Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista Portuguesa de Enfermagem de Reabilitação
versão impressa ISSN 2184-965Xversão On-line ISSN 2184-3023
RPER vol.2 no.1 Silvalde jun. 2019
https://doi.org/10.33194/rper.2019.v2.n1.08.4567
Articles
Exercise training in people with a stabilized chronic respiratory disease: a Scoping Review
1- Centro Hospitalar e Universitário São João
3- Escola Superior de Enfermagem do Porto
Introduction:
Pulmonary Rehabilitation is (PR) integrates the non-pharmacological component of the clinical guidelines for the control and treatment of chronic respiratory diseases.
The Rehabilitation Nurse (RN), integrated into a multidisciplinary team, designs, implements and monitors PR programs that include exercise training.
Being the nursing disciplinary knowledge one of the pillars of clinical decision and the guarantor of the quality and safety of nursing care becomes relevant to know the impact of these programs, conducted by RN, in order to improve clinical practice.
Objective:
To know the impact of PR programs, conducted by nurses, on people with chronic respiratory disease.
Methodology:
Scoping review with Joanna Briggs Institute® methodology using two independent reviewers.
Results:
We included 10 studies that showed that nurse-led PR programs increase exercise tolerance, quality of life, functional independence, and reduce dyspnea and anxiety.
Conclusion:
The PR performed by RN in patients with chronic respiratory disease is overlapping with the latest evidence.
Key words: Exercise training; Rehabilitation Nursing; Respiratory Rehabilitation; Chronic Respiratory Disease
Introdução:
A Reabilitação Respiratória (RR) integra a componente não farmacológica das principais guidelines clínicas para o controlo e tratamento das doenças respiratórias crónicas.
O Enfermeiro de Reabilitação (ER), integrado numa equipa multidisciplinar, concebe, implementa e monitoriza programas de RR onde se inclui o treino do exercício.
Sendo o conhecimento disciplinar de enfermagem um dos pilares da decisão clínica e a garantia da qualidade e segurança dos cuidados de enfermagem torna-se relevante conhecer o impacte destes programas, conduzidos por ER, de forma a melhorar a prática clinica.
Objetivo:
Conhecer o impacte dos programas de RR, conduzidos por enfermeiros, nas pessoas com doença respiratória crónica.
Metodologia:
Scoping review com metodologia do Joanna Briggs Institute® com recurso a dois revisores independentes.
Resultados:
incluímos 10 estudos que revelaram que programas de RR conduzidos por enfermeiros de reabilitação aumentam a tolerância ao exercício, a qualidade de vida, a independência funcional e reduzem a dispneia e a ansiedade.
Conclusão:
A RR realizada por ER em pessoas com doença respiratória crónica é sobreponível à mais recente evidência.
Palavras-chave: Treino de exercício; Enfermagem de Reabilitação; Reabilitação Respiratória; Doença respiratória crónica
Introducción:
La Rehabilitación Pulmonar (RP) es el tratamiento no farmacológico que consta en los principales guías clínicos para el control y la realización de las tareas respiratorias crónicas.
El Enfermero de Rehabilitación (ER), constituido en una disciplina multidisciplinaria, concibe, implementa y monitorea programas de RP en que se incluye el entrenamiento del ejercicio.
Siendo el conocimiento disciplinario de enfermería uno de los pilares de la decisión clínica y el garante de la calidad y seguridad de los cuidados de enfermería, resulta relevante conocer el impacto de estos programas, conducidos por ER, para mejorar la práctica clínica.
Objetivo:
conocer el impacto de los programas de RR, conducidos por enfermeros, en las personas con la enfermedad respiratoria crónica.
Metodología:
Revisión de alcance con metodología del Instituto Joanna Briggs® con dos revisores independientes.
Resultados:
incluimos 10 estudios que revelaron que los RR conducidos por enfermeros aumentaron la tolerancia al ejercicio, una calidad de vida, una autonomía funcional y una disnea y la ansiedad.
Conclusión:
La RR realizada por ER en personas con enfermedad respiratoria es crónica es sobreponible a la más reciente evidencia.
