1.Introduction
Worldwide, cardiovascular diseases are the main cause of morbidity, with heart failure (HF) accounting for about 20% of new hospitalizations (Direção Geral da Saúde, 2017). HF is one of the primary causes of the increasing public health costs, and the incidence rate and mortality associated with heart disease (Guerra et al., 2017; Panjrath & Ahmed, 2017). Patients with HF can have acute attacks and need hospitalization and emergency medical treatment. It is predicted that in the next decade, the number of people hospitalized for HF will increase significantly, which will put more and more pressure on the health-care system (Alpert et al., 2017; Savarese & Lund, 2017).
HF is a chronic disease with a slow progression, characterized by signs and symptoms like dyspnea, orthopnea, fatigue, effort intolerance, jugular engorgement, and malleolar edema; the symptoms are caused by structural or functional cardiac alterations, which reduce cardiac output and increase intracardiac pressures at rest or exertion (Silva-Cardoso & Campelo, 2021). Symptoms related to cardiac changes, such as arrhythmia and dyspnea, compromise oxygenation, and HF patients encounter great difficulties regarding what is termed Basic Human Needs (BHN)-breathing, moving, rest and sleep (Pereira et al., 2016). As treatment options for HF have evolved, patients have a better understanding of the overall burden of HF; as such, this has contributed to the development of care methods more adjusted to the needs of these individuals (Zhang, Bai & Huang, 2020). Nursing care is important for people who experience illness; nurses provide patients assistance for making changes in their behavior to achieve good health. At present, nurses use interventions in the clinical settings based on evidence, and with a particular emphasis on outcome assessment (Smeulders et al., 2010).
HF is one of the main chronic diseases that leads to reduced capacity to satisfy BHN, which is a main cause of hospitalization in these patients. HF has a huge impact on family and social life and often triggers anxiety due to the difficulty in being autonomous. The nurse's intervention is essential with these patients, especially in the preparation for returning home and facilitating the safe hospital-home transition. The safe transition enables the person and family to manage the health/disease condition, which implies in-depth knowledge of all its dimensions and with a holistic, person-centered perspective.
Nurses are part of the professional health team who are responsible for helping patients to develop skills to manage their symptoms (e.g., recognize relevant symptoms) and the therapeutic regimen; they promote empowerment, thereby enhancing a patient’s well-being and reducing readmissions (Vilas-Boas & Follath, 2006; Zhang et al., 2020). The aim of this study was to identify the most common nursing interventions for assisting with and improving the BHN of patients with HF, including those that promote relief of their symptoms, as well as facilitate their safe care transition from hospital to home.
2.Methodology
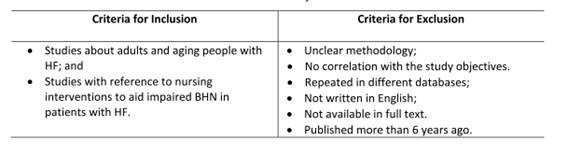
This is a mixed-methods systematic review study about evidence-based interventions that contribute to nursing practice. This approach is rigorous, explicit, and reproducible; it uses specific strategies and limits the bias in the selection of articles. It is about stringently evaluating primary studies in a specific area, through predetermined criteria according to the research question (Bettany-Saltikov, 2012). To formulate the research question, we considered the recommendations of the Joanna Briggs Institute (JBI, 2011). Based on the study problems and for a wider understanding of this phenomenon, the following question was created using the PICO format (Sousa et al., 2018): In patients with HF (population), what are nursing diagnoses and the most effective nursing interventions (intervention) to promote an individual’s ability to manage their BHN, to relieve their symptoms, and to support safe transition of care from hospital to home (outcome)? The review was performed using the electronic databases CINAHL and MEDLINE. Boolean descriptors and operators were also used in creating the search strategy, specifically: [(Nursing Care OR Nursing Diagnosis OR Nurs*) AND (Heart Failure) AND (Hospitalization or Transitional Care)]. To obtain relevant papers given the review question, we established inclusion and exclusion criteria (Table 1).
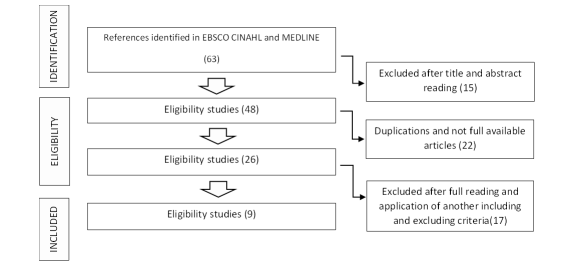
To select studies, we considered all papers with at least 75% of the quality criteria as per JBI (JBI, 2014a). The data were collected in October 2021; 63 articles were retrieved using our search strategy, after which they were analyzed by two independent reviewers to assess methodological quality using the JBI classification and following the inclusion and exclusion criteria. The method we followed is shown in Figure 1.
