1.Introduction
COVID-19 is considered the fifth pandemic after the 1918 flu pandemic. It is considered as “a controllable pandemic” by the WHO where all countries must be prepared to respond to. Act in solidarity, take steps to protect and care for those most at risk to suppress this pandemic. For low- and middle-income countries with weaker healthcare systems, this poses a great challenge (Wang et al., 2021; Tee et al., 2021). There is a specific concern that the disease presents higher risks for the elderly because of the likelihood of more dreadful outcomes from the virus. Because older people may not be fully independent, preventing them from being exposed to the virus can also be a difficulty. This pandemic has not only brought about biological phenomena but also implications of long-lasting psycho-social effects (Petersen et al., 2021). Although these effects are seen on a global scale, evidence shows that the virus has taken its biggest toll on the elderly population (Banerjee, 2020).
Early on in the course of the pandemic, the elderly were identified as the most vulnerable population. Firstly, according to the CDC, older individuals are at higher risk than younger individuals, particularly regarding the risk of a more severe course of the virus due to comorbidities. More than 80% of the deaths occur in adults over the age of 65 (Jaarsveld, 2020). Additionally, a study done by Mueller et al (2020), explains the idea behind why age is a risk factor in itself with regards to the aging immune system. Secondly, social distancing continues to play a very important role for this high-risk population. Several conditions were explicitly made to protect the elderly, including prohibiting visits to nursing homes and elderly care facilities (Fischer, et al. 2020). Families were kept from seeing their elder parents and grandparents since the beginning of the pandemic. It becomes important, therefore, to have a full understanding of how the elderly have been affected by the pandemic.
The researchers aim to identify the negative impact of COVID-19 on the elderly population. The review will cover negative impact on both the physical and mental health of the elderly. We aim to answer, how has the COVID pandemic affected the elderly populations concerning their health?
2. Methodology
2.1 Search Strategy
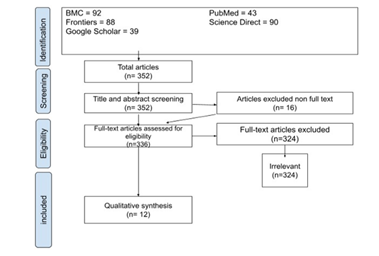
A search on articles published year 2020 and 2021 was conducted in BMC (BioMed Central), PubMed, Frontiers, Google Scholar and Science Direct using the following keywords: elderly, covid-19, negative impact, physical health, and mental health. The researchers utilized a systematic search of the literature based on the standards outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (2021) guidelines in the review and report writing procedures. There were nine (9) cross-sectional studies, two (2) commentaries, and one (1) retrospective study from the databases were identified and imported. Unrelated, duplicated, and unavailable full texts/abstract-only papers were removed. Following this, 2 reviewers (A & B) performed title/abstract screening and full-text screening of the articles for eligibility. Any discrepancies were resolved by another reviewer (C)Figure 1.
2.2 Eligibility Criteria
Specifics of inclusion are articles and journals addressing the impact of COVID-19 on our target age population, which is the elderly. World Health Organization classification on the elderly population will be followed, which is defined as 60 years and older. Eligibility criteria were based on the negative impact on physical health and mental health to categorize relevant articles. All studies that investigate the psychological and physical symptoms of the elderly resulting from the impact of the pandemic were included except for studies with systematic review and meta-analysis. Studies that analyzed mental and behavioral disorders due to the use of alcohol and other drugs, and studies carried out with children, adolescents, and pregnant women were excluded.
