Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Portuguesa de Enfermagem de Reabilitação
Print version ISSN 2184-965XOn-line version ISSN 2184-3023
RPER vol.2 no.2 Silvalde Dec. 2019
https://doi.org/10.33194/rper.2019.v2.n2.4581
Articles
Rehabilitation of Respiratory Function in person with bacterial pneumonia secondary to Influenza A: case study
1- Hospital Professor Doutor Fernando da Fonseca
3- Escola Superior de Saúde Atlântica
Background:
The autumn and winter months are associated with an increase in the seasonal epidemic flu responsible for 3 to 5 million cases of serious illness. Secondary bacterial infection is the most frequent complication, with high hospitalization rates. The rehabilitation nurse is recognized for being specialist in therapeutic interventions to provide the recovery of the person with respiratory pathology.
Objective:
To identify health outcomes from rehabilitation nursing care associated with the optimization of the respiratory function in a person diagnosed with streptococcus pneumonia community-acquired pneumonia secondary to Influenza A infection.
Method:
Qualitative case study research type. The study highlights the nursing care using the Padrão Documental dos Cuidados da Especialidade de Enfermagem de Reabilitação in an elderly person with altered respiratory function is presented, necessitating oxygen therapy and with its ability to expectorate compromised. The ethical principles in research have been fulfilled.
Results:
The implementation of the intervention plan constituted by four days revealed a reduction in the sensation of dyspnea; reduction of oxygen therapy; reduction of secretions; improvement in pulmonary auscultation of the vesicular murmur.
Conclusions:
It is verified that the implementation of an individualized rehabilitation nursing care plan can contribute significantly to promote the recovery of the person with restrictive respiratory pathology.
Keywords: Breathing Exercises; Bacterial Pneumonia; Rehabilitation Nursing; Case Reports
Introdução:
Os meses de Outono e Inverno estão associados a um aumento da epidemia sazonal da gripe responsável por 3 a 5 milhões de casos de doença grave. A sobre-infeção bacteriana secundária assume-se como a complicação mais frequente, com elevados índices de internamento. Aos enfermeiros especialistas em enfermagem de reabilitação são reconhecidas capacidades mediante um conjunto de intervenções terapêuticas para proporcionar a recuperação da pessoa portadora de patologia respiratória.
Objetivo:
Identificar os ganhos em saúde sensíveis aos cuidados de enfermagem de reabilitação na otimização da função respiratória numa pessoa com o diagnóstico de pneumonia adquirida na comunidade por streptococcus pneumoniae secundária à infeção por Influenza A.
Método:
Estudo de abordagem qualitativa, tipo estudo de caso. Consiste na utilização do processo de enfermagem, com recurso ao Padrão Documental dos Cuidados da Especialidade de Enfermagem de Reabilitação. É apresentado o caso de uma pessoa idosa com alteração da função respiratória, necessitando de oxigenoterapia e capacidade de expetorar comprometida. Foram cumpridos os princípios éticos em investigação.
Resultados:
Com a implementação do plano de intervenção constituído por quadro dias, foram verificados ganhos na redução da sensação de dispneia; redução do aporte de oxigenoterapia; redução da quantidade de secreções; melhoria na auscultação pulmonar do murmúrio vesicular.
Conclusões:
Verifica-se que com a implementação de um plano de cuidados de enfermagem de reabilitação individualizado pode-se contribuir significativamente na promoção da recuperação da pessoa com patologia respiratória restritiva.
Descritores: Exercícios Respiratórios; Pneumonia Bacteriana; Enfermeiro Especialista em Enfermagem de Reabilitação; Relatos de Casos
Introducción:
Los meses de otoño e invierno están asociados a un aumento de la epidemia estacional de la gripe responsable de 3 a 5 millones de casos de enfermedad grave. La sobre-infección bacteriana secundaria se asume como la complicación más frecuente, con altos índices de internamiento. A los enfermeros especialistas en enfermería de rehabilitación se les reconocen capacidades mediante un conjunto de intervenciones terapéuticas para proporcionar la recuperación de la persona portadora de patología respiratoria.
Objetivo:
Identificar los resultados de salud sensibles a los cuidados de enfermería de rehabilitación en la optimización de la función respiratoria en una persona con el diagnóstico de neumonía adquirida en la comunidad por streptococcus pneumoniae secundaria a la infeción por Influenza A.
Método:
Estudio de enfoque cualitativo, tipo estudio de caso. Consiste en la utilización del proceso de enfermería, con recurso al Padrão Documental dos Cuidados da Especialidade de Enfermagem de Reabilitação. Se presenta el caso de una persona anciana con alteración de la función respiratoria, necesitando de oxigenoterapia y capacidad de expetorar comprometida. Se han cumplido los principios éticos en investigación.
Resultados:
Con la implementación del plan de intervención constituido por cuadro días, se verificaron beneficios en la reducción de la sensación de disnea; reducción del aporte de oxigenoterapia; reducción de la cantidad de secreciones; mejora en la auscultación pulmonar del murmullo vesicular.
Conclusiones:
Se verifica que con la implementación de un plan de cuidados de enfermería de rehabilitación individualizada se puede contribuir significativamente a la promoción de la recuperación de la persona con patología respiratoria restrictiva.
Descriptores: Ejercicios Respiratorios; Neumonía Bacteriana; Enfermero Especialista en Enfermería em Rehabilitación; Informes de Casos
INTRODUCTION
Extreme and intense climatic phenomena are currently an increasingly frequent reality, with serious consequences for the health of the population, reflected in the increase in morbidity and mortality experienced in these periods1. The autumn and winter months are associated with an increase in the seasonal influenza epidemic, which despite being an acute respiratory disease and mostly benign, in some cases may have a more severe evolution (implying an increase in demand for health services) annually responsible for 3 to 5 million cases of severe disease and for 250,000 to 500,000 deaths worldwide1,2. In Portugal, epidemiological surveillance is carried out by the Sentinel Medical Network in collaboration with the National Reference Laboratory for the Influenza Virus and Other Respiratory Viruses in the Department of Epidemiology of the Ricardo Jorge Institute, issuing weekly surveillance bulletins. According to them, for the 2018/2019 season there was an increase in the incidence rate beginning on December 3, 2018, assuming epidemic flu activity between January 21 and 27, 2019, with an incidence rate of 89.3 per 100,000 inhabitants due to the circulation of subtype A3.
