Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Portuguesa de Enfermagem de Reabilitação
Print version ISSN 2184-965XOn-line version ISSN 2184-3023
RPER vol.2 no.2 Silvalde Dec. 2019
https://doi.org/10.33194/rper.2019.v2.n2.02.4554
Articles
The use of a multisensorial stimulation programme in patients with severe disabilities in their cognitive ability
1- Hospital Garcia de Orta - Serviço de Neurocirurgia
A multisensorial stimulation programme (MSP) was implemented in patients with severe changes in their state of councieousness, integrated in a project of continuous improvement of the quality of nursing care: "Evaluation and stimulation of patients with changes in the state of consciousness"(1). We aimed to promote the improvement of the state of consciousness of these patients.
This programme was applied to 22 people/participants with an average age of 57,95 years-old (+ 17,27), being 63,64% male patients. The majority of the patients included the ones affected by hemorrhagic stroke (59,09%), followed by traumatic brain injury (31,82%). The two chosen methods were: the Glasgow Coma Scale (GCS) as well as Rancho los Amigos Levels of Cognitive Functioning Scale (LCSF) to assess patients.
After the data analysis, the results were as follows: more than half of the patients showed a clear improvement in their cognitive awareness, 63,64% increased the GCS score and 54, 55 in the LCSF. The patients whose families were effectively involved in the programme improved in average, six times more in the GCS.
We have come to the conclusion that the introduction of our multisensorial programme led to an improvement in most of these patients.
Keywords: Rehabilitation Nursing; Cognitive Awareness; Cognitive Rehabilitation; Multisensorial Stimulation Programme; Major changes in cognitive abilities
Implementámos um Programa de Estimulação Multissensorial (PEM) a doentes com alterações severas do estado de consciência, integrado num projeto de melhoria contínua da qualidade dos cuidados de enfermagem: “Avaliação e estimulação do doente com alterações do estado de consciência” (1). Tivemos como objetivo geral promover a melhoria do estado de consciência destes doentes.
Foi aplicado a 22 pessoas com média de idade de 57,95 anos (+17,27), sendo 63,64% homens. A tipologia de doentes foi maioritariamente AVC Hemorrágico (59,09%), seguida de Traumatismo Crânio-Encefálico (31,82%). Escolhemos a Escala de Coma de Glasgow (ECG) e a Rancho los Amigos Levels of Cognitive Functioning Scale (LCSF) para avaliar o doente.
Dos resultados destacamos: mais de metade dos doentes evoluíram no estado de consciência, 63,64% melhoraram o Score na ECG e 54, 55% progrediram no nível LCFS; os que tiveram a família envolvida evoluíram seis vezes mais em média na ECG.
Concluímos que com a aplicação do nosso PEM poderemos contribuir para a melhoria do estado de consciência da maioria destes doentes.
Descritores: Enfermagem de Reabilitação; Estado de Consciência; Reabilitação Cognitiva; Programa de Estimulação multissensorial; Alterações severas do estado de consciência
Se ha implementado un Programa de Estimulación Multisensorial (PEM) en enfermos con alteraciones severas del estado de conciencia, integrado en un proyecto de mejora continua de la calidad de los cuidados de enfermería: “Evaluación y estimulación del enfermo con alteraciones del estado de conciencia” (1). Su objetivo general fue la promoción de mejoras en el estado de conciencia de los enfermos.
Fue aplicado a 22 personas con edad media de 57,95 años (+17,27), 63,64% de los cuales eran hombres. La tipologia de los enfermos fue mayoritariamente AVC Hemorragico (59,09%), seguida de Traumatismo Craneo-encefálico (31,82%). Se ha elegido la Escala de Coma de Glasgow (ECG) y la Escala Rancho los Amigos Levels of Cognitive Functioning Scale (LCSF) para evaluar los enfermos.
De los resultados destaca que más de la mitad de los enfermos han evolucionado en su estado de conciencia, 63,64% han mejorado su score según la ECG y 54,55% progresaron su nivel según la LCFS; aquellos enfermos cuya familia se ha involucrado en el proyecto han evolucionado seis veces más según la ECG, promedia.
Se concluye que, con la aplicación del PEM se puede contribuir a mejorar el estado de conciencia de la mayoría de dichos enfermos.