2.3 Data Extraction
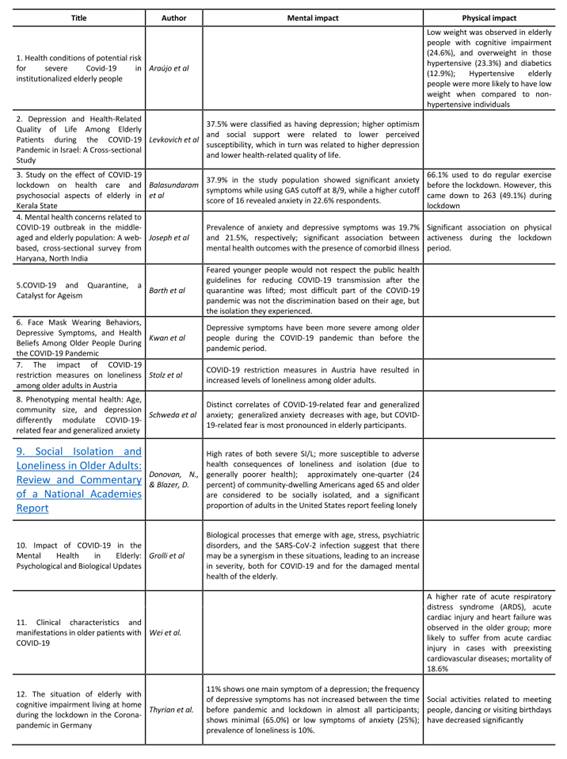
Extraction of the following information was done by five researchers (D, E, F, G, & H) using a standardized form with the following details: Title, authors, physical impact, and mental impact.
2.4 Risk of Bias Assessment
Five reviewers (I, J, K, L, & M) independently assessed the quality of articles using AACODS Appraisal Checklist (Tyndall, 2010) and Mixed Method Appraisal Tool (MMAT) (Hong et al, 2018) for two theoretical and ten research articles, respectively. Individual elements from seven questions were answered based on judgment as to yes, no, and can’t tell. On the other hand, AACODS Checklist for Gray Literature was used by the researchers who evaluated records that were not under the control of conventional publishing and distribution agencies. This classification encompasses government documents, commentaries, opinions, news reports, policy literature, speeches, and several others (University of Exeter, 2022). AACODS Checklist consists of approximately 25 questions that are answerable by a “yes” or “no”. Six main factors were considered by AACODS which included the profile of those behind the intellectual content (Authority); the validity and reliability of objectives and methodology, and the steps taken to be evaluated by a reputable institution (Accuracy); the limitations set by the articles (Coverage); the acknowledgement of bias (Objectivity); the relevance of the records in terms of time (Date); and the importance of the article in the area of research (Significance) (University of Canberra, n.d.). Overall, the articles included in the study are low risk bias.
3.Results
Twelve (12) studies were included in the review (Table 1). Five studies were conducted in Europe , three in Southeast Asia, three in America and one in Western Pacific. Study areas were geriatrics, neurobiology, mental health, public health, medicine, and psychiatry. Three authors were able to identify negative impact on both physical and mental health, seven on mental health, and two on physical health.
Chronic conditions and comorbidity of the elderly increase vulnerability to COVID-19 and are more likely to promote life-threatening respiratory failure and multi-systemic involvement (Araujo et al., 2021). Likewise, the poor outcome in the elderly population with COVID-19 was found out to be independently associated with increased incidence of acute cardiac injury and heart failure. In addition, low weight was observed in elderly people and overweight in those hypertensive and overweight. But it was found out that hypertensive elderly has low weight when compared to non-hypertensive elderly. Regular exercise and physical activeness on the other hand went down during pandemic. While lockdown did not only limit social contact of the elderly with others, it has adversely affected the social activities related to meeting people such as dancing or visiting birthdays.
COVID-19 related fear increases in the presence of risk diseases and are most pronounced in the elderly. They experienced fear of acquiring COVID-19 when quarantine was lifted because younger generations had difficulty in following protocols. It is common in urban communities compared to rural communities in which generalized anxiety is more prevalent. In addition, COVID-19 infection showed a synergistic effect on the mental health of the elderly such as psychological distress, anxiety, and depression. Although one author mentioned that depression, anxiety and loneliness showed only a small impact during the pandemic, another author was able to explore and associate depressive symptoms to wearing of mask behavior among the elderly. Loneliness was higher during the lockdown and social isolation can be life-saving, but to the elderly, it is a more troubling experience than aging because it deprives them of their fundamental human need for companionship.