Influenza virus infection, in addition to increasing the risk of exacerbating chronic diseases, presents as the most frequent complication secondary to bacterial overinfection, mainly caused by Streptococcus pneumoniae, Haemophilus Influenzae and Staphylococcus aureus1,4.
Pneumonia is an infection of the lung parenchyma in which all or part of the alveoli are filled with fluid and erythrocytes, conferring the designation of pulmonary consolidation, replacing both the air available in the alveoli and the area available for gas exchange. This is a phenomenon that gives it a restrictive pattern due to the reduction in pulmonary compliance, reflected in an increase in respiratory rate, a reduction in tidal volume and in the ventilation-perfusion index5.
Pneumonia (n=40345) is assumed in Portugal as the main cause of hospitalization for respiratory disease in 2016, followed by chronic obstructive pulmonary disease (n=7864) and lung cancer (n=5541)6. Pneumonia is responsible for 7% of hospital admissions, with an increased prevalence in patients aged 80 years-old and over, with high percentages of morbidity and mortality, the latter being at 20%6.
Community-acquired pneumonia is one that has its origin in the community or that manifests within 48 hours after the person is hospitalized. Commonly, the person presents with chest pain, fever, dyspnea, cough, initially mucous and progressively purulent sputum, and chills. Pulmonary auscultation is marked by the presence of audible crackling ferns in both breaths, although more intense in the inspiratory phase and often in the posterior phase of the thorax at the level of the middle lung fields, simulating "hair squeezing between the fingers"7,8. The presence of consolidations is identified by a hyporesonance to percussion9 and an increase in the thoraco-vocal shiver on palpation5.
In situations of hospitalization of a person with community-acquired pneumonia, the person should undergo control by chest teleradiography and arterial blood gas. Chest teleradiography is an essential means of diagnosis in this area, providing information on the lung parenchyma, mediastinum, bone structures and soft tissues5. In community-acquired pneumonia, the image of pulmonary consolidation is frequently present in the lower lobes, as well as the presence of a diffuse interstitial infiltrate resulting from the inflammatory process8. Arterial blood gas analysis allows the assessment of oxygen concentrations, the effectiveness of gas exchange between the alveoli-capillaries and acid-base balance, being a method for controlling the clinical evolution and determining the need for additional oxygen5.
Therapeutic treatment of community-acquired pneumonia is based on antibiotic therapy directed at the specific microorganism, and due to the need for an early start, it turns out to be empirical. In addition to antibiotic therapy, this treatment should be complemented with the administration of oxygen, nutritional support and prevention and treatment of possible associated metabolic disorders7,8. Inhalation therapy, as the preferred route, is also assumed to be effective in the treatment and prevention of secretion stasis. Given the situation, there is a wide variety of therapies such as saline, bronchodilators, anti-inflammatory drugs, mucolytics and antibiotics, with equal therapeutic effects compared to other routes of drug administration, in addition to a reduction in adverse effects8.
The rehabilitation nurse (RN) is the health professional who is recognized for the ability to provide a set of therapeutic interventions (with emphasis on non-pharmacological ones) with the aim of improving residual functions, maintaining and recovering independence in life activities and minimize the impact of disabilities in terms of neurological, respiratory, cardiac, orthopedic, impairments and incapacities10.
In this sense, respiratory rehabilitation, as a holistic process that gives the person a full physical, mental, emotional, social and professional state, has become a standard of care recommended to people with respiratory pathology in its chronicity and/or exacerbation5, with the RN recognized as having specialized competences in the implementation of respiratory functional re-education programs, also called respiratory kinesitherapy11.
Currently, it is shown that respiratory rehabilitation reduces the symptoms presented, improving limb muscle function, exercise capacity, emotional function, quality of life, knowledge and self-efficacy, being considered an essential component in the integrated care of patients supported by better cost-effectiveness, reduced hospitalizations and reduced health costs12.
Respiratory functional re-education is a non-invasive therapy with no harmful adverse effects, encompassing a set of techniques based on breath control, positioning and movement aimed at better efficiency in gas exchange and symptom reduction, complementing the established pharmacological treatments5,12.
The intervention of respiratory rehabilitation in people with community-acquired pneumonia is dependent on the stage of the disease, and should be intervened after stabilization of severe hyperthermia and hemodynamic instability. In the initial phase, the intervention aims to reverse the volume reduction in the lung segments and prevent atelectasis and the consequent reduction in the ventilation-perfusion index, while as the disease progresses to its resolution, there is a reduction in the consolidation of lung fields and the occurrence of productive cough with secretions5,8. The objective of the RN intervention focuses on optimizing ventilation with lung reexpansion, with special attention to the prevention and correction of postural changes; in the permeability of the airways with the drainage of secretions and promotion of an effective cough; the reduction of respiratory work and effort re-education5,8.
The intervention of the RN should be based on the initial assessment of the person and the symptoms presented, complemented by imaging and clinical observation8. The ventilation focus is compromised by its restrictive nature, providing hypoventilation patterns, decreased inspiratory muscle action and increased respiratory effort5. To enhance lung re-expansion, it is necessary to modify ineffective breathing patterns based on techniques that make the person aware of ventilatory dynamics and mechanics. Techniques for correcting ventilatory asynergy and optimizing alveolar ventilation should be established, such as the control and dissociation of respiratory times; abdomino-diaphragmatic breathing; exhalation with the lips half-closed; thoracic and joint mobilization; abdomino-diaphragmatic re-education; selective and global costal re-education; respiratory muscle training with emphasis on inspiration and controlled inspiratory flow exercise11. Within the focus expectorate, this shows a decrease in its effectiveness associated with pathophysiological changes in the airways, mucociliary system and the decrease in the strength of the inspiratory and expiratory muscles, also contributing to the impairment of ventilation and, consequently, of the respiratory function. A set of techniques such as effective coughing are included for this focus; drainage of secretions with accessory maneuvers; postural drainage; autogenic drainage; huffing and the forced expiration technique and active cycle of breathing techniques11.