Palabras clave: Enfermería en Rehabilitación; Estado de Conciencia; Rehabilitación Cognitiva; Programa de Estimulación multisensorial; Alteraciones severas del estado de conciencia
INTRODUCTION
Patients with severe brain injuries that in the past could not survive, nowadays, with all the existing technology at intensive care level, manage to resist, sometimes with serious consequences, namely in terms of the state of consciousness2. Patients in coma, vegetative state and minimal state of consciousness are included here (Table 1).
Table 1 Description of state of consciousness. Source: Adapted from Laureys S et al.,3; Giacino JT et al.,4; RCP5
| State of consciousness | Comportamental signals |
| Coma | It is not awake; absent or reflex motor activity. |
| Vegetative Status (VS) | Awake for periods, but with no visual fixation. Spontaneous reflex or behaviors, but without evidence of intentionality. |
| Minimum State of Conscience (MSC) | Start to be more alert. Visual fixation. Intentional, fluctuating but reproducible behavioral responses. According to the Aspen group, at least one of these behaviors: follow simple order; intelligible speech; purposeful behavior. |
As rehabilitation nurses in a neurosurgery service, when faced with these patients, we asked ourselves of how to cognitively rehabilitate patients during the global rehabilitation nursing program.
There are few studies dedicated to the subject, some indicate that the key lies in multisensory stimulation6.
Chipps et al., mentioned by Hoeman7 highlight the importance of stimulating the senses with known stimulus and refer as Rehabilitation Interventions in comatous patients, the introduction of controlled stimulus, including known strong odors and flavors (coffee, chocolate, salt, sugar); familiar sounds (voices of family members, favorite music); tactile stimulation with different textures and visual stimulation (colored cards).
For the neuroplasticity of the nervous system, sensory stimulation can contribute to the improvement of state of consciousness. Taylor8, a neuroscientist who suffered from a stroke, states that “the brain has an extraordinary ability to modify its connections based on stimulus that come to it from the outside. This “plasticity” of the brain underlies its ability to regain lost functions”. He also states: “neurons only develop when they are connected in a circuit with other neurons, isolated without stimulation, they wither away”. Monteiro9 summarizes that after neuronal injury or neural death, our brain looks for alternative axonal pathways that perform the same tasks, developing them. Royal Colleges of Physicians (RCP) in their Guidelines5 refer that some authors have used Sensory Stimulation Programs to try to increase responsiveness, taking into account that the brain develops and adapts through the use and the response to external stimulus.
The general aiming of our project was to promote the state of consciousness improvement on patients with severe state of consciousness changes, the first step towards their Cognitive Rehabilitation, through the application of a systematized Multisensory Stimulation Program, as it can reduce the duration of the coma, avoiding sensory deprivation.
METHOD
Taking into account the bibliography and the clinical practice, in 2015, in the Neurosurgery Service of the Hospital Garcia de Orta, a project for the continuous improvement of the quality of nursing care - Assessment and stimulation of the patient with changes in the state of consciousness1. The above project received the 1st prize in the Nursing Care Quality Standards competition from the Southern Regional Section of the Ordem dos Enfermeiros (Order of Nurses), which provided us with the acquisition of material to implement the program (Figure 1).
The general objective was to promote the improvement of the patient's state of consciousness, through the application of a systematized Multisensory Stimulation Program. Following our project, we elaborated the MSP (Table 2)10. The Glasgow Coma Scale was selected to assess the level of consciousness and also the first three levels of the LCSF (Table 3), in order to measure cognitive evolution. LCSF was developed and is mainly used in patients with traumatic brain injury (TBI). It features eight levels of progression of cognitive functioning, from no response to appropriate behavior. According to our clinical practice, they reflect the evolution that these patients go through. In our study, we used the first three levels as they correspond to severe changes in the state of consciousness. It has an easy and quick application with objectives for each level (Table 4) and also specific indications for stimulation, particularly useful for the family. We researched other scales, including the Coma Recovery Scale - Revised (CRS-R), which is very complete, but time-consuming to apply in the work context.
This resulted in a Regulation for the application of the MSP. The inclusion criteria were patients admitted to the Neurosurgery Service of Hospital Garcia de Orta, with a Glasgow Score (GS) less than 10, hemodynamic stability and intracranial pressure less than 15 mmHg in the last 24 hours. Exceptions: brain dead patients and those with sedation.