3.Discussion
The researchers have conducted a systematic review of the negative impact of COVID on the elderly. The current existing literature identifies physical and mental impact individually but fails to cover the overall negative impact of COVID on this population. Although all ages are susceptible to the effects of the virus, the elderly have higher morbidity and mortality when compared to younger individuals, mainly due to the stronger association with comorbidity seen in the elderly. A retrospective study was done at the Renmin Hospital and Wuhan University, China, which found that older patients presented with more severe mortality of 18.6%, as compared to the younger and middle-aged patients. Their findings concluded that aging is complex and multi-factorial, thus factors such as frailty, nutritional status, immunosenescence, and coexisting diseases all contributed to the overall higher mortality of the elderly (Wei et al., 2020). Another study done in a Long-Term Care Facility in Brazil identified that chronic heart and lung diseases, chronic kidney disease on dialysis, liver disease, immunosuppressed conditions, and severe obesity lead to a higher risk for developing the severe form of COVID-19 (Araujo et al., 2021). Thus, although COVID-19 has taken its toll on a pandemic scale, the elderly population must be given extra care because of their heightened vulnerability to the virus.
Stricter quarantine measures were imposed by countries such as Israel and United Kingdom on older adult citizens (70 years and older) compared to younger age groups. After lifting quarantine measures in France, discrimination seems to have also increased against older adults (Barth et al., 2021). Aside from the heightened effects on the elderly due to comorbidity, other aspects of their physical health were affected by COVID as well. A study done in Kerala State, India, revealed that within their study population, there was a 25.5% decrease in the participants who no longer engaged in exercise and a 48.3% decrease in medical follow-ups and consultation among the participants before and during the lockdown (Libu et al., 2021). Therefore, COVID has made both direct and indirect effects on the physical well-being of the elderly.
Throughout the pandemic, because of the higher vulnerability of the elderly, physical and social isolation was highly emphasized. Therefore, not only did this population experience higher levels of physical stress during the pandemic but also the mental stress brought about by heightened social isolation (Javed et al., 2020). It was also mentioned in the article done by Johnson et al., (2020) that the strongest mental health impact during pandemic is among the elderly and areas where social distancing is being implemented. Although social isolation can be life-saving, it is linked to the deprivation of older adults from companionship and community (Sikali, 2020). There is then a higher burden placed on the elderly with a lack of access to technology for video-conferencing and chatting, particularly those in lower socioeconomic communities, as well as those with cognitive and social impairments (Donovan et al., 2020). Social isolation leaves older adults more susceptible to experiencing loneliness, anxiety, and excessive worrying. A study done in Austria identified that the elderly already had an increased risk of loneliness before the pandemic due to factors such as widowhood, living alone, or mobility limitations. The findings of such a study included that the loneliness levels in 2020 were increased compared to previous years and that levels were higher particularly during a lockdown, but decreased with re-opening phases (Stolz et al., 2021). A cited study from Vietnam Nguyen et al., (2020) identified possible causes of depressive symptoms in the elderly including: “Pandemic risk factors such as unforeseeable threats, social isolation and person and economic burden, pre-pandemic risk factors such as the social crisis in some regions and unmet mental health services and age-specific risk factors such as comorbidity of brain disorders or systemic diseases, psycho-social changes including bereavement and loss, change of role and loss of social status, and receiving institutional care” (Kwan et al., 2021). There are varying findings regarding the comparison between depressive levels seen in the elderly. A study conducted in India sought to identify the difference, but none of the results revealed no statistical significance between the middle-aged (50-65 years) and elderly (>60 years) (Joseph et al., 2020). The study’s limitations simply prompt encouragement for more research regarding the difference to tell the degree of impact on the elderly.
