, A; Galbete, A, et al. Effect of Exercise Intervention on Functional Decline in Very Elderly Patients During Acute Hospitalization: A Randomized Clinical Trial. JAMA Intern Med. 2018. [ Links ]
21 Kato, Y; Islam, M; Koizumi, D; Rogers, M; Takeshima, N. Effects of a 12-week marching in place and chair rise daily exercise intervention on ADL and functional mobility in frail older adults. J. Phys. Ther. Sci. 2018; 30(4): 549-554. [ Links ]
22 Hess, J e Woollacott, M. Effect og high-intensity strenght-training on functional measures of ballance ability in balance-impaired older adults. J Manipulative Psysiol Ther. 2005; 28(8): 582-90. [ Links ]
Received: April 24, 2019; Accepted: June 27, 2019











 texto em
texto em