Table 2 PEM Main Items for Specialist Rehabilitation Nurses Source: The authors
| Sensory regulation of stimulus |
| Maintenance of a calm, peaceful and comfortable environment; organized (one at a time) and slow stimulation of the senses, with rest at the end; 15 to 45 min maximum. |
| Multisensory Stimulation |
| Auditory: normal tone of voice (do not infantilize); use the usual name; introduce yourself; orientate to space and time; give response time even if you don't yet; explain what you do; ambient music and/or headphones at the end (know the patient's taste) Smell: Pass along the nostrils known aroma for approximately 1 minute (personal perfume, coffee, lemon, pine, eucalyptus, vanilla, lavender…) Taste: Place drops of a pleasant known flavor on the tongue (coffee, sweet...) Visual: Show significant objects, if eye opening (photos of family/friends, children's drawings, TV, magazines with images, videos, optical fibers of various colors) Tactile and Proprioceptive: Passive muscle-articular mobilization with verbal stimulation for movement; massage; touch with different textures; bath in the bathtub stretcher. Vestibular: Balance training sitting on the edge of the bed, if allowed to stand up. |
| Involvement of family member/significant person |
| To explain that the person needs stimulus from the 5 senses, known and pleasing: images/videos/music from the cell phone; holding hands, applying cream, massaging, combing… Ask them to speak in a normal voice (not enfatilize). Reinforce that alternating periods of stimulation (not to exceed 45 minutes) with rest periods. |
Table 3 LCFS (Níveis I, II, III.) Source: Adapted from Hoeman S.,11; Simões J.,12; Rancho los Amigos13
| Level | Behavior | |
|---|---|---|
| I | No answer | Absence of patient response to any stimulus |
| II | General answer | Inconsistent, inappropriate, non-stimulation-specific reaction (chewing, sweating, blood pressure increase, polypnea, moaning, movements) |
| III | Local answer | More awake during the day and more movements. Specific but inconsistent response to stimulus (turns to a sound, runs away from pain, tries to observe someone moving in the room, starts to recognize family and friends, follows some simple instructions). |
Table 4 LCFS and objectives for levels. Source: Adapted from Hoeman S,7; Simões J,12
| Level | Behavior | Objectives |
|---|---|---|
| I | No answer | Raise conciousness; Activate response and decrease agitation. |
| II | General answer | |
| III | Local answer | |
| IV | Confused - agitated | |
| V | Confused-unreasonable | Activate an intentional and appropriate response. |
| VI | Confused-appropriate | |
| VII | Automatic-appropriate | Increase the ability to perform activities of daily living with little or no direct supervision. |
| VIII | Purposeful-appropriate |
RESULTS
From March 2016 to September 2018, the Multisensory Stimulation Programme(MSP) was applied to 22 patients (Table 5) who met the criteria described. Most were men, with a mean age of 57.95, between 21 and 84 years old. Most had a diagnosis of hemorrhagic stroke (59.09%), followed by TBI (31.82%) of which most were polytraumatized. Patients who underwent initial surgical treatment only started PEM after this.
Most started MSP in Intensive Care (6 patients) or Intermediate (9 patients) and the rest in wards(7 patients), as soon as they had met the inclusion criteria already described in the methodology.
Table 5 Sample characterization
| Variables | N | % | Average | Standard deviation | |
|---|---|---|---|---|---|
| Sex | Female | 8 | 36.36 | ||
| Male | 14 | 63.64 | |||
| Age | 57.95 | 17.27 | |||
| diagnostics | Hemorrhagic stroke | 13 | 59.09 | ||
| TBI | 7 | 31.82 | |||
| Brain tumour | 1 | 4.55 | |||
| ischemia bi-hemispheric after spine surgery | 1 | 4.55 | |||
Sessions were scheduled once a day, ranging from 1 to 28 per patient, with an average of 9.18. Of the total of 22 patients, 2 finished the program because they evolved favorably to a state of confusion and started to need other types of interventions, other than MSP (such as Reality Orientation Therapies). Unfortunately and despite already visible gains, even with few sessions, the program had to be interrupted in 14 of the patients because they were transferred and in other 6 because of death.
State of consciousness at the beginning and end of PEM
The majority started MSP in a Vegetative State (63.64%), followed by patients in coma (27.27%) and finally a minority in MSC (9.09%). In the last MSP session, no patient remained in coma, 31.82% presented with CME, 59.09% with vegetative state (VS) and 9.09% progressed to a state of confusion (Graphic 1).
