Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Portuguesa de Enfermagem de Reabilitação
Print version ISSN 2184-965XOn-line version ISSN 2184-3023
RPER vol.6 no.1 Silvalde June 2023 Epub June 30, 2023
https://doi.org/10.33194/rper.2023.264
Literature review
Dysphagia screening tools after prolonged intubation: a systematic review of the literature
1Escola Superior De Saúde Norte Da Cruz Vermelha Portuguesa, Oliveira de Azeméis, Portugal
2Centro Hospitalar do Porto, Porto, Portugal
Introduction:
Post-extubation dysphagia affects a significant percentage of patients. However, its screening is not systematically performed, contributing to low awareness of the problem and predisposing to complications. The systematization of the approach to these patients begins with the use of reliable and sensitive screening tools.
Methodology:
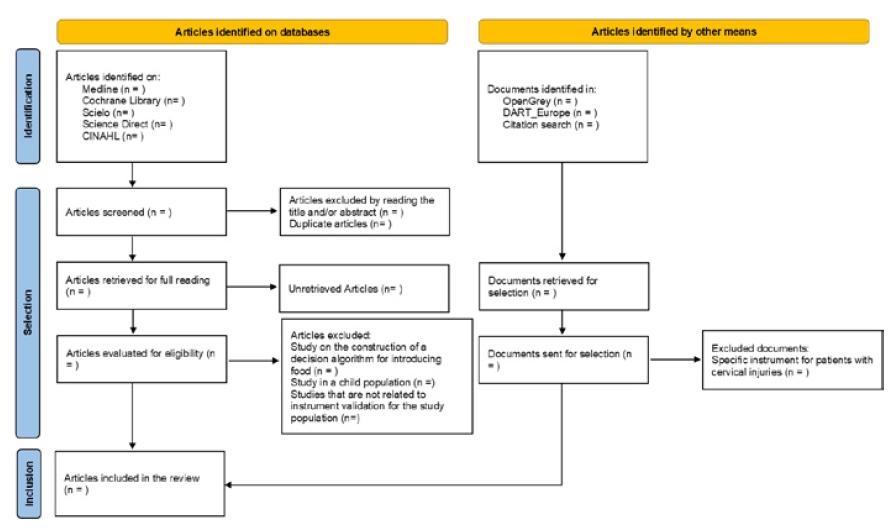
Systematic literature review guided by the principles of the Cochrane Screening and Diagnostic Test Methods Group and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses. The Medline, Cochrane Library, Scielo, Science Direct and CINAHL databases were consulted. Additionally, a gray literature search was performed. Inclusion criteria included validation studies of screening instruments for patients after prolonged intubation (more than 48 hours).
Results:
7,043 articles were reviewed of which seven were selected for full reading, and only one met the inclusion criteria.
Discussion:
There are several validated dysphagia screening instruments for other clinical populations, but only one was identified for this specific population. The instrument has good inter-rater reliability, however, a sensitivity of 81%, means that part of these patients will not be identified as dysphagic, which will have negative repercussions. This instrument was validated against clinical evaluation, which is a limitation to the interpretation of its results.
Conclusion:
There is no Portuguese version of this instrument, which hinders the development of guidelines that systematize the therapeutic approach for patients after extubation. We advocate its translation and validation for the national context and validation with a reference test.
DESCRIPTORS: Deglutition disorders; critical care; screening; intratracheal intubation; nursing care; rehabilitation nursing
Introdução:
A disfagia pós-extubação afeta uma percentagem significativa de doentes. Contudo o seu rastreio não é realizado de forma sistemática, contribuindo para uma reduzida perceção do problema e predispondo à ocorrência de complicações.
Metodologia:
Revisão Sistemática da Literatura orientada pelos princípios da Cochrane Screening and Diagnostic Test Methods Group e o Preferred Reporting Items for Systematic Reviews and Meta-Analyses, com o objetivo de identificar os instrumentos de rastreio da disfagia em doentes pós-extubação. Consultadas as bases de dados Medline, Cochrane Library, Scielo, Science Direct e CINAHL e efetuada pesquisa na literatura cinzenta. Como critérios de inclusão foram definidos estudos de validação de instrumentos de rastreio para doentes pós-extubação de intubação prolongada (superior a 48 horas).