The bibliography refers to little scientific evidence about the real benefits of functional respiratory reeducation in people with pneumonia, although the intervention remains considerably applied5. In view of the above, this case study presents the guiding question: “What is the contribution of the Specialist Nurse in Rehabilitation Nursing in the respiratory function of a person with bacterial pneumonia secondary to viral infection by Influenza A?”.
This case study presents the general objective of evaluating the impact of the RN intervention, with the application of respiratory functional reeducation, in people with bacterial pneumonia secondary to viral infection by Influenza A.
For the purpose of the study, the following specific objectives are identified:
MATERIAL AND METHODS
The case study consists of a structured research method for knowledge of individual or group phenomena. For Yin, this is an empirical research when the limits between the phenomenon and context are not evident, with the objective of exploring, describing, and explaining the event13. In Nursing research, the case study allows that, through different sources of evidence, it is possible to study highly complex life phenomena13.
This case study is structured according to the theoretical frameworks of Yin and Stake in six stages: Problem definition; Case definition; Theoretical foundation; Preparation of the study protocol; Data collection; Analysis and discussion of results13.
In this case study, a person with Streptococcus pneumoniae Pneumonia secondary to viral infection by Influenza A is presented, addressing the rehabilitation program of the respiratory function during hospitalization in order to show the results obtained. Data collection was performed through anamnesis and consultation of the clinical file.
The respiratory rehabilitation program took place in February 2019 with the beginning of admission to hospital. The person was designated as an individual in order to safeguard data confidentiality and anonymity. In this way, due to the involvement of personal, non-transferable and confidentiality issues of the hospital clinic, it became essential to respect the ethical guidelines for nursing research, following the principles of Beneficiency; No Malefficiency; Loyalty; Justice; Veracity and Confidentiality, thus informing about the risks and benefits14. Informed consent was obtained prior to data collection.
The specific instruments for the assessment of respiratory function were based on the Guiding Guide for the Good Practice for Respiratory Rehabilitation of the Ordem dos Enfermeiros (Nursing Council). Thus, the assessment was incident on the Pathological Process, based on signs and symptoms of respiratory pathology: chest pain, measured by the Numerical Pain Scale; Dyspnea, measured by the Modified Borg Scale; coughing and sputum due to the macroscopic aspect and the Body Process, carrying out the assessment of respiratory function through physical examination (inspection, palpation, percussion and auscultation), arterial blood gas and chest teleradiography.
The results shown in this study approach a person who presented as selection criteria: elderly people, aged 65 years-old or over; absence of known personal respiratory history and Influenza A infection in the current hospitalization.
Case presentation
Anamnese
Resulting from the information obtained in the anamnesis, it directs the health professional towards the diagnosis and respective therapeutic plan. It should consist of information related to past history, family and socioeconomic history and current clinical history9.
This case corresponds to an individual, 90 years-old, male, Caucasian and of Portuguese nationality, married, residing with his wife and child. Currently retired, having worked as an electrical engineer. Patient went to the emergency department on February 3, 2019 due to fever, dyspnea, productive cough with the presence of whitish sputum, rhinorrhea, chest pain in the infracostal region with pleuritic characteristics and myalgia with five days of evolution. Upon arrival at the emergency department, presented a fever peak of 39.2°C. Complementary exams were performed, verifying an arterial blood gas analysis performed with oxygen supply at 3L/min through nasal glasses with a pH of 7.45; pCO2 35mmHg; pO2 58mmHg; 3.5mml/L lactates and 24.3 mmol/L HCO3, a chest cephalogram described as “bilateral peri-hilar reinforcement. Permeable costus and cardiophrenic sinuses, without images suggestive of condensation”, a nasal exudate positive for Influenza A and a positive antigenuria for Streptococcus pneumoniae.
He is transferred on February 4, 2019 to hospital and the oxygen supply is increased to 5L/min through nasal cannula.
The individual has known personal history of high blood pressure and Crohn's disease. Usual medication: Messalazine 100mg, twice a day; Rifaximin 200mg twice daily; Pravastatin 20mg/day. No allergies Known.
Regarding the performance of his activities of daily living, patient was independent until the date of hospitalization, practicing regular physical exercise three times a week in the gym. In terms of socio-family and housing, does not present with economic difficulties and resides on the 3rd floor of a building with an elevator.
Rehabilitation Nursing Assessment
For an efficient performance of the RN in the implementation of its performance, it is necessary to associate the data obtained through anamnesis with the observation of complementary diagnostic tests and a physical examination of the person with respiratory pathology, taking into account details that may go unnoticed8,9. The rehabilitation plan began on February 14, 2019, and the respective interventions were implemented until February 21, 2019. The individual was discharged from the clinic on February 22, 2019.
The physical examination, based on the four stages mentioned above, as well as the complementary means of diagnosis allow the identification of the stage of the disease and the consequent elaboration of nursing diagnoses, adapting the intervention and emphasizing the alterations presented by the person. These instruments, according to the scientific evidence recommended by the American Association of Cardiovascular & Pulmonary Rehabilitation, were applied before and after the implementation of the respiratory functional reeducation program, allowing the identification of sensitive gains in rehabilitation nursing care. In restrictive pathology, scientific studies reveal that the effectiveness of respiratory rehabilitation is scarce, essentially focusing on the functional status and reduction of dyspnea5.
The interventions focused on aerobic and resistance exercises are currently considered as the modality that provides the most benefits to people with pneumonia5. Their monitoring was continuous, based on peripheral oxygen oximetry (SpO2) and heart rate values, in addition to the previously mentioned Modified Borg Scale.
Nursing diagnoses
According to the ICNP® language, and within the scope of the respiratory function rehabilitation program, four nursing diagnoses were identified related to the “ventilation” and “expectation” focuses:
Respiratory Function Rehabilitation Program
Nursing interventions appropriate to the diagnoses defined by the assessment of respiratory function, based on what is recommended by the Documental Standard of Nursing Care of the Rehabilitation Nursing Specialty15 and Guiding Guide for Good Practice of Respiratory Rehabilitation5, are presented in table 1.
Through the set of nursing interventions presented, associated with a holistic look at the person targeted by the established care, other nursing diagnoses were also enunciated, such as intolerance to compromised activity and reduced muscle movement.
The interventions were ensured in the various sessions held, lasting between 30 and 45 minutes.