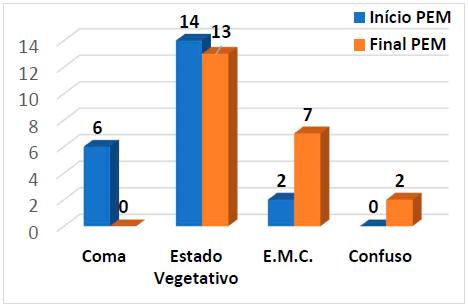
Graphic 1 Distribution of patients according to the State of Conscience at the Beginning and End of the MSP
By analyzing the evolution of each patient, we found that of the 6 in coma, all evolved, 4 of them after only 1 to 4 sessions and the rest in 8 to 11 sessions. Five evolved to the VS and one surpassed the MSC (went to the state of confusion). Of the 14 who started PEM in VS, five evolved to CME in 2 to 8 sessions, one to a state of confusion, and 8 kept the VS. The 2 patients who started with MSC maintained this status.
Glasgow score at the beginning and end of the MSP
The level of awareness on the Glasgow Coma Scale at the beginning of the MSP ranged between score 3 and 9, with a mean of 7. While at the end of the MSP it ranged between score 5 and 14, with a mean of 9. Most of the patients started the MSP with Score 7 or lower (63.64%). At the end of the MSP, most had a score equal to or greater than 8 (77.27%) (Graphic 2).
LCFS level at the beginning and end of MSP
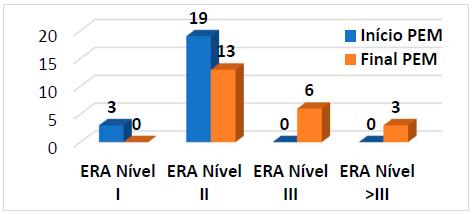
The vast majority of patients (86.36%) started MSP at level II of the LCFS and the rest (13.64%) started at level I. At the end of MSP, none remained at level I, just over half (59, 09%) stayed in level II, 27.27% stayed in level III and 13.63% went beyond level III and left the program (Graphic 3).
In the evolution of each patient, of the three patients who started MSP at level I of the LCFS, two progressed to level II and one to III. Of the 19 who started at level II, 10 remained at that level, 6 progressed to level III and 3 surpassed the latter. In total 54, 55% evolved.
Family involvement
The family of 55% of patients was actively involved in MSP. In these, the evolution in the GCS was in average 3.75 points, while in the others the evolution was an average of 0.6 points, that is, 6.25 more.
Behavioral reactions observed in the MSP application
We also registered different reactions to the applied stimulus. We highlight the power of the olfactory stimulus, even in patients in coma and VS, triggering chewing movements, eyelids (blinking, eyes widening), facial/grimaces, head, limbs and hyperventilation. We found that the reactivity to the olfactory stimulus decreased as the patient evolved in his state of consciousness. Upon gustatory stimulation, 14 patients, including those in coma, triggered chewing movements. To visual stimulus the observed reactions, including visual fixation and following stimulus, occurred in 4 patients in CME. and one in VS. 4 CME patients responded to verbal auditory stimulation with blinking and blinking, 2 coma patients responded with tears. One of the MSC patients moved all 4 limbs when seated (vestibular stimulus).
Further gains in functional independence
As already mentioned, in most cases the MSP was interrupted by patient transfer. All needed continuity of rehabilitation nursing care, namely and for this case, cognitive. The question arose as to how far they had progressed. So we went on, as far as possible, along its path. We highlight 3 cases that we know had gains in functional independence, which gives us encouragement to continue investing with our MSP, in these patients with serious neurological sequelae, as a starting point for their continued rehabilitation.
Case 1 - MLCA, female, 76 years old, hemorrhagic stroke due to aneurysm rupture. She started MSP in ICU, with mechanical ventilation, in a coma, GS 7, level I of the LCFS. Patient had 16 sessions, at the end of which she had SG 11 and LCFS level III, evolving to a state of confusion (GS 14). The two daughters were guided by us and actively involved in stimulation. From the observed reactions, we highlight the movement of the right upper limb (healthy side) to the olfactory stimulus, when in VS. She was transferred to another service, then to National Network of Continuous Integrated Care and finally to the Center for Physical Medicine and Rehabilitation (CMFR) in Alcoitão. According to data from the last neurosurgery appointment, patient lives with a daughter, has autonomous walking and some disorientation.