Resultados:
Revistos 7043 artigos dos quais foram selecionados sete para leitura integral, sendo que apenas um cumpria os critérios de inclusão.
Discussão:
Apenas um instrumento de rastreio de disfagia validado foi identificado para esta população específica. O instrumento apresenta boa fiabilidade entre observadores, no entanto, a sensibilidade, sendo de 81%, significa que parte destes doentes não será identificado como disfágico, o que terá repercussões negativas. Este instrumento foi validado contra avaliação clínica, o que se mostra uma limitação à interpretação dos seus resultados.
Conclusão:
Não existe versão em português deste instrumento, o que dificulta a elaboração de orientações que sistematizem a abordagem terapêutica para doentes pós-extubação. Advoga-se a sua tradução e validação para o contexto nacional e validação com teste de referência.
DESCRITORES: Transtornos de deglutição; cuidados críticos; screening; intubação intratraqueal; cuidados de enfermagem; enfermagem em reabilitação
Introducción:
La disfagia postextubación afecta a un porcentaje importante de pacientes. Sin embargo, no se realiza un cribado sistemático, lo que contribuye a una escasa concienciación del problema y predispone a las complicaciones. La sistematización del abordaje de estos pacientes comienza con el uso de herramientas de cribado fiables y sensibles.
Metodología:
Revisión sistemática de la literatura guiada por los principios del Cochrane Screening and Diagnostic Test Methods Group y Preferred Reporting Items for Systematic Reviews and Meta-Analyses. Se consultaron las bases de datos Medline, Cochrane Library, Scielo, Science Direct y CINAHL. Además, se realizó una búsqueda en la literatura gris. Los criterios de inclusión se definieron como estudios de validación de instrumentos de cribado para pacientes tras una intubación prolongada (más de 48 horas).
Resultados:
Se revisaron 7043 artículos, de los cuales se seleccionaron siete para su lectura completa, y sólo uno cumplió los criterios de inclusión.
Discusión:
Sólo se ha identificado un instrumento para esta población específica, que muestra una buena fiabilidad interobservador. Sin embargo, la sensibilidad, al ser del 81%, significa que parte de estos pacientes no serán identificados como disfágicos, lo que tendrá repercusiones negativas. Este instrumento fue validado con una evaluación clínica, lo que muestra una limitación en la interpretación de sus resultados.
Conclusión:
No existe una versión en portugués de este instrumento, lo que dificulta la elaboración de orientaciones que sistematicen el abordaje terapéutico para estes pacientes. Abogamos por su traducción y validación con una prueba de referencia en el contexto nacional.
DESCRIPTORES: Trastornos de deglución; cuidados intensivos; cribado; intubación intratraqueal; atención de enfermería; enfermería en rehabilitación
INTRODUCTION
The need for invasive mechanical ventilation (IMV) is one of the main reasons for admission to intensive care units (ICU), and therefore it is necessary to establish an artificial airway, through endotracheal intubation. In 2017, in the United States of America, 903,745 patients were discharged from hospital after admission due to respiratory failure and need for IMV 1. More recently, the pandemic context has led to an increase in the number of patients in need of ICU admission and this type of support. Furthermore, recent data from ICNARC 2 (Intensive Care National Audit & Research Centre, 2022), in the United Kingdom, indicate that 30.7% of patients admitted to intensive care due to COVID-19 (Coronavirus Disease 2019), required IMV in the first 24 hours, which was maintained for an average of 13 days.
The development of swallowing disorders can occur after removal of the endotracheal tube, a phenomenon known as post-extubation dysphagia, which, due to its consequences can cause, namely aspiration, and is a cause for concern in intensive care units/services. The incidence of this problem varies according to the patient populations studied and the screening methods used. However, a recent meta-analysis states that it affects 41% of patients after extubation, also verifying that a significant percentage of these patients have silent aspiration 3. There is also a correlation between the duration of IMV and the occurrence of post-extubation dysphagia 4, suggesting other risk factors, such as increasing age, altered vocal quality and the degree of voice impairment 5. This condition can persist until hospital discharge, constituting an independent predictor of death 6 and even last for long periods after discharge, with recovery in some cases extending up to five years 7.