Table 1 List of Nursing Diagnoses and Interventions5 , 15 )
| Nursing diagnosis | |
|---|---|
| Impaired ventilation, in a moderate degree | |
| Nursing interventions | - To observe chest [color, deformations, symmetry, before and after intervention]; - Auscultate the chest [identify breathing sounds and adventitious sounds, before and after intervention]; - To monitor ventilation [expansibility, type, rhythm, amplitude, inspiratory and expiratory times, rescue of accessory muscles, before and after intervention]; - To monitor [peripheral oxygen oximetry (SpO2)]; - To monitor respiratory rate; - To observe the exam [arterial blood gas and chest teleradiography]; - To encourage the use of breathing devices [incentive spirometer]; - To optimize ventilation through the positioning technique [resting position and relaxation techniques; Headboard at 30-45º; Postural correction]; - To perform breathing techniques [control and dissociation of breathing times; exhalation with semi-closed lips, 2 sets of 10 repetitions; abdominodiaphragmatic re-education with 1kg resistance; bilateral lower costal reeducation]; - To perform respiratory kinesitherapy [exercise of rotation of the humeral scapula; global costal opening with stick, 2 sets of 10 reps; selective costal opening; thoracic and joint mobilization with respiratory control and emphasis on inspiration - stretching, active chest mobilization with and without therapeutic ball, shoulder adduction/abduction in the horizontal plan and sagittal axis in the standing position; kinetic chain anterior flexion of the pelvis to the bottom of the bed, 1 series of 10 repetitions]. |
| Ineffective expectorating | |
| Nursing interventions | - To evaluate cough reflex; - To encourage coughing; - To encourage fluid intake; - To perform inhalation therapy through an inhaler; -To perform respiratory kinesiotherapy [chest vibration technique, chest percussion technique, chest compression technique]; - To assist in coughing [assisted cough, directed cough]; - To watch over the sputum. |
| Potential to improve knowledge of cough technique | |
| Nursing interventions | - To assess knowledge about cough technique; - To teach about coughing technique [assisted cough: sitting or head-up position, with controlled diaphragmatic breathing and emphasis on deep breaths. Close the glottis and contract the abdominals. Vigorous manual compression assisted by a professional, at the beginning of the expiratory phase, on the hypogastric or lower costal region. The pressure applied is quick and applied 2 to 3 times, increasing chest compression, stimulating coughing; Directed cough: sitting position and feet flat, trunk leaning forward. Inhales through the nose as if to “smell the flower”, compresses the abdomen with the upper limbs hugging a pillow, with the trunk bent and coughing; Huffing and forced expiration technique] |
| Potencial to improve capacity to emply cough technique | |
| Nursing interventions | - To assess ability to use the cough technique; - To instruct about cough technique [assisted coughing; directed cough; Huffing and forced expiration technique] - To train the cough technique |
RESULTS
The individual's respiratory function rehabilitation program included a total of four sessions, all of which were alert and very participatory in the implemented interventions.
The evaluation of the results obtained from the interventions of the rehabilitation program took place as defined by the Guiding Guide for Good Respiratory Rehabilitation Practice, starting with the assessment of the pathological process, giving a subjective assessment of the respiratory function, through the signs and symptoms presented5. Pain assessment was performed using the Numerical Pain Scale (Table 2). The individual rated pain level 0, before and after the intervention.
Table 2 Results of the assessment using the numerical pain scale
| Date (2019) | 14/02 | 18/02 | 20/02 | 21/02 |
|---|---|---|---|---|
| Pre-intervention intensity | 0 | 0 | 0 | 0 |
| Post-intervention intensity | 0 | 0 | 0 | 0 |
Dyspnea is experienced as respiratory distress. This discomfort was continuously monitored by the individual, using the Modified Borg Scale. Its result was recorded throughout the sessions, before the intervention and after a period of rest. Its monitoring during the established plan did not limit the performance of the outlined exercises, verifying that there was a gradual improvement in effort tolerance (Graphic 1). In the first sessions, there is an explicit greater respiratory discomfort and tiredness expressed by the individual, which progressively diminished, stating “I don't feel tired at all” after a period of rest at the end of the session (Graphic 1).
Initially, the cough was productive and ineffective, failing to expel secretions. This data showed the need for an adjustment in the validation process of knowledge and ability to use the cough technique. Coughing became more effective in the 2nd session, with better mobilization of secretions, which despite being in small quantities, allowed their elimination (Table 4). The characteristics of the secretions were possible to be evaluated during the planned exercises, presenting themselves as thick and mucopurulent. With the acquisition of the ability to use the technique of assisted and progressively directed coughing, associated with nebulization with previous saline solution, there was better fluidity of the same, ending up in the last session as there were only dry cough accesses (Table 3).
Table 3 Assessment of the knowledge and learning of skills dimension of the expector focus
| Nursing diagnosis | 14/02 | 18/02 | 20/02 | 21/02 |
|---|---|---|---|---|
| Potential to improve knowledge of cough technique | ND | D | D | D |
| Potential to improve ability to use cough technique | ND | D | D | D |
Subtitle: D - Demonstrate; ND - Not demonstrate.
As part of the assessment of the body process, a systematic assessment was carried out in order to identify pathophysiological changes during the evolution of the pathology, as well as the implemented interventions. This assessment consisted of a physical examination which included inspection, palpation, percussion and auscultation.
The inspection essentially focused on the evolution of the breathing pattern, the presence of respiratory distress and postural deformities.
It was found that, at first, the individual had the need to resort to the use of accessory muscles of breathing, which provide with greater muscle tension. Although there were no thoracic asymmetries and absence of spinal deformities, a constant elevation of the shoulders and shoulder blades was notable, which simultaneously conferred a stressful posture, reflected in the subjective perception of dyspnea. Progressively, with the measures adopted for postural correction and relaxation techniques, it stopped resorting to accessory muscles associated with a more regular breathing pattern and a type of breathing with emphasis on diaphragmatic excursion and, consequently, on the inspiratory phase. This fact was possible with the synchrony and collaboration obtained in the dissociation of respiratory times, in the 2nd session (Table 4).