The two independent investigators followed the same method, with the sequence suggested by the guidance of Mixed methods systematic reviews (Stern et al., 2020) The results were obtained in stages, from reading the title, the abstract, to the full text. The results obtained were compared and agreement between investigators was considered. In cases of disagreement or doubt, the article was moved to the next phase of analysis. A table was created to systematize the information collected and facilitate the analysis and interpretation. The investigators carried out a survey of diagnoses and nursing interventions, through the analyze the content of the results and discussion of the articles selected. The articles were subjected to an identification process regarding level evidence considering JBI levels of evidence (JBI,2014b)
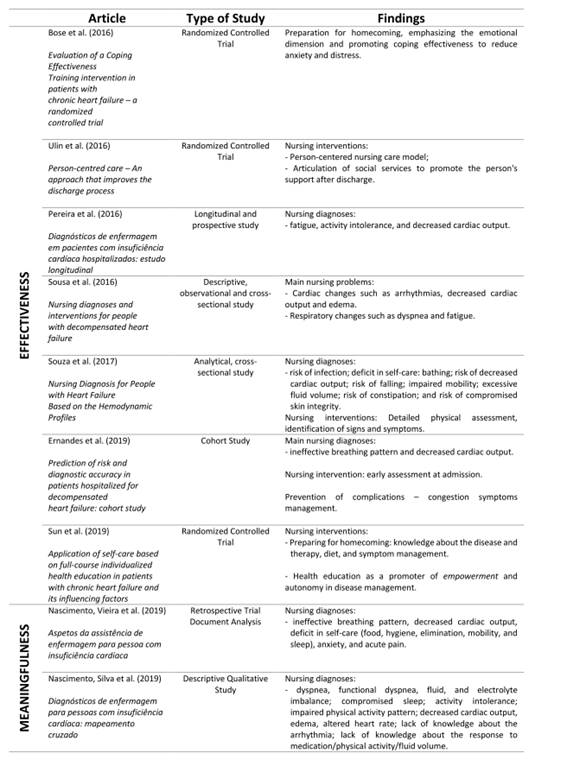
The final included nine studies for this review are the following:
Effectiveness: three (3) randomized controlled studies (Bose et al., 2016; Sun et al., 2019; Ulin et al., 2016) - Level of evidence 1c; one (1) cohort study (Ernandes et al., 2019) - level of evidence 3c and three (3) observational studies (Pereira et al., 2019; Sousa et al., 2016; Souza et al., 2017) - level of evidence 4b.
Meaningfulness: two (2) qualitative studies (Nascimento, Silva, et al., 2019; Nascimento, Vieira, et al., 2019) - level of evidence 3. In this section, we present the main results as based on the nine selected studies. The HF patient has symptoms such as dyspnea, edema, and arrhythmias; as such, nursing interventions are essential to support the patient’s BHN and the disease management. The nursing approaches in this regard are shown in the following table.
Table 2. Studies included in the review
3.Discussion
The main finding in this review study, as based on the selected studies, is about the needs of the patient with HF and the diagnoses and interventions by nurses. From the research, the interventions of greatest importance for the patient with HF are: effective management of impaired BHN to alleviate symptoms (Ernandes et al., 2019; Nascimento, Silva et al., 2019; Nascimento, Vieira et al., 2019; Pereira et al., 2016; Sousa et al., 2016; Souza et al., 2017) and transitional care from hospital to home, including disease management and health education (Sun et al., 2019; Bose et al., 2016; Ulin et al., 2016).
Nursing diagnoses were formulated based on the patient's symptoms and needs. The most common clinical manifestations were signs of congestion, such as dyspnea and edema, and fatigue. The diagnoses were designed according to these clinical manifestations and their consequences. It appears the most prevalent were decreased cardiac output, ineffective breathing pattern/dyspnea, excessive volume of fluids/edema, activity intolerance, and fatigue. The BHN most compromised is breathing. If a person has dyspnea and other signs and symptoms of congestion, this will compromise other BHNs, such as moving and maintaining a correct posture; this is represented by the diagnoses of activity intolerance, and impaired mobility, fatigue, and poor sleep (Nascimento, Vieira et al., 2019; Pereira et al., 2016; Souza et al., 2017).
Early and detailed assessment-from the time of admission throughout the hospital stay-for the person with HF is essential, so that it is possible to manage the symptoms and effectively address their BHN (Ernandes et al., 2019). Sousa et al. (2016) identify several nursing interventions that make it possible to alleviate symptoms (aligned with nursing diagnoses) in the patients who are hospitalized. If the patient has arrhythmias, controlling vital signs is essential and basic and advanced life support is necessary. In the case of decreased cardiac output, one must monitor for signs of shock and peripheral perfusion, and in the presence of edema, one must assess, for example, the need for fluid restriction, fluid balance and weight surveillance. For the diagnosis of dyspnea and fatigue, the main interventions are related to oxygen management, monitoring signs of hypoxemia, and managing periods of rest and effort. The nurse's intervention should also focus on promoting comfort in the sense of relieving symptoms, such as pain and anxiety (Nascimento, Vieira et al. 2019). Assessment for signs of congestion should be part of determining if the patient’s clinical status is appropriate for discharge; further, respiratory symptoms should be investigated, such as orthopnea, paroxysmal nocturnal dyspnea, and pulmonary edema, as well as signs of jugular vein engorgement and the person's functionality and effort tolerance (Nascimento, Silva et al., 2019; Nascimento, Vieira et al., 2019; Sousa et al., 2016).