Since swallowing is a complex phenomenon, which involves the synchronous functioning of a large number of muscles and cranial nerves, some mechanisms that are at the origin of dysphagia are known and are directly related to an underlying pathology (for example, stroke). However, the etiology of post-extubation dysphagia is multifactorial and still partially understood, with potential mechanisms for its development being pointed out as: oropharyngeal or laryngeal trauma, intensive care unit acquired weakness , decreased laryngeal sensation, altered consciousness due to delirium or sedation, gastroesophageal reflux and lack of coordination between breathing and swallowing 8, which may explain the relative difficulty in perceiving the problem and screening.
Post-extubation dysphagia increases the risk of aspiration and development of pneumonia, delay in nutritional recovery, malnutrition, decreased quality of life, prolonged length of stay in intensive care and hospital, increased morbidity and mortality, also having a significant economic impact on health systems 9. Despite the potential consequences and the acknowledgment that this is a significant and frequent problem, dysphagia is not regularly screened in the context of intensive care, and the absence of diagnostic, treatment and rehabilitation protocols is also frequent 10. Thus, as validated international recommendations are not known, the need for the adoption in clinical contexts of instruments that allow the effective dysphagia screening and the referral of identified patients for differentiated intervention is evident, thus avoiding the development of complications that negatively affect prognosis.
Since the nurse is the professional who spends the most time with the patient and is also responsible for managing the reintroduction of oral feeding, it is important that validated instruments are made available for screening and initial assessment, in order to contribute to the decision-making process on the interventions to be implemented and the referral to the specialist nurse in rehabilitation nursing to initiate specialized interventions.
In this context, a systematic literature review was carried out with the aim of identifying dysphagia screening instruments in post-extubation patients who had been submitted to IMV for a period longer than 48 hours.
METHODOLOGY
In response to the objective of this study, a systematic review of the literature was carried out guided by the principles of the Cochrane Screening and Diagnostic Test Methods Group 11 and in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 12. The research strategy was designed by two reviewers and followed the key concepts defined by the following PICO model 13: post-extubation patients who have been submitted to IMV for a period greater than 48 hours (Population); dysphagia screening instruments (Intervention); clinical and/or instrumental evaluation by swallowing videofluoroscopy or swallowing fibroendoscopy (Comparator); and dysphagia and/or aspiration (outcome). All methodological studies of validation of health measurement instruments, published in the last 10 years and with no publication language limit, were eligible for inclusion in this review. The definition of the time limit for the inclusion of articles was based on the argument of the intention to perform a review of recently published evidence.
The search was conducted between January and April 2022 in the following databases: Medline (via Pubmed), the Cochrane Library, Scielo, Science Direct and CINAHL (via EbscoHost). Additionally, bibliographical references of the most relevant articles retrieved were manually searched and gray literature was searched in OpenGrey and DART-Europe. For the management of references, the Mendeley Reference Manager, version 2.66.0, was used.
Table 1 presents the search strategy for each of the databases.