Palabras clave: Ejercicio; Enfermería de Rehabilitación; Rehabilitación Respiratoria; Enfermedad respiratoria crónica
INTRODUCTION
Dyspnea, activity intolerance and reduced quality of life are frequent manifestations in people with chronic respiratory disease (CRD)1-4. These manifestations are not only the result of loss of lung function, but result from peripheral muscle dysfunction. If that were the case, medication alone would be effective in increasing tolerance to the activity, which is not the case 1-2,5-6. Peripheral muscle dysfunction is characterized by the loss of strength and muscle mass, which leads to changes in the distribution of muscle fibers, which, together with alterations in gas exchanges, result in reduced exercise capacity in people with CRD.
This activity intolerance limits functional independence with a consequent negative impact on the capacity for self-care9, and on the increase in mortality1,10.
Clinically, it is translated by the person's inability to carry out their daily activities, in the intensity or duration normally tolerable for healthy and sedentary people1. This adoption of a sedentary lifestyle (in order to avoid functional dyspnea) leads to muscle deconditioning, enhancing the loss of function1,7,10-11.
Muscle performance (strength and endurance) results from the physiological structure of the muscles, and the peripheral muscle dysfunction manifested by people with CRD results from an alteration in the distribution of muscle fibers, their size, capillary density and metabolic capacity(2,4-5.11).
In this context, the unavoidable importance of exercise training emerges, which in a respiratory rehabilitation program (RRP) contributes to the increase in exercise tolerance, decreasing oxygen consumption in the face of the same amount of exercise and reducing the manifestations of dyspnea1,5,8.
Exercise training in this context includes aerobic training, or endurance training and anaerobic or muscle strength training.
Aerobic training, or endurance training, uses large muscle groups with moderate to long duration and moderate to high intensity2,4,9,12. It requires repeated physical activity over a specific period of time and aims to increase and modulate endurance capacity and increase the number of type I fibers.
On the other hand, muscle strength training (anaerobic training component) designed to increase muscle strength and mass, essential for carrying out activities of daily living, uses small muscle groups at high intensity and for a short duration, thus reducing cardiorespiratory limitations characteristics of people with chronic respiratory disease in more advanced stages of the disease.
The best physiological response is obtained by joining the two training modalities, tending to be performed at high intensity.
This is why Respiratory Rehabilitation, which obligatorily includes exercise training, is the recommended non-pharmacological treatment for people with chronic respiratory disease in an outpatient setting.
In this sense, the role of the RN should not be solely related to respiratory kinesitherapy or the educational component, but should accompany the scientific evidence and also undergo exercise training, as is furthermore enshrined in the Regulation of Specific Competencies of the Specialist Nurse Rehabilitation Nursing, which describes the competence of the Rehabilitation Nurse - to design, implement, evaluate and reformulate motor and cardio-respiratory training programs.
Given the above, it is essential to know the exercise training programs included in the respiratory rehabilitation programs (RRP) carried out by rehabilitation nurses.
A previous search carried out in MEDLINE and CINAHL did not reveal any literature review on this topic, so it was decided to carry out a Scoping Review in order to map the use of exercise training in respiratory rehabilitation programs carried out by nurses for people with disease chronic respiratory in an outpatient setting.
The option for a scoping review was linked not only to the objective of mapping scientific evidence to support the clinical decision of rehabilitation nurses, but also to identify possible areas of interest for disciplinary investigation.
METHOD
The methodology used to carry out this scoping review followed the steps proposed by the Joanna Briggs Institute®, and intended to answer the following question: "What is the impact of exercise training programs, conducted by rehabilitation nurses, on people with chronic respiratory disease?"
Inclusion Criteria
Type of participants
People with chronic respiratory disease, without age limit and regardless of disease severity.
Concept
Regarding concepts, articles focused on respiratory rehabilitation programs defined as “comprehensive intervention, based on an extensive assessment of patients, followed by individualized treatments that include - but not limited to - physical exercise. Education and behavioral change, designed to improve the physical and emotional condition of people with chronic respiratory disease and to promote long-term adherence to health behaviors.” 1-3
The definition of exercise training includes a combination of aerobic and anaerobic training (with muscle strengthening of the upper and lower limbs) with a minimum duration of 8 weeks.1-3
Exclusion Criteria
Studies applied to areas of health other than nursing and those in which the methodology presents omissions in the research design were excluded from the review.