Case 2 - EMLF, female, 46 years old, hemorrhagic stroke due to aneurysm rupture. Patient started MSP in ICU, with mechanical ventilation, in a vegetative state, GS 6, LCFS level II. Patient had 9 sessions, at the end of which she had GS 12 (tracheostomized). The husband was very present and involved in the stimulation under our guidance. From the observed reactions, we highlight chewing movements to the taste stimulation of coffee in VS. Patient progressed even during hospitalization to GS 15 and started Activities of daily living (ADL) training. She was transferred to National Network of Continuous Integrated Care. We found, after the last neurosurgery consultation, living with her husband, presenting autonomous walking, being aware, oriented and independent in the ADL. As a curiosity, the patient, after being asked if she remembered any intervention by the MSP, said that currently couldn't even smell the coffee (Knowing patient appreciated it before) and that patient remembered some lights associating to Christmas lights (optical fibres).
Case 3 - RMFB, male, 21 years-old, severe TBI, started the MSP in Intermediate Care, in MSC, GS 9, level II of the LCFS. Patient had 28 sessions, evolving to GS 12, LCFS level III, maintaining the MSC. The mother was always present and very involved in the stimulation under our guidance. From the observed reactions, we highlight in chronological order: chewing movements to the olfactory stimulus, following with the eyes, moving the 4 limbs when sitting, turning the head to the side of the sound, response with blinking of the eyes, emission of guttural sounds in response to the stimulus verbal. Patient was transferred to the RNCCI and then to the Physical Medicine and Rehabilitation Center of S. Braz de Alportel. After the last neurosurgery consultation, we found that patient was living with his mother, had GS of 15, was walking in a wheelchair (patient reported being able to walk, although unstable, with support), presented with dysarthria and was undergoing oral feeding training, but still with Percutaneous Endoscopic Gastrostomy (PEG).
DISCUSSION
With this project, we wanted to optimize the cognitive rehabilitation of patients with severe changes in the state of conscious, through the application of a Multisensory Stimulation Program. It is therefore essential to evaluate and discuss the application of the MSP, the results obtained and the reactions observed.
Most of our patients had hemorrhagic stroke and TBI as diagnoses, which is in accordance with the main causes mentioned by the CPR Guidelines5.
MSP application
As for the structuring of our MSP, we considered it adequate, triggering some positive behavioral reactions and we did not observe undesirable reactions, as can occur in situations of sensory overload. In particular, we did not find adverse hemodynamic changes or autonomic dysfunctions. The RCP Guidelines5, in line with our program, state that in these patients, overstimulation and many stimulus must be avoided simultaneously, not to trigger sympathetic hyperactivity. They recommend that stimulation should focus on pleasant sensations (favorite music, gentle massage, pets) offered one at a time, for short periods, to minimize sensory overload. And they report that although the studies are not conclusive yet, due essentially to its methodology, controlled stimulation provides the best opportunity to observe responses.
As for our concern with sensory regulation, the data obtained in the study by Pinto14, through interviews with TBI patients who had been in a coma, also lead her to consider the regulation of cognitive stimulation as important, preferably with an emotional tone.
Tayler 8, neuroscientist, reported in the first person his recovery from a severe hemorrhagic stroke. She refers to the importance of various sensory stimulous combined with family monitoring and alerts for their sensory regulation, with an emphasis on the serenity of the environment and communication, on the need for well-deserved rest after rehabilitation. All these aspects are also included in our MSP.
According to the study by Sun et al.,15, the use of personalized objects seems to be more effective in triggering responses in patients with alterations in the state of conscious, compared to the use of non-personal objects, in the evaluation of the item “Use of Functional Objects” of the CRS-R scale, the difference being statistically significant. It was also our concern to integrate personal items in MSP.
In another study, by Laureys et al.,16, it was found that using the patient's name, in relation to the use of other sound stimulus, causes a broader activation at the brain level when using Positron Emission Tomography (PET).
Sharon17 studied the patient's reaction in VS to familiar faces through functional MRI. The author found that the activated regions were those related to emotional activities in the limbic area. This study showed that familiar stimulus, such as familiar faces, result in a greater number of responses.