Table 1 Search strategy
| Database | Results | |
|---|---|---|
| Medline (via PubMed) - searched on February 7th, 2022 | ||
| #1 | ,"((((((""critical care"") OR (""intensive care"")) OR (""artificial respiration"")) OR (ventilation)) OR (""mechanical ventilation"")) OR (weaning)) OR (post-extubation)",,,"""critical care""[All Fields] OR ""intensive care""[All Fields] OR ""artificial respiration""[All Fields] OR (""ventilated""[All Fields] OR ""ventilates""[All Fields] OR ""ventilating""[All Fields] OR ""ventilation""[MeSH Terms] OR ""ventilation""[All Fields] OR ""ventilate""[All Fields] OR ""ventilations""[All Fields] OR ""ventilator s""[All Fields] OR ""ventilators, mechanical""[MeSH Terms] OR (""ventilators""[All Fields] AND ""mechanical""[All Fields]) OR ""mechanical ventilators""[All Fields] OR ""ventilator""[All Fields] OR ""ventilators""[All Fields] OR ""ventilation""[All Fields]) OR ""mechanical ventilation""[All Fields] OR (""weaning""[MeSH Terms] OR ""weaning""[All Fields] OR ""weaned""[All Fields] OR ""weaning""[All Fields] OR ""weans""[All Fields]) OR ""post-extubation""[All Fields]" | 655 219 |
| #2 | ,"((((screen*) OR (sensitivity)) OR (""predictive values"")) OR (validity)) OR (reliability)",,,"""screen*""[All Fields] OR (""hypersensitivity""[MeSH Terms] OR ""hypersensitivity""[All Fields] OR ""sensitive""[All Fields] OR ""sensitively""[All Fields] OR ""sensitives""[All Fields] OR ""sensitivities""[All Fields] OR ""sensitivity and specificity""[MeSH Terms] OR (""sensitivity""[All Fields] AND ""specificity""[All Fields]) OR ""sensitivity and specificity""[All Fields] OR ""sensitivity""[All Fields]) OR ""predictive values""[All Fields] OR (""valid""[All Fields] OR ""validate""[All Fields] OR ""validated""[All Fields] OR ""validates""[All Fields] OR ""validating""[All Fields] OR ""validation""[All Fields] OR ""validation""[All Fields] OR ""validations""[All Fields] OR ""validator""[All Fields] OR ""validators""[All Fields] OR ""validities""[All Fields] OR ""validity""[All Fields]) OR (""reliabilities""[All Fields] OR ""reliability""[All Fields] OR ""reliable""[All Fields] OR ""reliability""[All Fields] OR ""reliably""[All Fields])" | 4 226 804 |
| #3 | "(((dysphagia) OR (""deglutition disorders"")) OR (swallow*)) OR (aspiration)",,,"""deglutition disorders""[MeSH Terms] OR (""deglutition""[All Fields] AND ""disorders""[All Fields]) OR ""deglutition disorders""[All Fields] OR ""dysphagia""[All Fields] OR ""dysphagia""[All Fields] OR ""deglutition disorders""[All Fields] OR ""swallow*""[All Fields] OR (""aspirant""[All Fields] OR ""aspirants""[All Fields] OR ""aspirate""[All Fields] OR ""aspirated""[All Fields] OR ""aspirates""[All Fields] OR ""aspirating""[All Fields] OR ""aspiration""[All Fields] OR ""aspirational""[All Fields] OR ""aspirations, psychological""[MeSH Terms] OR (""aspirations""[All Fields] AND ""psychological""[All Fields]) OR ""psychological aspirations""[All Fields] OR ""aspirations""[All Fields] OR ""aspirative""[All Fields] OR ""aspirator""[All Fields] OR ""aspirators""[All Fields] OR ""aspire""[All Fields] OR ""aspired""[All Fields] OR ""aspires""[All Fields] OR ""aspiring""[All Fields])" | 217 281 |
| #4 | 1# AND #2 AND #3 Filters: adults and publication date since January 1st, 2012 | 433 |
| Cochrane Library - searched on April 11th, 2022 | ||
| #1 | (critical care):ti,ab,kw OR (intensive care):ti,ab,kw OR (artificial ventilation):ti,ab,kw OR (ventilation):ti,ab,kw OR (mechanical ventilation):ti,ab,kw (Word variations have been searched) | 75165 |
| #2 | (screen*):ti,ab,kw OR (sensitivity):ti,ab,kw OR (predictive values):ti,ab,kw OR (validity):ti,ab,kw OR (reliability):ti,ab,kw (Word variations have been searched) | 240788 |
| #3 | (dysphagia):ti,ab,kw OR (swallowing disorders):ti,ab,kw OR (aspiration):ti,ab,kw OR (swallowing):ti,ab,kw (Word variations have been searched) | 19527 |
| 4# | 1# AND #2 AND #3 No filters | 341 |
| Scielo - searched on March 14th, 2022 | ||
| #1 | (dysphagia OR "swallowing disorders" OR aspiration OR swallowing) AND ("intensive care") OR ("critical care") | 595 |
| Science Direct - pesquisada a 21 de março de 2022 | ||
| #1 | dysphasia OR "deglutition disorders" OR aspiration OR swallow AND "critical cares" OR "intensive care" AND "mechanical ventilation" OR "post-extubation" | 5537 |
| CINAHL (via EbscoHost) - pesquisada a 7 de fevereiro de 2022 | ||
| (dysphagia OR "deglutition disorders" OR aspiration OR swallow* AND "critical care" OR "intensive care" AND "mechanical ventilation" OR weaning OR "post-extubation") AND (sensitivity OR screen* OR "predictive value") | 137 | |
| DART-Europe - pesquisada a 7 de março de 2022 | ||
| #1 | dysphagia AND ("intensive care" OR "critical care") No filters | 3 |
| OpenGrey - searched on March 23, 2022 | ||
| #1 | Dysphagia No filters | 4 |
All identified articles were initially assessed for relevance according to title and abstract by two independent reviewers. Whenever the information contained in the abstract was not sufficient to assess compliance with the inclusion criteria, full articles were retrieved for reading. The selected articles were then assessed for their methodological quality by two independent reviewers, using the QUADAS 2 instrument 14. This instrument assesses methodological quality in four domains: patient selection, instrument used, reference test, and flow and time. The cut-off point for the inclusion of a study was the “low risk” response in at least five of the seven items contained in the assessment instrument. Disagreements between reviewers were resolved by consulting a third reviewer.
