Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
GE-Portuguese Journal of Gastroenterology
Print version ISSN 2341-4545
GE Port J Gastroenterol vol.22 no.2 Lisboa Apr. 2015
https://doi.org/10.1016/j.jpge.2014.12.001
ENDOSCOPIC SNAPSHOT
Incidental Diagnosis of Mantle Lymphoma Made by Sigmoidoscopy
Diagnóstico Incidental de Linfoma do Manto por Proctossigmoidoscopia
Jorge Lagea,∗, Pedro Pimentel-Nunesa, Duarte Menezesa,b, Ana Sílvia Luísb, Catarina Brandãob, Luís Moreira-Diasb
a Gastroenterology Department, Instituto Português de Oncologia do Porto Francisco Gentil, Porto, Portugal
b Pathology Department, Instituto Português de Oncologia do Porto Francisco Gentil, Porto, Portugal
* Corresponding author.
A 82-year-old man has been followed in our oncology hospital after prostatic cancer and prostatectomy. He was medicated with gonadotropin releasing hormone superagonist goserelin and olmesartan for arterial hypertension.
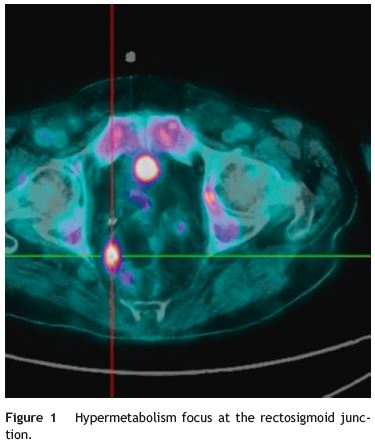
Due to the recent installation of orthopnea, a chest X-ray was carried out, revealing a mass in the right hilar region which was subsequently characterized as right hilar and mediastinal lymphadenopathy by chest CT. Bronchoscopy with bronchial biopsies, citology and microbiological studies revealed no signs of malignancy or infection. Taking into consideration the patients medical history and the occasional back pain he referred, PET scan was thought to be the appropriate following exam. In addition to confirming hypermetabolism in the already known lymphadenopathies, PET-CT scan also showed a hypermetabolic focus at the rectosigmoid junction (Fig. 1).
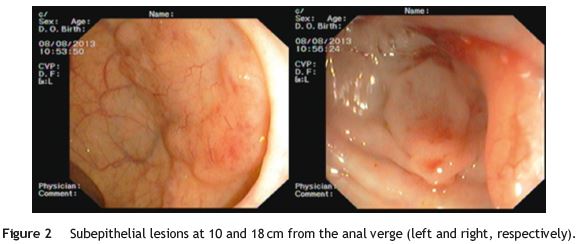
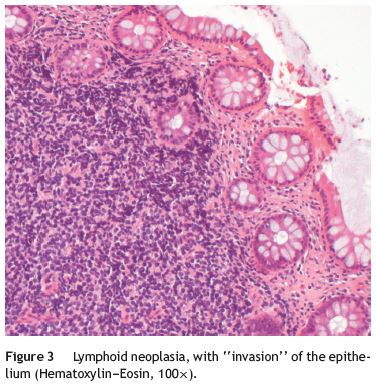
Sigmoidoscopy was performed and revealed two subepithelial lesions at 10 and 18 cm from the anal verge (Fig. 2). Biopsy specimens were obtained by using a biopsy-on-biopsy technique. Histological examination showed the presence of a lymphoid neoplasia of small sized cells with irregular nuclei, fine chromatin, small inconspicuous nucleoli and pale indistinct scant cytoplasm, with the peculiarity that there was involvement of the epithelium (Fig. 3). Immunophenotype studies were consistent with the diagnosis of mantle cell lymphoma: expression of CD20 and other pan-B cell antigens and overexpression of cyclin D1. The patient was referred to the onco-hematology department to start treatment.
Approximately 40% of lymphomas have extranodal manifestations, and the most common site of extranodal involvement is the gastrointestinal tract.1 Nonetheless, colorectal lymphoma remains a rare clinical entity.2 Gastrointestinal involvement in mantle cell lymphoma, presenting with intestinal symptoms, was estimated at 30% but recent studies show an infiltration even in 92% of cases.3 The clinical case reported by the authors report a first diagnosis by colonic biopsy/approach, an interesting finding with iconography that supports the case.
References
1. Zucca E, Roggero E, Bertoni F, Cavalli F. Primary extranodal non-Hodgkins lymphomas. Part 1: Gastrointestinal, cutaneous and genitourinary lymphomas. Acta Oncol. 1997;8:727-37. [ Links ]
2. Quayle FJ, Lowney JK. Colorectal lymphoma. Clin Colon Rectal Surg. 2006;19:49-53. [ Links ]
3. Salar A, Juanpere N, Bellosillo B, Domingo-Domenech E, Espinet B, Seoane A. Gastrointestinal involvement in mantle cell lymphoma: a prospective clinic, endoscopic, and pathologic study. Am J Surg Pathol. 2006;30:1274-80. [ Links ]
* Corresponding author
E-mail address: jorgetl86@gmail.com (J. Lage).
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interest
The authors have no conflicts of interest to declare.
Received 29 September 2014; accepted 19 December 2014