The study by Heine et al.,18 concluded that favorite music and familiar voices have effects on these patients' cognitive and behavioral processes.
We found that in our MSP, the aspects referred to in these studies are covered there.
We also found that some studies focus more on the diagnostic assessment of the state of conscious, for clinical decision-making (for example, in the case of insurance companies) not taking into account that the stimulus applied in the tests will help the patient to progress.
Results of evaluation
With regard to the results obtained, we emphasize that, in more than half of the patients, we were unable to continue the program because they were transferred. It would be important for the MSP to be part of good practices in other institutions so that there was continuity of care. We trust that, at least, the family members we advised had some follow-up, as the results show that patients who had their family actively involved progressed more points in average on the GCS. Therefore we recommend encouraging family involvement whenever possible. As stated in the RCP Guidelines5, this involvement is a generally welcome opportunity for family and friends to play a positive role during visits.
The results of our MSP show that more than half of the patients evolved in their state of conscious (54.55%), in the GS (63.64%) and in the LCFS (54.55%). If the program had continued, how many more patients would evolve? In the study by Doman et al.,19, of the 200 patients with brain damage and GS equal to or less than 6, who underwent a MSP, 91% emerged from a coma. However, Lombardi et al.,20, when reviewing the literature on sensory stimulation in patients with brain injuries who were in a coma or VS, found that the few controlled studies that exist are of relatively low quality, and therefore not the effectiveness of these programs can be clearly demonstrated.
Also Cabral et al.,6, in a literature review, concluded that there is still no scientific proof of the effectiveness of MSP.
Observations during MSP application
It was with the olfactory stimulus that we observed more reactions, especially in patients in coma and VS. We know from neurophysiology that smell has direct access to the brain without going through the thalamus as in other directions21.
Freiherr22 states that olfactory information not passing through the thalamus, on its way to the neocortex, may be the reason for the multiplicity of unconscious processes involved in olfactory perception. The olfactory system is strongly connected with the limbic system, resulting in responses to odors with a strong emotional tone and a robust relationship with memory processes. These characteristics of the olfactory system form the basis of the perception of smell that makes it unique, among other sensory perceptions.
The fact that olfactory and gustatory reactions are evident even in patients in coma, goes against what Caldas23 mentions, about smell and taste, “they seem to be felt with functions that are more disconnected from cognition and more adapted to the information of more primitive systems of nervous function”.
CONCLUSION
We conclude that MSP can contribute to improving the state of conscious of most patients with severe changes in the state of conscious. Our experience with this project leads us to advocate the involvement of the family as an important supporter of the MSP. Also, family stimulus, due to their emotional richness, are crucial to trigger behavioral responses in these patients.
The olfactory stimulus, due to the observed reactions and knowing that it has a direct circuit to the brain, which prints a strong emotional tone and is related to memory processes, could be of great importance for the awakening of conscious, requiring further investigation.
There are few studies, not always recent and with a methodology that does not allow to clearly prove the effectiveness of multisensory programs. However, there are more recent and reliable studies15,17,18 on specific stimulous, but more with the aim of diagnostic evaluation.
By carrying out this project and analyzing its results, we intend to contribute to the development of good practices in cognitive rehabilitation nursing care for these patients and make new contributions to know the impact of applying a MSP in patients with severe disorders of the state of conscious, motivating future studies.
It is, therefore, important to continue to research to what extent these programs contribute to the cognitive rehabilitation of these patients.