Data were extracted by two independent reviewers into an a priori defined data extraction table, prepared according to the review objectives, including information on the main characteristics of the participants, screening instrument to be validated and its description, reference test applied and main results (sensitivity, specificity and reliability). Disagreements between reviewers in data extraction were resolved using a third reviewer. The results are presented in a narrative synthesis format.
RESULTS
A total of 7,043 articles were reviewed by title and/or abstract, and of these, seven were reviewed by full reading, of which one met the inclusion criteria. The process of identification, selection and inclusion of articles is systematized in Figure 1. The article that met the inclusion criteria was subjected to a methodological quality assessment, having obtained a total of 5 items evaluated as low risk and two items evaluated as uncertain 14.
The data related to the articles included for review and extracted are presented in table 2.
DISCUSSION
Post-extubation dysphagia is frequent in ventilated critically ill patients 3 and, although the mechanisms underlying its development are not yet fully understood 9, it is known to result in poorer quality of life, increased length of hospital stay and of mortality at 28 and 90 days6,8. The systematic screening and
Table 2 Data extraction table with results
| Author | Participants | Screening tool | Reference test | Results |
|---|---|---|---|---|
| Johnson et al., 2018 15 | 66 patients from 4 medical-surgical intensive care units | Test composed of 5 parts, resulting in the assessment of the risk of dysphagia, and the affirmative answer to any of the questions in each of these parts implies the interruption of the test and maintenance of the patient on a zero diet. The first part refers to the existence of a previous assessment by a speech therapist; the second part to the state of consciousness; the third related to respiratory status; the fourth part on clinical data and the existence of pre-existing nasogastric intubation or gastrostomy and the fifth part on verification of the diet prescription by the physician. | Clinical assessment including physical examination, cognitive assessment, and examination of oral motricity and oral and pharyngeal muscle function. Assessment carried out by a speech therapist within 16 hours of applying the screening instrument. | Inter-observer reliability k=0.92 Sensitivity 81% and specificity 69% Positive predictive value 77% and negative predictive value 74% |
early diagnosis of dysphagia in other clinical populations reduces the incidence of pneumonia 16, which suggests that systematic screening is beneficial and therefore should also be performed in these patients 9. However, the existence of guidelines or clinical recommendations formally issued by competent bodies regarding the need and best strategy for screening post-extubation dysphagia is unknown.
In fact, the literature review suggests that this is not yet a focus of attention at the research level, and the results of a study carried out in 26 countries suggest that it is not yet a focus of attention in practice 17. This study reveals that 67% of the ICUs do not have implemented protocols for dysphagia screening, 70% do not systematically assess post-extubation swallowing for patients intubated for more than 48 hours, about 46% use water tests to assess aspiration and only 8% resort to instrumental assessment. The instrumental evaluation is considered the gold standard in the evaluation of dysphagia and, more specifically, in the identification of aspiration 18. Considering the high prevalence of post-extubation dysphagia and the prevalence of silent aspiration in these patients 3, it is expected that, as seen in other clinical populations, it increases the risk of developing complications, both respiratory and nutritional, with serious repercussions in the rehabilitation process and placing a greater economic burden on health systems 19.