Research strategy
The survey, carried out in June 2018, was designed considering three main steps:
In the first stage, first and second level controlled terms were considered to define the research term, namely by collecting the main and additional descriptors and qualifiers present in the Medical Subject Headings (MeSH) and in the Headings of the Cumulative Index of Nursing and Allied Health Literature (CINAHL). In the second stage, keywords and terms used by the authors to define the categories under analysis were added, constructing the following search term:
("Exercise training" OR "Pulmonary rehab*") AND ("Lung Disease*" OR "Pulmonary disease*" OR “COPD” OR “Bronchiectasis” OR "Cystic fibrosis" OR “Asthma” OR "Interstitial lung disease*") AND ("nurse led intervent" *" OR "nurse-led clinic*" OR "Nurses practice pattern*") AND ("self-care" OR "functional independence" OR "exercise tolerance" OR "activity of daily living" OR "quality of life" OR " motor activity") NOT ("physical therapy*")
Therefore, reference databases were tracked, namely Scopus and Web of Science, and the EBSCO content aggregator, allowing coverage of the following databases and indexes MEDLINE, Science Citation Index, Social Sciences Citation Index, Emerging Sources Citation Index , Book Citation Index, Conference Proceedings Citation Index, Korean Citation Index, Russian Science Citation Index, SciELO Citation Index, Directory of Open Access Journals, Directory of Open Access Scholarly Resources, Academic Search Complete, Business Source Complete, CINAHL Complete, ERIC, MedicLatina, Psychology and Behavioral Sciences Collection and SPORTDiscus database. It also accesses the research in gray literature in the Scientific Repository of Open Access of Portugal.
In the third stage, the reference lists of the included studies were analyzed in order to build the citation map and potential references for inclusion.
The selection of studies was made according to the inclusion and exclusion criteria previously defined by two independent reviewers, based on the information mentioned in the title and abstract. The disagreement between the two reviewers implied the intervention of a third reviewer.
For the step of separating, summarizing and reporting the essential elements found in each study, a structured instrument was built that allowed for the synthesis, interpretation and analysis of data, the nature and distribution of the studies incorporated in the review. Items such as year of publication, methodology used, duration of exercise training programs, interventions and results obtained were grouped.
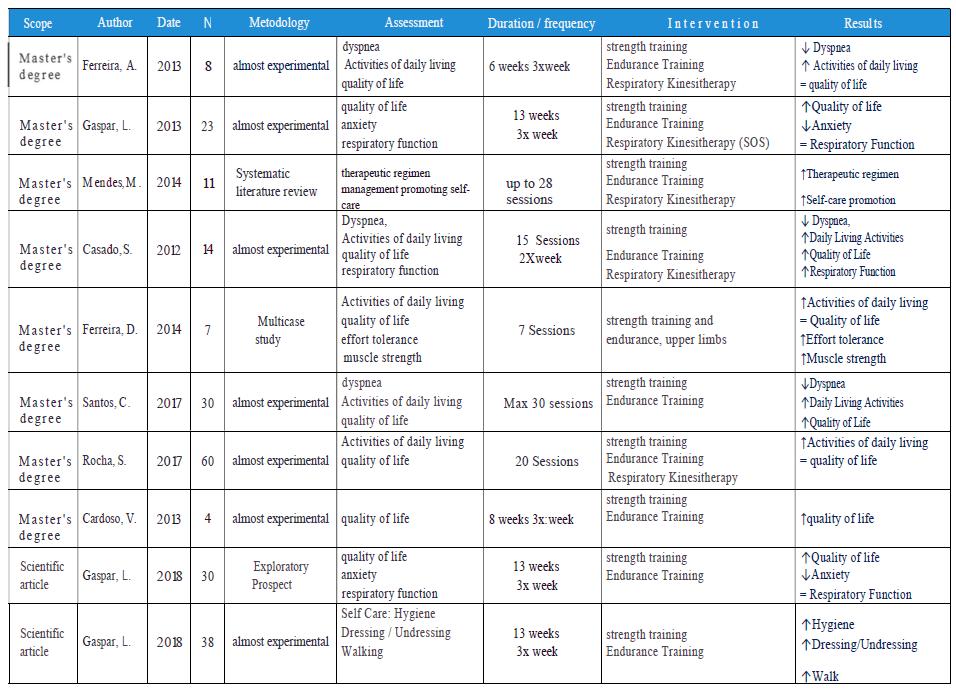
In the final phase, a framework was built in order to obtain an overview of the studies included in the review. (figure 2)
EXTRACTION OF RESULTS
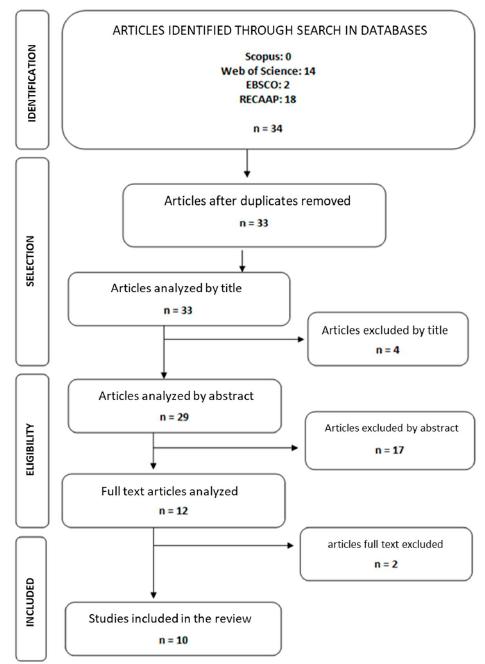
Based on the applied search strategy, 34 potentially relevant articles were identified.