REFERÊNCIAS
1 Varanda E, Rodrigues CA. Avaliação e estimulação do doente com alterações do estado de consciência: Projeto de melhoria contínua da qualidade dos cuidados de enfermagem. Ordem dos Enfermeiros. 2015. Disponível em: https://www.ordemenfermeiros.pt/arquivo/projectos/Documents/Projetos_Melhoria_Qualidade_Cuidados_Enfermagem/HospitalGarciaOrta_AvaliacaoEstimulacaoDoenteComAlteracoesEstadoConsciencia.pdf [ Links ]
2 Demertzi A, Laureys S, Bruno A. Ethics in Disorders of Consciousness. Jl Vincent(ed.), Annual Update in Intensive Care and Emergency Medicine. Springer. 2011. [ Links ]
3 Laureys S, Owen AM, Schiff N. Brain function in coma, vegetative state, and related disorders. Lancet Neurol. 2004; 3: 537-546. Disponível em: http://www.coma.ulg.ac.be/papers/vs/PVS_MCS_LIS_LancetN04.pdf [ Links ]
4 Giacino JT, Ashwal S, Childs N, et al. The minimally conscious state: Definition and diagnostic criteria. Neurol. 2002; 58: 349-353. Disponível em: https://pdfs.semanticscholar.org/21d1/d1961a0496ad1edc7ccbd471e93025a15459.pdf [ Links ]
5 Royal College of Physicians. Prolonged disorders of consciousness. National clinical guidelines. London. RCP Rev. 2018. [ Links ]
6 Cabral FA, Pompeu SM, Apolinário A, Pompeu JE. Estimulação Multissensorial em pacientes comatosos: uma revisão da literatura. Revista o Mundo da Saúde. São Paulo. 2008; 32 (1): 64-69. [ Links ]
7 Hoeman S. Enfermagem de Reabilitação: Aplicação e processo. (2ª Edição). Loures: Lusociência. 2000: 635-184. [ Links ]
8 Taylor J. O dia em que a minha vida mudou. Lisboa: Editorial Presença. 2008. [ Links ]
9 Monteiro A, Oliveira C, Pereira C, et al. A oculta face do coma: o despertar do desconhecido. Loures: Lusociência. 2013: 31-37. [ Links ]
10 Varanda E, Rodrigues CA. Reeducação cognitiva em Enfermagem de Reabilitação: Recuperar o Bailado da Mente. In C. Marques-Vieira, L Sousa (Eds). Cuidados de Enfermagem de Reabilitação à pessoa ao Longo da vida. Loures: Lusodidacta. 2017: 219-221. [ Links ]
11 Hoeman S. Enfermagem de Reabilitação: Prevenção, intervenção e resultados esperados. Loures: Lusociência. 2011: 556 [ Links ]
12 Simões J. A influência da estimulação auditiva na pessoa em coma. Universidade de Aveiro. 2011. [ Links ]
13 Rancho los Amigos National Rehabilitation Center. Family Guide to The Rancho Levels of Cognitive Functioning. Disponível em: http://file.lacounty.gov/dhs/cms1_218115.pdf. [ Links ]
14 Pinto V. Coma Provocar a consciência num movimento espiral. Loures: Lusodidacta. 2014. [ Links ]
15 Sun y, Wang J, Heine L, et al. Personalized objects can optimize the diagnosis of EMCS in the assessment of functional object use in the CRS-R: a double blind, randomized clinical trial. BMC Neurol. Dec;18(1):38. Disponível em: https://doi.org/10.1186/s12883-018-1040-5 [ Links ]
16 Laureys S, Perrin F, Faymonville ME, et al. Cerebral processing in the minimally conscious state. Neurol.2004:63(5): 916-8 https://bmcneurol.biomedcentral.com/articles/10.1186/s12883-018-1040-5 [ Links ]
17 Sharon H, Pasternak Y, Ben S. et al. Emotional processing of personally familiar faces in the vegetative state. Plos One. 2013; 8(9) e74711. Disponivel em: [ Links ]
18 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3783455/ [ Links ]
19 Heine L, Castro M, Martial C, et al. Exploration of functional connectivity during preferred music stimulation in patients with disorders of consciousness. Front Psychol. 2015; 6: 1704. Disponivel em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4637404/ [ Links ]
20 Doman G, Wilkinson R, Dimancescu MD et al. The effects of intense multi-sensory stimulation on coma arousal and recovery. Neuropsychol Rehabil. 1993; 3:203-12. [ Links ]
21 Lombardi F, Taricco M, Tanti A, et al. Sensory stimulation for brain injured individuals in coma or vegetative state. Cochrane Database Syst Rev. 2004;(2) [ Links ]
22 Nolte J. Neurociência. Arizona: Elsevier. 2008: 155. [ Links ]
23 Freiherr J. Cortical Olfactory Processing. In Buettner A. (Ed). Springer Handbook of Odor. Germany: Spinger. 2017: 764-766. [ Links ]
24 Caldas AC. A Herança de Franz Joseph Gall. O Cérebro ao serviço do comportamento humano. Lisboa: Mc Graw Hill. 2000: 83. [ Links ]
Received: December 04, 2018; Accepted: November 27, 2019











 text in
text in