This context alerts to another relevant issue related to the results of this review. For this specific clinical population, the results indicate the existence of only one validated instrument 15, although there is evidence of the use of instruments validated with other clinical populations 8 in the screening of dysphagia in ICU patients. The validation of this instrument was carried out using clinical evaluation as a reference test, and there is evidence of reduced sensitivity for the identification of dysphagia when clinical evaluation is used as a reference 20. It follows that the results regarding the sensitivity and specificity of this instrument should be interpreted with reservations. Ideally, all screening instruments should have 100% sensitivity and specificity 21. This is the only way to ensure that all dysphagic and non-dysphagic patients are correctly identified. The results obtained for this instrument reveal that part of the patients will not be correctly identified as dysphagic in the screening (19%). This aspect is particularly important given that the inadequate identification of dysphagic patients has serious immediate repercussions, such as respiratory complications 9. Another dysphagia screening instrument was identified for this specific clinical population 22. One of the authors of this instrument was contacted, since the literature review did not show results from its validation, and information was provided that the validation process is still ongoing, so it is not possible to compare the results.
Furthermore, only the psychometric properties of the instrument were made available, resulting in dysphagia. Results for aspiration screening are not available, thus not allowing to determine the validity of screening. These are the main limitations identified in this instrument. It should be noted, however, the excellent inter-rater reliability , which guarantees that similar results will be obtained when using the instrument, when used under similar conditions by different professionals 23.
Regarding the national context, no Portuguese version of this instrument or any other developed with prolonged post-extubation patients as a target population was identified. It follows that there is no instrument available for the Portuguese population to screen for dysphagia, which creates an obstacle for the first step in the systematization of the therapeutic approach to the patient with dysphagia 24. The availability of validated instruments becomes essential for the early screening of dysphagia by general care nurses, regardless of the context in which it occurs 25, for subsequent referral to the specialist nurse in rehabilitation nursing for clinical evaluation and early intervention 26, thus ensuring better functional results.
CONCLUSION
Post-extubation dysphagia in patients hospitalized in intensive care has a significant expression, so early screening is essential. This systematic review identified only one screening instrument developed specifically for this patient population. Although this instrument has good reliability among observers, some patients will not be identified as having dysphagia, given its sensitivity of 81%, thus predisposing to the occurrence of complications, with significant repercussions on the rehabilitation process. It should also be noted that the results obtained in terms of sensitivity and specificity were obtained through clinical evaluation and not through instrumental evaluation, which raises some reservations regarding their interpretation.
Since the factors that can potentially lead to post-extubation dysphagia are different from other patient populations, for which screening instruments have already been validated, this instrument presents criteria that are relevant and specific for the evaluation of extubated patients after prolonged endotracheal intubation, allowing thus a more adequate screening to the characteristics of the patients to which it is applied. However, no translation and validation for the national context was found, which makes it difficult to implement strategies for a systematic approach to the problem.
This review has limitations, namely the existence of only one instrument, which prevents comparability of results and assessment of instrument results. In addition, despite having sought to cover a wide range of databases for research and gray literature, systematic reviews tend to selection bias.
It is recommended to carry out translation and validation studies of this instrument for the Portuguese population, with a more significant sample and its validation using instrumental evaluation, which can support a systematic approach, promoting referral for diagnostic evaluation and initiation of interventions of rehabilitation.