One was excluded because it was duplicated, four were excluded after title analysis and seventeen were excluded after abstract analysis.
The analysis of the full text of the remaining twelve articles led to the exclusion of two. Finally, ten articles were included in the review (figure 1).
All of the studies are Portuguese, eight resulting from master's dissertations and two from scientific articles published in a journal.
From a methodological point of view, all studies are quantitative, seven being quasi-experimental, two exploratory descriptive and one systematic literature review.
There was little scientific production on this topic considering the different contexts.
Six studies have respiratory kinesitherapy intervention that is not recommended in this context.
From the analysis of the articles, the following categories of information emerged: duration/frequency of the exercise training program, type of exercise training and results obtained.
Duration of exercise training programs
The duration of exercise and training programs found in the articles under review was quite diverse, ranging between 7 and 39 weeks, and in most articles found the duration of the programs is between 25 and 39 weeks.
Exercise training typology
The exercise training typology category comprises the type and characteristics of the training.
In all the selected articles, the exercise training programs included aerobic training of 30 minutes and anaerobic training, the latter being on upper and lower limbs.
Five articles include respiratory kinesitherapy as an intervention that is not recommended in this context.
Results obtained
Regarding the results obtained, three articles refer to a decrease in dyspnea, five to an increase in quality of life and tolerance in activities of daily living, two articles reveal the promotion of self-care, decrease in anxiety and increase in tolerance to exertion, and one article refers to improvement in the management of therapeutic regimen.
DISCUSSION
The results of this review allow us to identify that the exercise training programs designed, implemented and carried out by rehabilitation nurses contribute to the reduction of dyspnea, anxiety, increasing tolerance to effort and life activities, thus contributing to the improvement quality of life.
These results overlap with the scientific evidence clearly identified in the latest European Respiratory Society Guidelines published in 20133 and confirmed in 2017 by Shioya et al13.
Recently, studies such as those by Robinson et al.8 and McNamara et al.12, both in 2018, confirmed the role of exercise training in improving dyspnea.
Gordon et al., 201914 published a meta-analysis showing the impact of exercise training on depression and anxiety. Regarding the increase in exercise tolerance and its consequences on the ability to perform activities of daily living, the evidence is vast, as shown by the studies by Bisca et al., 201415, Spruit et al, 20155 and more recently in 2019 the study by Vaes15 showing the positive impact on these variables.
The multisystemic character of chronic respiratory diseases (especially COPD) leads to a progressive functional decline, resulting from sarcopenia secondary to immobility, with important consequences, namely in terms of autonomy in carrying out activities of daily living and self-care9-10,13.
In this context, Respiratory Rehabilitation emerges as the non-pharmacological treatment indicated for people with chronic respiratory disease, fundamentally focused on an approach in which exercise training is, along with education, the main component1,4,6.
Respiratory rehabilitation programs increase activity tolerance and reduce dyspnea, aspects that translate into functional gains and the capacity for self-care2,9,15.
In addition to these effects, respiratory rehabilitation also reduces hospitalizations and mortality16.
There is no consensus about its duration and the most recent recommendation defines it as a minimum duration of 8 weeks with 3 sessions per week1,3,16. As most symptoms result from peripheral muscle dysfunction (which leads to increased oxygen consumption) it is clear that the objective of respiratory rehabilitation programs is to improve activity tolerance and later exercise tolerance through improving strength and peripheral muscle resistance, thus contributing to improve quality of life1,3,5.
There is, in fact, a direct relationship between walking time and functional status11, as well as between upper limb performance and performance in activities of daily living 17.