Table 1 Inspection Evaluation Results
| Date | 14/02/19 | 18/02/19 | 20/02/19 | 21/02/19 | ||||
|---|---|---|---|---|---|---|---|---|
| Start | End | Start | End | Start | End | Start | End | |
| Oxygen supply (L/min) | 5 | 5 | 3 | 3 | 2 | 2 | 2 | 1 |
| Aerosol therapy | N | N | N | N | S | N | S | N |
| Chest symmetry | S | S | S | S | S | S | S | S |
| Chest deformations | N | N | N | N | N | N | N | N |
| Breath Type | M | M | M | M | AD | AD | AD | AD |
| Rhythm | I | I | I | R | R | R | R | R |
| Amplitude | D | D | D | D | D | NO | NO | NO |
| Accessory muscles | S | N | S | N | N | N | N | N |
| Coughing | IN/P | IN/P | IN/P | EF/P | EF/P | EF/P | SE | SE |
| Secretions | NA | MP | NA | MP | NA | MP | NA | NA |
| Viscosity | NA | ES | NA | ES | NA | ES | NA | NA |
Subtitle: S - Yes; N - No; NO - Normal; D - Decreased; R - Regular; I - Irregular; M - Mixed; AD - Abdominodiaphragmatic; MP - Mucopurulent; ES - Thick; IN- Ineffective; EF - Effective; P - Productive; SE - Drought; AU - Absent; NA - Not evaluated.
Constant weaning from oxygen supply, through follow-up and medical prescription, was tolerated, not limiting both the number of sets and repetitions in the following sessions, as well as in the assessment using instruments such as the Modified Borg Scale. Through palpation, a bilateral evaluation of the chest and diaphragm was performed, essential for the follow-up of the evaluation of chest elasticity, which was found to be slight. During the sessions, the thoraco-vocal tremor showed an increase felt in the later phase, more incident in the bases, not registering a significant reduction with the accompanying expulsion of secretions (Table 5).
Percussion showed results aimed at different densities of lung fields. In the four sessions carried out, it was verified that the sound was never compromised at the apical level. On the other hand, and in a characteristic way in this pathology, dullness was found bilaterally installed in the bases and only in the last two sessions was there a slight clear pulmonary sound (Table 6).
Table 2 Results of palpation assessment
| Date | 14/02/19 | 18/02/19 | 20/02/19 | 21/02/19 | ||||
|---|---|---|---|---|---|---|---|---|
| Start | End | Start | End | Start | End | Start | End | |
| Centralized trachea | S | S | S | S | S | S | S | S |
| Elasticity | D | D | D | D | D | M | M | M |
| Thoraco-Vocal Fremit: | Anterior face of the chest | |||||||
| 1/3 Superior Right | M | M | M | M | M | M | M | M |
| 1/3 Middle Right | M | M | M | M | M | M | M | M |
| 1/3 Bottom Right | M | M | M | M | M | M | M | M |
| 1/3 Top Left | M | M | M | M | M | M | M | M |
| 1/3 Middle Left | M | M | M | M | M | M | M | M |
| 1/3 Bottom Left | M | M | M | M | M | M | M | M |
| Thoraco-Vocal Fremit: | Posterior face of the chest | |||||||
| 1/3 Superior Right | M | M | M | M | M | M | M | M |
| 1/3 Middle Right | A | A | A | A | A | A | M | M |
| 1/3 Bottom Right | A | A | A | A | A | A | A | A |
| 1/3 Top Left | M | M | M | M | M | M | M | M |
| 1/3 Middle Left | A | A | A | A | A | A | M | M |
| 1/3 Bottom Left | A | A | A | A | A | A | A | A |
Subtitle: S - Yes; N - No; AU - Absent; M - Kept; D - Decreased; A - Incresead.
Table 3 Percussion Evaluation Results
| Digit-digital thoracic percussion - Anterior face of the chest | ||||||||
|---|---|---|---|---|---|---|---|---|
| Date | 14/02/19 | 18/02/19 | 20/02/19 | 21/02/19 | ||||
| Start | End | Start | End | Start | End | Start | End | |
| 1/3 Superior Right | SP | SP | SP | SP | SP | SP | SP | SP |
| 1/3 Middle Right | HO | HO | HO | HO | HO | SP | SP | SP |
| 1/3 Bottom Right | M | M | M | M | M | M | M | M |
| 1/3 Top Left | SP | SP | SP | SP | SP | SP | SP | SP |
| 1/3 Middle Left | HO | HO | HO | HO | HO | HO | HO | SP |
| 1/3 Bottom Left | M | M | M | M | M | M | M | M |
| Digit-digital thoracic percussion - Posterior surface of the chest | ||||||||
| Date | 14/02/19 | 18/02/19 | 20/02/19 | 21/02/19 | ||||
| Start | End | Start | End | Start | End | Start | End | |
| 1/3 Superior Right | SP | SP | SP | SP | SP | SP | SP | SP |
| 1/3 Middle Right | SP | SP | SP | SP | SP | SP | SP | SP |
| 1/3 Bottom Right | HO | HO | HO | HO | HO | HO | HO | HO |
| 1/3 Top Left | SP | SP | SP | SP | SP | SP | SP | SP |
| 1/3 Middle Left | SP | SP | SP | SP | SP | SP | SP | SP |
| 1/3 Bottom Left | HO | HO | HO | HO | HO | HO | HO | HO |
Subtitle: SP - Clear Pulmonary Sound; M - Massive; HO - Hyposonority; HE - Hyperactivity.
Specialized care in respiratory rehabilitation was guided by auscultation performed at the beginning of the intervention and when necessary during the session, providing important data for the dynamics of the nursing intervention statement. Based on the analysis of the data obtained, the almost general decrease in vesicular murmur was evident in the previous auscultation up to the 3rd session. On the posterior face, the best recordings were obtained with a clearly audible vesicular murmur. The crackling rattles, in the inspiratory phase, were the only adventitious sounds present in this study, having been audible bilaterally in the middle and lower thirds. With the performance of promotional exercises for airway cleaning in conjunction with the ability to use expectoratoin techniques, in the fourth session, crackling ferns were found only present in both bases at a lower intensity (Table 7 and 8).