REFERENCES
1 Kempker JA, Abril MK, Chen Y, Kramer MR, Waller LA, Martin GS. The epidemiology of respiratory failure in the United States 2002-2017: A serial cross-sectional study. Crit care Expl [Internet]. 2020 [cited 2022 May 3]; 2:e0128. Disponível em: https://doi.org/10.1097/CCE.0000000000000128 [ Links ]
2 Intensive Care National Audit Research Centre. ICNARC report on COVID-19 in critical care: England, Wales and Northern Ireland 8 april 2022 [Internet]. London: Intensive Care National Audit Research Centre, 2022 [cited 2022 May 3]. Disponível em: https://www.icnarc.org/DataServices/Attachments/Download/d7890b82-5fb7-ec11-913d-00505601089b [ Links ]
3 McIntre M, Doeltgen S, Dalton N, Koppa M, Chimunda T. Pos-extubation dysphagia incidence in critically ill patients: A systematic review and meta-analysis. Aust Crit Care [Internet]. 2021[cited 2022 May 2]; 34(1): 67-75. Disponível em: https://doi.org/10.101016/j.aucc.2020.05.008 [ Links ]
4 Laguna LB, Marcos-Neira P, Zurbano IM, Marco EM, Guisasola CP, Soria CD, Martí PR. Dysphagia and mechanical ventilation in SARS-COV-2 pneumonia: It’s real. Clin Nutr [Internet]. 2021[cited 2022 May 3]; 23:S0261-5614(21)00527-6. Disponivel em https://doi.org/10.1016/j.clnu.2021.11.018 [ Links ]
5 Oliveira AC, Friche AA, Salomão MS, Bougo GC, Vicente LC. Predictive factos for oropharyngeal dysphagia after prolonged orotracheal intubation. Braz J Otorhinolaryngol [Internet]. 2018[cited 2022 May 4]; 84:722-8. Disponivel em: https://doi.org/10.1016/j.bjorl.2017.08.010 [ Links ]
6 Schefold JC, Berger D, Zürcher P, Lensch M, Perren A, Jakob S, et al. Dysphagia in mechanically ventilated ICU patients /DYnAMICS): A prospective observational trial. Crit Care Med [Internet].2017[cited 2022 May 3]; 45(12):2061-2069. Disponivel em: https://doi.org/10.1097/CCM.0000000000002765 [ Links ]
7 Brodsky MB, Huang M, Shanholtz C, Mendez-Tellez PA, Palmer JB, Colantuoni E, Needham DM. Recovery from dysphagia symptoms after oral endotracheal intubation in acute respiratory distress syndrome survivors a 5-year longitudinal study. Ann Am Thorac Soc [Internet].2017[cited 2022 May 3]; 14(3): 376-383. Disponivel em: https://doi.org/10.1513/AnnalsATS.201606-455OC [ Links ]
8 Perren A, Zürcher P, Schefold JC. Clinical approaches to assess post-extubation dysphagia (PED) in the critically ill. Dysphagia [Internet]. 2019[cited 2022 May 3]; 34(4):475-486. Disponivel em: https://doi.org/10.1007/s00455-019-09977-w [ Links ]
9 Zuercker P, Moret CS, Dziewas R, Schefold JC. Dysphagia in the intensive care unit: epidemiology, mechanisms, and clinical management. Critical Care [Internet]. 2019[cited 2022 May 5]; 23:103. Disponivel em: https://doi.org/10.1186/s13054-019-2400-2 [ Links ]
10 van Snippenburg W, Kröner A, Flim M, Hofhuis J, Buise M, Hemler R et al. Awareness and management of dysphagia in Dutch intensive care units: A nationwide survey. Dysphagia [Internet]. 2019[cited 2022 May 5]; 34(2):220-228. Disponivel em: https://doi.org/10.1007/s00455-018-9930-7 [ Links ]
11 Deeks JJ, Bossuyt PM, Gatsonis C (editors), Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy Version 1.0.0. [Internet]. The Cochrane Collaboration, 2013[cited 2022 April 28]. Disponível em: http://srdta.cochrane.org/ [ Links ]
12 Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ [Internet]. 2021[cited 2022 April 20]; 372:n71. Disponivel em: https://doi.org/10.1136/bmj.n71 [ Links ]
13 Considine J, Shaban RZ, Fry M, Curtis K. Evidence based emergency nursing: Designing a research question and searching the literature. Int Emerg Nurs [Internet]. 2017[cited 2022 April 15]; 32:78-82. Disponivel em: https://doi.org/10.1016/j.ienj.2017.02.001 [ Links ]