According to Johnson et al (2020), one of the participants who is a sixty-year-old woman answered “I feel scared. I am older and I take immunosuppresants.” This could be due to a shifted focus of this population to a more health-related fear as opposed to generalized fear, due to preexisting vulnerabilities (Schweda et al., 2020). In Germany, lower levels of loneliness in the elderly compared to the general population were possibly influenced by the idea of short-term isolation or restriction with a clear cause and foreseeable end. Additionally, the study identified a “positive effect” of the pandemic. This is the frequency of talking to family and friends by phone, gardening, or other similar activities with less personal contact (Thyrian et al., 2020). The decreased levels of generalized anxiety and loneliness seen in the elderly are a common trend seen throughout the various journals involved in this systematic review. In the elderly around the world, more than 20% live with psychiatric disorders or neurological disorders such as dementia, major depressive disorder (MDD), and anxiety. Similarly, the higher degree of chronic inflammation brought about by COVID and aging can predispose the elderly to psychiatric disorders, such as anxiety and MDD (Grolli et al., 2021). Thus, special attention should be diverted to the elderly, especially those with preexisting neurological disorders.
A study in Israel made the association of depression with “lower optimism, lower social support, and higher perceived susceptibility” (Levkovich et al., 2021). Thus, emphasis must be placed on the promotion of higher optimism and social support to serve as a buffer against the emotional stress placed upon the elderly during this time. Overall, however, this provides for a comprehensive and unbiased synthesis of the current literature. Possible limitations may be set within the journals themselves.
5.Conclusion
The findings summarized in this review suggest that older adults experienced negative impact, both physically and mentally, related to the ongoing pandemic. This might be due to fewer changes in their daily routine compared to their routine before the pandemic. Impact of COVID-19 on physical health to elderly were weight loss, lesser time of exercise, decreased social activities, increased respiratory and heart diseases, and increased mortality. On the other hand, identified impact on mental health were higher depression, anxiety, fear of acquiring COVID due to irresponsible younger generations, discrimination and isolation, increased levels of loneliness, and generalized anxiety. Institutions responsible should consider the mental health of the elderly regarding public health measures and access to health care, both during the pandemic and for future health crises.
6.Recommendations
Older people are especially vulnerable to social isolation, loneliness, and depression resulting in a significant effect on their health (Levkovich et al., 2021 & Balasundaram et al., 2021). The corona-virus outbreak has highlighted some of the barriers that the elderly has had to face, especially when it comes to the lack of access and inexperience to technology. To bridge this technological gap, the researchers recommend that programs should be launched to teach basic technological skills to the elderly. This technology can be confusing to navigate; hence, volunteer programs that connect the elderly with individuals who could provide technological support are beneficial, as this would also provide companionship and connection within their community.
To combat loneliness and social isolation, it is further recommended that the elderly participate in learning how to access services that provide video conferencing, such as Facebook Messenger, Zoom, G meet, Skype, and Face Time. These platforms are offering training sessions, tutorials, and free interactive daily webinars to help users familiarize themselves with understanding the services that they provide. Programs to teach and assist the elderly to connect with their family and friends through video calls may help reduce loneliness and encourage them to use it frequently.
With the elderly population facing a significant risk of developing severe illness due to Covid-19, home isolation has been recommended to protect them. These physical limitations have prevented the elderly from performing their daily activities resulting in a sedentary lifestyle. Therefore, the researchers also recommend that programs providing virtual exercise classes should be considered to help the elderly stay active in the comfort of their own homes. Likewise, promoting digital exercise programs that provide a step-by-step exercise tutorial that could improve their health and quality of life is recommended. Exercise programs should also be launched through a live video chat platform, allowing the elderly to interact with the trainer as well as other people who are participating. Accessing healthcare services during the pandemic is challenging for the elderly, leaving them with minimal alternatives unless they have access to tele-health. With elderly individuals unprepared for video visits due to inexperience with technology, it is also recommended that caregivers, family, and friends assist and teach the elderly person how to operate these services. For the elderly individuals who do not have access to technological devices, as well as those who reside in developing countries that might not have the services needed to access tele-health, such as internet and electricity, it is recommended that regular landline phone calls be considered to receive the same quality of care.
In addition, it is hoped that the elderly considers taking the opportunity to join these programs that have been recommended so that they would gain confidence to use and incorporate technology into their daily lives. These programs would benefit them tremendously, not only by allowing them to virtually connect with family and friends, but will also help them in daily activities, such as online shopping, access to tele-health services, and staying up to date with current events.