Individualized information about the health situation of each patient is important and must be explained in language adapted to everyone’s understanding. The information should include the typical signs and symptoms suggestive of health status deterioration and worsening, the strategies to be adopted for its monitoring, medication(s) and the importance of therapeutic adherence in maintaining health status, as well as diet and health habits, such as promotion of physical exercise that is right for them (Sun et al., 2019).
Preparation for hospital discharge-transitional care-should begin at the time of patient admission and should take place throughout the entire length of stay. The hospital discharge plan should include the following objectives: to schedule a follow-up appointment (Bose et al., 2016); to ensure therapeutic management; to ensure the person recognizes signs and symptoms of HF; to assess the factors that may have an impact on discharge planning; and to educate the person and to provide the support resources the person can use after discharge (Ulin et al. 2016). In the study by Sun et al. (2019), they revealed health education properly adapted to the patient’s/family’s learning abilities and their active participation in the care, promoted empowerment and independence of patients with HF.
In a systematic review of the literature by Albert (2016), they highlight the importance of nurses preparing for the discharge of patients with HF. Thus, to ensure that information is transmitted, the author recommends the creation of a checklist adopted by the multidisciplinary health team, which must be used by all professionals. This strategy would ensure the transmission of necessary information to promote empowerment of the patient at discharge.
The positive impact of person-centered care and the empowerment of patients with HF in the management of their own health condition through the promotion of all BHN is noteworthy (Ulin et al., 2016). A careful assessment of the person, and of the characteristics that can influence the promotion of independence and empowerment (domicile conditions, socioeconomic status, health status, social and family support, learning capacity) defines a starting point for the elaboration of a plan of intervention that responds to the needs of patients and their families and a safe hospital-home transition (Sun et al., 2019). The hospital-home transition can cause some insecurity and anxiety in these patients and for this reason Bose et al. (2016) mention the importance of promoting effective coping strategies for problem-solving and stress and anxiety management, while promoting social interaction.
Ulin et al., (2016) also identified a nursing person-centered care model is essential in helping nurses identify people's concrete needs, and to include individuals in their care plan as active agents of their health-disease process. The nurse's intervention, according to the person-centered care model, begins with the patient history where important information is collected for the identification of nursing diagnoses, and patient motivations, and objectives in view of their health condition, and to make decisions for the nursing intervention (Sun et al., 2019).
Corroborating the studies identified in this research, there is evidence that nursing care focused on the needs of these patients, such as hospital-home transition preparation, educational intervention and follow-up by nurses have a significant positive impact, reducing their readmissions (Ingles, 2020). The systematic reviews conducted by Albert (2016) and Ryan et al. (2019) also highlight the relevance of nursing interventions in this domain, especially through health education and preparation for the discharge of the patient with HF, namely in therapeutic self-management and identification of symptoms, thus promoting their empowerment, independence, quality of life, and reducing the risk of readmissions.
The current study has the limitation of being a secondary study, also the possibility that was been missed some relevant studies in the revision because have used just two databases.
4.Final Considerations
Nurses’ interventions for the hospitalized patient with HF in the acute phase are about aiming to establish clinical stability, responding to their BHN and to prevent other complications. The most prevalent interventions are aligned with nursing diagnoses of decreased cardiac output, ineffective breathing pattern, excessive fluid volume, activity intolerance and self-care deficit. There is a need to develop interventions in the control of anxiety because this disease is a very difficult health situation for the patient and their family. Preparing for discharge is a fundamental intervention, as it aims to enable the patient to manage their health situation, reduce the frequency of hospitalizations and reduce the progression of the disease. Promoting empowerment by training the HF patient about pathophysiology, warning signs and symptoms, how to monitor their health status, management of the therapeutic regimen, diet, and physical activity, are important to prepare them for discharge. Researchers highlight the importance of family integration in care planning and training for returning home.
Due to the prevalence of this disease in population and given the problems and complications for the patient and family, nurses need to give greater attention to all the aspects of this problem and invest in educational and monitoring programs for these patients.
Nurses are members of the professional health team who are responsible for helping patients to develop skills to manage their health and disease conditions, like recognizing relevant symptoms, the therapeutic regimen, promoting disease self-management and empowerment, thereby reducing readmissions and promoting their well-being.