14 Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM; QUADAS-2 Group. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med [Internet]. 2011[cited 2022 April 30]; 155(8):529-36. Disponivel em: https://doi.org/10.7326/0003-4819-155-8-201110180-00009 [ Links ]
15 Johnson KL, Speirs L, Mitchell A, Przybyl H, Anderson D, Manos B, Schaenzer AT, Winchester K. Validation of a Postextubation Dysphagia Screening Tool for Patients After Prolonged Endotracheal Intubation. Am J Crit Care [Internet]. 2018[cited 2022 April 20]; 27(2):89-96. Disponivel em: https://doi.org/10.4037/ajcc2018483 [ Links ]
16 Teuschl Y, Trapl M, Ratajczak P, Matz K, Dachenhausen A, Brainin M. Systematic dysphagia screening and dietary modifications to reduce stroke-associated pneumonia rates in a stroke-unit. PLoS One[Internet]. 2018[cited 2022 May 9]; 13(2):e0192142. Disponivel em: https://doi.org/10.1371/journal.pone.0192142 [ Links ]
17 Spronk PE, Spronk LEJ, Egerod I, McGaughey J, McRae J, Rose L, Brodsky MB; DICE study investigators. Dysphagia in Intensive Care Evaluation (DICE): An International Cross-Sectional Survey. Dysphagia [Internet]. [cited 2022 May 9]. Disponivel em: https://doi.org/10.1007/s00455-021-10389-y. Epub ahead of print. [ Links ]
18 Garon BR, Sierzant T, Ormiston C. Silent aspiration: results of 2,000 video fluoroscopic evaluations. J Neurosci Nurs [Internet]. 2009[cited 2022 May 8]; 41(4):178-85 Disponivel em: https://doi.org/10.1097/JNN.0b013e3181aaaade [ Links ]
19 Marin S, Serra-Prat M, Ortega O, Clavé P. Healthcare-related cost of oropharyngeal dysphagia and its complications pneumonia and malnutrition after stroke: a systematic review. BMJ Open [Internet]. 2020 [cited 2022 May 10]; 10(8):e031629. Disponivel em: https://doi.org/10.1136/bmjopen-2019-031629 [ Links ]
20 Oliveira IJ, Rodrigues Couto G, Moreira A, Gonçalves C, Marques M, Lopes Ferreira P. The portuguese version of the gugging swallowing screen: results from its application. Rev. Mill [Internet]. 2021[cited 2022 May 16]; 2(16):93-101. Disponivel em: https://doi.org/10.29352/mill0216.24585 [ Links ]
21 Trevethan R. Sensitivity, Specificity, and Predictive Values: Foundations, Pliabilities, and Pitfalls in Research and Practice. Front Public Health [Internet]. 2017[cited 2022 May 16]; 5:307. Disponível em: http://dx.doi.org/10.3389/fpubh.2017.00307 [ Links ]
22 Christensen M, Trapl M. Development of a modified swallowing screening tool to manage post-extubation dysphagia. Nurs Crit Care [Internet]. 2018[cited 2022 May 16]; 23(2):102-107. Disponivel em: https://doi.org/10.1111/nicc.12333 [ Links ]
23 McHugh ML. Interrater reliability: the kappa statistic. Biochem Med [Internet]. 2012[cited 2022 May 17]; 22(3):276-82. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3900052/ [ Links ]
24 Oliveira I. J, Couto G. R, Santos R. V, Campolargo A. M, Lima C, Ferreira P. L: Best Practice Recommendations for Dysphagia Management in Stroke Patients: A Consensus from a Portuguese Expert Panel. Port J Public Health [Internet].2021[cited 2022 May 18]; 39:145-162. Disponivel em: https://doi.org/10.1159/000520505 [ Links ]
25 Ferreira FF, Fernandes LV, Oliveira I de J. Prevalência da disfagia em idosos institucionalizados. Rev Port Enf Reab. 2022[cited 2022 May 18]. Disponível em: https://doi.org/10.33194/rper.2022.218. [EPub ahead of print] [ Links ]
26 Azevedo P, Gomes B, Pereira J, Carvalho F, Ferreira S, Pires A, et al. Functional dependence at discharge from the intensive care unit: relevance for rehabilitation nursing. Revista de Enfermagem Referência [Internet]. 2019[cited 2022 May 18]; IV Série(No 20):37-46. Disponivel em: http://dx.doi.org/10.12707/RIV18084 [ Links ]











 text in
text in