All indicators show that the usual tendency of immobility in these people is not only respiratory, but also muscular, since the muscle morphological changes found in these people are important, namely the reduction of type I fibers, the loss of strength and capacity of resistance, especially of the lower limbs1-2,4,7.
When compared to healthy people, tolerance to exertion is lower, resulting in increased shortness of breath secondary to dynamic hyperinflation and immobility2,4,12.
This is the reason why it is concluded that the combination of aerobic and anaerobic training is more effective1,3,5.
The evidence related to the results of exercise training programs is quite vast. Studies show that there are health gains in practically all the indicators studied, namely dyspnea and activity intolerance, with an important impact on the promotion of self-care and quality of life.
CONCLUSION
This study allowed us to identify two central aspects: the first is that exercise training programs conducted by nurses adhere to international guidelines; the second is that the results obtained (improved perception of dyspnea; decreased anxiety; increased tolerance to exertion and activities of daily living, as well as improved quality of life) are comparable to the best available scientific evidence.
This study demonstrates the positive impact of the action of rehabilitation nurses on the health condition of people with chronic respiratory disease who participate in exercise training programs.
Given the widely described importance of the benefits of exercise training in this context, more studies should be carried out and published on this topic.
REFERÊNCIAS BIBLIOGRÁFICAS
1 Ferreira D, Teodoro A, Gaspar Lea. Guia Orientador de Boa Prática - Reabilitação Respiratória Lisboa: Ordem dos Enfermeiros; 2018. [ Links ]
2 Gaspar L. Treino aeróbico e de fortalecimento muscular no doente com patologia respiratória. Enfermeiro: Anuário 2017. 2017 Maio;.(Reabilitação Respiratória). [ Links ]
3 Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, Hill K, Holland AE, Lareau SC, Man WD, Pitta F. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013 Oct 15;188(8):e13-64. [ Links ]
4 Andrianopoulos V, Klijn P, Franssen FM, Spruit MA. Exercise training in pulmonary rehabilitationClin Chest Med. 2014 Jun 1;35(2):313-22.. [ Links ]
5 Spruit MA, Pitta F, McAuley E, ZuWallack RL, Nici L. Pulmonary rehabilitation and physical activity in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2015 Oct 15;192(8):924-33.. [ Links ]
6 Pitta F, Troosters T, Spruit MA, Probst VS, Decramer M, Gosselink R. Characteristics of physical activities in daily life in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005 May 1;171(9):972-7. [ Links ]
7 Braido F, Baiardini I, Menoni S, Bagnasco AM, Balbi F, Bocchibianchi S, Balestracci S, Piroddi MG, Canonica GW. Disability in COPD and its relationship to clinical and patient-reported outcomes. Curr Med Res Opin. 2011 May 1;27(5):981-6. [ Links ]
8 Robinson H, Williams V, Curtis F, Bridle C, Jones AW. Facilitators and barriers to physical activity following pulmonary rehabilitation in COPD: a systematic review of qualitative studies. NPJ Prim Care Respir Med. 2018 Jun 4;28(1):19. [ Links ]
9 Gaspar L, Martins P. Impacto de um programa de reabilitação respiratória nos autocuidados higiene, vestir-se/despir-se e andar avaliados pela escala London Chest Of Daily Living em pessoas com doença respiratória crónica. Rev Port Enferm Reabil. 2018; 1(1):13-17. [ Links ]
10 Lahaije AJ, Van Helvoort HA, Dekhuijzen PN, Heijdra YF. Physiologic limitations during daily life activities in COPD patients. Respir Med. 2010 Aug 1;104(8):1152-9. [ Links ]
11 Miravitlles M, Cantoni J, Naberan K. Factors associated with a low level of physical activity in patients with chronic obstructive pulmonary disease. Lung. 2014 Apr 1;192(2):259-65.. [ Links ]
12 McNamara RJ, Spencer L, Dale M, Leung RW, McKeough ZJ. Alternative Exercise and Breathing Interventions in Chronic Obstructive Pulmonary Disease: A Critical Review. EMJ Respir. 2018;6(1):117-27. [ Links ]