Table 7 Results of the evaluation by previous consultation
| Data | 14/02/19 | 18/02/19 | 20/02/19 | 21/02/19 | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Start | End | Start | End | Start | End | Start | End | ||||||||||||
| Pulmonary Bilaterality | D | E | D | E | D | E | D | E | D | E | D | E | D | E | D | E | |||
| Vesicular murmur | 1/3 Sup | D | D | D | D | D | D | M | M | M | M | M | M | M | M | M | M | ||
| 1/3 Med | D | D | D | D | D | D | M | M | M | M | M | M | M | M | M | M | |||
| 1/3 Inf | A | A | A | A | A | A | D | A | D | D | D | D | D | D | D | D | |||
| Adventitious sounds | 1/3 Sup | ||||||||||||||||||
| 1/3 Med | FC | ||||||||||||||||||
| 1/3 Inf | FC | FC | FC | FC | FC | FC | FC | FC | |||||||||||
Subtitle: M - Kept; D - Decreased; A - Absent; FC - Crackling ferns.
Table 8 Results of posterior auscultation evaluation
| Date | 14/02/19 | 18/02/19 | 20/02/19 | 21/02/19 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Start | End | Start | End | Start | End | Start | End | ||||||||||
| Pulmonary Bilaterality | D | E | D | E | D | E | D | E | D | E | D | E | D | E | D | E | |
| Vesicular murmur | 1/3 Sup | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M |
| 1/3 Med | D | D | M | M | M | M | M | M | M | M | M | M | M | M | M | M | |
| 1/3 Inf | D | D | D | D | D | D | D | D | M | M | M | M | M | M | M | M | |
| Adventitious sounds | 1/3 Sup | ||||||||||||||||
| 1/3 Med | FC | FC | FC | ||||||||||||||
| 1/3 Inf | FC | FC | FC | FC | FC | FC | FC | FC | FC | FC | FC | FC | FC | FC | FC | FC | |
Subtitle: M - Kept; D - Decreased; A - Absent; FC - Crackling ferns.
Vital parameters never conferred limitations or even contraindications to the intervention. From this analysis, regular recording of heart rate (Table 9) should be highlighted, not suggesting exercise intensity conditioning. SpO2 always remained above 95% with the beginning of the rehabilitation sessions, taking into account that weaning from oxygen therapy was performed from session to session. With no worsening of dyspnea after rest, the last session was the only one in which SpO2 was recorded with a supplemental intake lower than at the beginning, reflecting only 1% less (Table 9).
Table 4 Assessment of vital signs and peripheral oxygen oximetry
| Date | 14/02/19 | 18/02/19 | 20/02/19 | 21/02/19 | ||||
|---|---|---|---|---|---|---|---|---|
| Start | End | Start | End | Start | End | Start | End | |
| Blood Pressure (mmHg) | 135/65 | 106/65 | 105/63 | 119/63 | 142/81 | 112/70 | 113/63 | 124/75 |
| Heart Rate (Bpm) | 94 | 80 | 91 | 98 | 96 | 96 | 96 | 95 |
| Respiratory Rate (Cycles/min) | 25 | 20 | 22 | 20 | 19 | 18 | 20 | 18 |
| Temperature (°C) | 36.4 | 36.5 | 35.6 | 36.0 | 37.0 | 36.6 | 36.5 | 36.7 |
| Peripheral Oximetry (%) | 92 | 95 | 95 | 95 | 96 | 98 | 96 | 95 |
Complementary diagnostic tests are essential for the assessment of the individual's respiratory pathology, as well as its evolution.
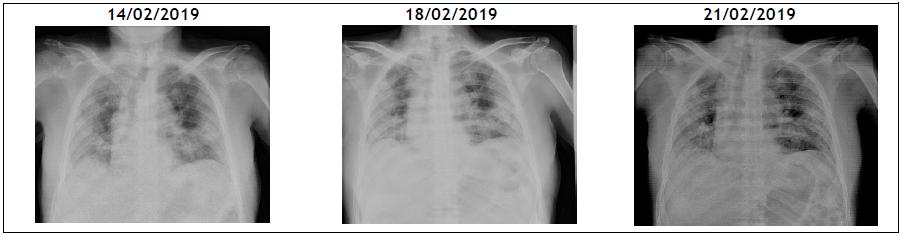
Figure 1 shows the imaging evolution by means of teleradiography of the individual's chest. The three cephalograms present a central image that expresses a global parenchymal infiltrate. The greatest consolidation remained at the level of the pulmonary bases bilaterally. In the last image (2/21/2019), there is a maintained alignment of the diaphragmatic hemicupulas and a slight increase in hypertransparency of both lung fields.
Arterial blood gas reflect the exchange of gases between alveoli and the pulmonary blood stream, being an integral part of the study of respiratory function5.
Table 10 Arterial Blood Gas Results
| Date (2019) | O2 (l/min) | pH | pCO2 (mmHg) | pO2 (mmHg) | Lact (mmol/L) | spO2 (%) | HCO3 (mmol/L) |
|---|---|---|---|---|---|---|---|
| 14/02 | 5 | 7.490 | 39.0 | 52.0 | 1.60 | 85.2 | 29.7 |
| 18/02 | 3 | 7.450 | 47.0 | 55.0 | 1.90 | 90.3 | 34.7 |
| 20/02 | 2 | 7.440 | 39.0 | 52.0 | 1.20 | 89.9 | 26.5 |
| 21/02 | 1 | 7.450 | 41.0 | 65.0 | 1.20 | 94.5 | 28.5 |
By analyzing the values obtained in arterial blood gas, it can be seen that the first 3 sessions are marked by considerable hypoxemia, which had no observable repercussions in the recording of SpO2 or heart rate. These records were obtained in sessions performed with a longer time interval. In the last session there is a general stabilization of parameters within the limits established by the literature and a slight improvement in hypoxemia.
DISCUSSION
The results obtained during the evaluation of the rehabilitation sessions demonstrate that the specialized care of rehabilitation nursing plays an important role in the re-education of the respiratory function of the person with restrictive respiratory pathology, namely bacterial pneumonia.
The approach to the hospitalized person with respiratory pathology is multidisciplinary, involving the medical team, health technicians, operational assistants, and it is only possible for nurses, who maintain direct contact with the person on a daily basis, to carry out systematic monitoring of the health condition and thus establish diagnoses of rehabilitation nursing that allow the most appropriate intervention and in an individualized way, accelerating recovery in situations of acute illness, already demonstrated with level of evidence A by the last update of the ATS/ERS document in 20135.