13 Bisca GW, Proença M, Salomão A, Hernandes NA, Pitta F. Minimal detectable change of the London chest activity of daily living scale in patients with COPD. J Cardiopulm Rehabil Prev. 2014 May 1;34(3):213-6.. [ Links ]
14 Spruit MA, Pitta F, McAuley E, ZuWallack RL, Nici L. Pulmonary rehabilitation and physical activity in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2015 Oct 15;192(8):924-33.. [ Links ]
15 Martins T, Araujo MF, Peixoto MJ, Machado PP. A pessoa dependente & o familiar cuidados Porto: Enfermagem.Porto; 2016. [ Links ]
16 McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane database of systematic reviews. 2015(2). Disponível em: https://doi.org/10.1002/14651858.CD003793.pub3 [ Links ]
17 Velloso M, Stella SG, Cendon S, Silva AC, Jardim JR. Metabolic and ventilatory parameters of four activities of daily living accomplished with arms in COPD patients. Chest. 2003 Apr 1;123(4):1047-53. [ Links ]
18 ICN. Classificação Internacinal para a Prática de Enfermagem (CIPE) versão 1.0 Genebra; 2005. [ Links ]
19 Pitta F, Probst VS, Kovelis D, Segretti NO, Leoni AM, Garrod R, Brunetto AF. Validação da versão em português da escala London Chest Activity of Daily Living (LCADL) em doentes com doença pulmonar obstrutiva crónica. Rev Port Pneumol. 2008 Feb;14(1):27-47. . [ Links ]
20 Goto Y. Measurement of Activities of daily living in patients with chronic obstructive pulmonary disease. Pulm Res Respir Med Open J. 2017; SE(2): S23-S25. doi: 10.17140/PRRMOJ-SE-2-104 [ Links ]
21 Garrod R, Paul EA, Wedzicha JA. An evaluation of the reliability and sensitivity of the London Chest Activity of Daily Living Scale (LCADL). Respir Med. 2002 Sep 1;96(9):725-30.. [ Links ]
22 Jehn M, Schmidt-Trucksäss A, Meyer A, Schindler C, Tamm M, Stolz D. Association of daily physical activity volume and intensity with COPD severity. Respir Med. 2011 Dec 1;105(12):1846-52. [ Links ]
23 Carpes MF, Mayer AF, Simon KM, Jardim JR, Garrod R. Versão brasileira da escala London Chest Activity of Daily Living para uso em pacientes com doença pulmonar obstrutiva crônica. J Bras Pneumol. 2008 Mar;34(3):143-51. [ Links ]
24 Muller JP, Gonçalves PA, da Fontoura FF, Mattiello R, Florian J. Aplicabilidade da escala London Chest Activity of Daily Living em pacientes em lista de espera para transplante de pulmão. J Bras Pneumol. 2013;39(1):92-7.. [ Links ]
25 ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111-7. [ Links ]
26 Agusti A, Decramer M, Celli BR. Pocket guide to COPD diagnosis, management and prevention. Global Initiative for Chronic Obstructive Lung Disease. 2017; 14:37-44. [ Links ]
27 Sciriha A, Moore K, Montefort S. Combining inspiratory muscle training and upper limb exercises. Does it improve outcomes in COPD patients?. J ACPRC. 2009; 41. [ Links ]
28 Zeng Y, Jiang F, Chen Y, Chen P, Cai S. Exercise assessments and trainings of pulmonary rehabilitation in COPD: a literature review. Int J Chron Obstruct Pulmon Dis. 2018;13:2013-23. [ Links ]
29 Shioya T, Iwakura M, Kawagoshi A. Recent advances in pulmonary rehabilitation for patients with COPD. Pulm Res Respir Med Open J. 2017:S7-19. [ Links ]
30 Braido F, Baiardini I, Menoni S, Bagnasco AM, Balbi F, Bocchibianchi S, Balestracci S, Piroddi MG, Canonica GW. Disability in COPD and its relationship to clinical and patient-reported outcomes. Curr Med Res Opin. 2011 May 1;27(5):981-6. [ Links ]
31 Carpes MF, Mayer AF, Simon KM, Jardim JR, Garrod R. Versão brasileira da escala London Chest Activity of Daily Living para uso em pacientes com doença pulmonar obstrutiva crônica. J Bras Pneumol. 2008 Mar;34(3):143-51.. [ Links ]
32 Jehn M, Schmidt-Trucksäss A, Meyer A, Schindler C, Tamm M, Stolz D. Association of daily physical activity volume and intensity with COPD severity. Respir Med. 2011 Dec 1;105(12):1846-52. [ Links ]
Received: March 14, 2019; Accepted: June 22, 2019











 texto em
texto em