Respiratory rehabilitation programs include a holistic view of the person receiving care, providing individualized aspects of care that must meet the person's preferences and expectations16. Based on the results obtained, the symptoms associated with the acute episode were minimized, being considered one of the objectives to be achieved with a program of this type5.
The initial assessment with the target person was essential to collect information both subjectively and through physical examination and allowed for the adaptation of interventions following the stage of the disease. This assessment is enriched if complemented by the analysis of complementary means of diagnosis.
The selection of assessment instruments such as the Modified Borg Scale and its ability to directly measure dyspnea by the person at different times allowed for the adaptation of the intensity and frequency of the exercises to the person's condition and expectations; the importance of training with moments of pause and recovery is also highlighted, as well as the evaluation of symptoms after sessions. The implementation of techniques to relieve muscle tension and awareness of respiratory times at an early stage, complemented with exercises to re-educate the respiratory function, showed reductions in the perception of dyspnea felt, ending up with no report of perceived tiredness after rest in the last sessions, with a rating of 0 out of 10 possible on the Modified Borg Scale.
Acting on the dimension of knowledge and on the ability to learn the cough technique enabled the person to perform it independently and more directed to their needs, provided gains in the mobilization and elimination of secretions in the various sessions carried out, ending in the last session only in the presence of dry cough. In addition to this intervention, in a characteristic way.
The program established and defended by the guiding bibliographic evidence based on the opinion of experts5,8-9 showed efficacy in the results obtained in the pathological process, however, it was not equally evident in the monitoring of the body process.
In the physical examination, consisting of four stages, percussion and palpation were not by themselves a record of significant and/or defining changes in the staging of the disease evolution process. The benefits recorded focused on inspection for improved breathing pattern, being more regular with respiratory rates between 12 and 20 cycles/min, relaxation of accessory muscles of breathing and auscultation of the posterior phase of the thorax, with a overall increase in vesicular murmur and an absence of the sizzling ferns felt in the bilateral middle third. At the last assessment, these adventitious sounds were still present in the lung bases, although at a lower intensity, which coincided with the best ability to cough.
Together with the exercise program for diaphragmatic and costal re-education, the techniques performed at the level of rest, postural correction and associated thoracic mobilizations allowed for better tolerance to exertion and reduced oxygen supply. The SpO2 evaluation method, non-invasive and easy to apply using a portable oximeter, allowed this evaluation to be carried out continuously with the necessary safety for the person. It was possible to verify that the possibility of allowing visual contact of the SpO2 result obtained during the exercises worked as a positive stimulus for their motivation.
Incentive spirometry was important not only in the training of respiratory muscles8 but also in the motivation and commitment to complying with the sessions due to its ability to establish visual goals to be achieved. Its use may occur before the session and after the rest, with improved results in this second evaluation compared to the first.
Chest radiography confirmed pulmonary involvement, as well as the location and extent of lobar consolidation8. The appearance of hypertransparency was slightly evident on the last day, not following the evolution presented by data such as SpO2, Modified Borg Scale monitoring, pulmonary auscultation and the reduction in sputum upon coughing. However, the imaging changes may not immediately translate current changes8.
This case study reflects the importance of the RN in developing and improving its respiratory function assessment techniques in order to carry out a systematic assessment, if necessary, readjust its intervention based on the data obtained.
In this research, it would have been beneficial to carry out sessions with a shorter time interval, because a greater evolution between the 20th and 21st of February. According to gasometric values obtained, the reversion of the marked hypoxemia occurred only in this period and was not limited by the reduction of oxygen supply, which was initially at a rate of 5L/min and which at the end of the program was administered at 1L/min. This situation is not in line with what Cordeiro & Menoita defend in their bibliography, when state that the people as the target of this study, that is, without previous respiratory pathology, in a situation of bacterial pneumonia, regular arterial blood gas analysis is not justified, except in low SpO28.
It is relatively frequent that people with Influenza A who are overinfected with bacterial pneumonia develop severe hypoxemia conditions difficult to reverse. In this case study, both focuses were addressed with the appropriate interventions directed towards their resolution, supported by the most updated bibliography. The lack of other similar studies did not make it possible to establish a comparison of the increase in pO2 associated with a respiratory rehabilitation intervention plan.
FINAL THOUGHTS
This case study highlighted the benefits of the respiratory function, in the ventilation and expectoration focuses, resulting from the specialized intervention of the specialist nurse in rehabilitation nursing.
In respiratory functional reeducation, it is essential to perform a subjective assessment of respiratory function, complemented by physical examination and complementary diagnostic data, such as chest teleradiography and gasimetric data. It results in a set of data that allow the rehabilitation nurse to analyze the information obtained, identify problems and plan the respective interventions, supported by reliable and valid instruments.
Thus, the gains obtained by the functional respiratory reeducation centered on the perception of dyspnea by the Modified Borg Scale, with a reduction from 2 to 0; on breathing pattern with absence of recruitment to accessory muscles, decrease in respiratory cycles per minute accompanied by a more regular pattern with diaphragmatic excursion; on auscultation, essentially of the posterior thorax, with an overall increase in vesicular murmur and reduction in crackling sounds; on chest X-ray with the appearance, although slight but progressive, of hypertransparency in both lung fields; in cough, with training to use directed cough, ending the sessions with an essentially dry cough; in gasimetric results showing the beginning of reversal of hypoxemia in the last session; in the weaning from the supplemental oxygen supply, starting with 5L/min and ending with 1L/min.
To obtain the abovementioned gains, it was essential to use specialized techniques directed to the different focuses, including the ventilation focus: interventions such as the resting position, massage of accessory muscles, control and dissociation of respiratory times, expiration with semi-closed lips, rotation of the humeral scapula, global opening with a stick, bilateral lower costal and abdominodiaphragmatic re-education, thoracic mobilization exercises and incentive spirometry. In the spectorate focus, techniques such as accessory maneuvers (vibration, percussion and compression), assisted/directed coughing, huffing and the forced expiration technique are evidenced, supported by the previous use of nebulizers with saline solution.
Based on the epidemiological data obtained, bacterial pneumonia as a possibility of secondary infection resulting from Influenza A is an increasingly growing fact. It is hoped that this case will contribute to giving visibility to the importance that rehabilitation nursing can have in reducing the comorbidities resulting from these episodes. It would be beneficial to develop more studies on this pathology, which despite being characteristically restrictive, suffers from seasonal influence.
It is suggested in future studies the possibility of performing earlier and more regular sessions (or even preferably daily) in order to contribute to a better clarification of the importance that the intervention of respiratory functional reeducation by RN can obtain in sustained severe hypoxemia and thus reduce the length of hospital stay, culminating in an increased level of evidence. Intervention plans with greater emphasis on aerobic exercises using cycle ergometers and thoracic mobilizations are also suggested, allowing the ventilation-perfusion index. In some cases, intervention plans of shorter duration and/or divided into two daily moments will be considered.
REFERÊNCIAS
1 Administração Regional de Saúde Lisboa e Vale do Tejo, I.P. Plano De Contingência Saúde Sazonal. Portugal: Autor; 2018.(Consultado a 20/02/2019) Disponível em: http://www.arslvt.min-saude.pt/uploads/writer_file/document/6505/ARSLVT_Saude_Sazonal_Modulo_Inverno_2018_2019.pdf [ Links ]
2 Kislaya I, Machado A, Gomez V, Mexia R. Utilização dos cuidados de saúde na presença de síndrome gripal: descrição das épocas 2011/2012 a 2016/2017. [ Links ]
3 Instituto Nacional de Saúde Doutor Ricardo Jorge I.P.. Boletim de Vigilância Epidemiológica da Gripe: Semana 4. Portugal: Autor; 2019. (Consultado a 20/02/2019); Disponivel em: http://www.insa.min-saude.pt/wp-content/uploads/2019/02/S04_2019.pdf [ Links ]
4 Fonseca S, Barbosa A, Melnikova Z, Silva C, Silva S, Alves V, Barreto JV. Pneumonias Pneumocócicas e Pneumonias por Influenza A: Estudo Comparativo. Medicina Interna. 2017 Jun;24(2):106-11. [ Links ]
5 Ordem dos Enfermeiros-Conselho de Enfermagem e Mesa do Colégio de Enfermagem de Reabilitação. Guia Orientador de Boa Prática: Reabilitação Respiratória. Lisboa: Autor. 2018. Consultado a 20/01/2019. Disponível em: https://www.ordemenfermeiros.pt/media/5441/gobp_reabilita%C3%A7%C3%A3o-respirat%C3%B3ria_mceer_final-para-divulga%C3%A7%C3%A3o-site.pdf [ Links ]
6 Santos A. 13º Relatório do Observatório Nacional das Doenças Respiratórias: Panorama das doenças respiratórias em Portugal 2018. Portugal: ONDR; 2018 (Consultado a 10/01/2019) Disponível em: https://www.ondr.pt/relatorios_ondr.html [ Links ]
7 Assunção RG, Pereira WA, Abreu AG. Pneumonia bacteriana: aspectos epidemiológicos, fisiopatologia e avanços no diagnóstico. Rev Inv Biomédica. 2018 Jul 31;10(1):83-91 [ Links ]
8 Cordeiro M; Menoita E. Manual de Boas Práticas na Reabilitação Respiratória: Conceitos, Princípios e Técnicas. Loures: Lusociência. 2012. [ Links ]
9 Ferreira D, Santos A. Avaliação da Pessoa com Patologia Respiratória. In C. Marques-Vieira; L. Sousa (Eds). Cuidados de Enfermagem de Reabilitação à Pessoa ao Longo da Vida. Loures: Lusodidata. 2017:167 - 180 [ Links ]
10 Ordem dos Enfermeiros. Regulamento das competências comuns do enfermeiro especialista. Lisboa: Autor; 2010. (Consultado a 21/2/2019). Disponível em https://www.ordemenfermeiros.pt/arquivo/legislacao/Documents/LegislacaoOE/RegulamentoCompetenciasReabilitacao_aprovadoAG20Nov2010.pdf [ Links ]
11 Gomes B, Ferreira D. Reeducação da Função Respiratória. In C. Marques-Vieira; L. Sousa (Eds). Cuidados de Enfermagem de Reabilitação à Pessoa ao Longo da Vida. Loures: Lusodidata. 2017: 253 - 262 [ Links ]
12 Rodrigues C, Martins V, Munhá J, Branco C. Programa Nacional para as Doenças Respiratórias: Relatório de Análise da Capacidade Instalada de Reabilitação Respiratória nos Hospitais do Serviço Nacional de Saúde. Portugal: Direção Geral de Saúde. 2015. [ Links ]
Andrade SR, Ruoff AB, Piccoli T, Schmitt MD, Ferreira A, Xavier AC. O estudo de caso como método de pesquisa em enfermagem: uma revisão integrativa. Texto & Contexto-Enferm. 2017;26(4). [ Links ]
14 Nunes L. Considerações éticas: a atender nos trabalhos de investigação académica de enfermagem. Setúbal: Departamento de Enfermagem ESS; 2013. (Consultado a 20/02/2019). Disponível em: https://comum.rcaap.pt/bitstream/10400.26/4547/1/consid%20eticas%20na%20investig%20academica%20em%20enfermagem.pdf [ Links ]
15 Assembleia do Colégio da Especialidade de Enfermagem de Reabilitação. Padrão Documental dos Cuidados de Enfermagem da Especialidade de Enfermagem de Reabilitação. Lisboa: Ordem dos Enfermeiros. 2014. (Consultado a 20/02/2019). Disponível em: https://www.ordemenfermeiros.pt/arquivo/colegios/Documents/2015/MCEER_Assembleia/PadraoDocumental_EER.pdf [ Links ]
16 Pereira, R. Enfermagem Baseada na Evidência: Um desafio, Uma Oportunidade. In C. Marques-Vieira; L. Sousa (Eds). Cuidados de Enfermagem de Reabilitação à Pessoa ao Longo da Vida. Loures: Lusodidata. 2017:101 - 111 [ Links ]
Received: July 05, 2019; Accepted: November 22, 2019











 text in
text in