Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
GE-Portuguese Journal of Gastroenterology
Print version ISSN 2341-4545
GE Port J Gastroenterol vol.23 no.5 Lisboa Oct. 2016
https://doi.org/10.1016/j.jpge.2016.01.005
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
Idiopathic Pneumatosis Intestinalis, Radiological and Endoscopic Images
Pneumatosis Coli Idiopática, Imagens Radiológicas e Endoscópicas
Maria Fraga * , Maria João Nunes da Silva, Margarida Lucas
Medicine 2 Department, Hospital de Santa Maria Centro Hospitalar de Lisboa Norte, Lisbon, Portugal
* Corresponding author.
Keywords: Endoscopy, Gastrointestinal. Pneumatosis Cystoides Intestinalis/diagnosis. Pneumatosis Cystoides Intestinalis/radiography.
Palavras-chave:Endoscopia Gastroeintestinal. Pneumatose Cistoide Intestinal/diagnóstico. Pneumatose Cistoide Intestinal/radiografia.
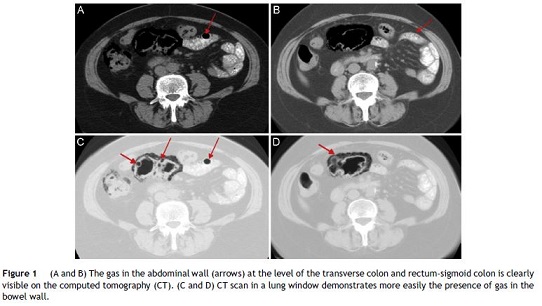
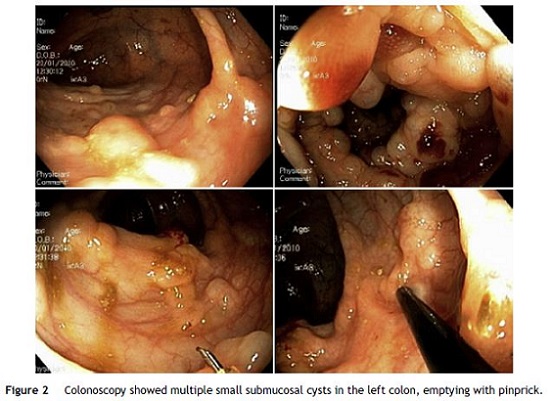
A 66-year-old female, hypertensive, presented with pain and abdominal distension, constipation, flatulence and “pencil thin stool” that developed over six months, with no other symptoms, namely weight loss. There was no travel history, diet change, sick contacts, abdominal surgery or gastrointestinal diseases. She denied alcohol or tobacco. She was not taking any medication or supplements with the exception of the usual antihypertensive therapy. In the physical examination she was hemodynamically stable with abdominal distention and mild abdominal pain, but without peritoneal reaction. Laboratory evaluation was normal as well as gasometric parameters. Abdominal computed tomography (CT) evidenced the presence of gas in the abdominal wall, at the level of the transverse and rectum-sigmoid colon (Fig. 1), with no other changes. Colonoscopy showed small emphysematous formations in the left colon, emptying with pinprick (Fig. 2) confirming pneumatosis intestinalis (PI). An idiopathic PI was admitted in view of the absence of a secondary cause of PI and endoscopic images of discrete bubbles of gas instead crescentic or linear gas collections more often associated with secondary PI. After low fiber diet, dimethicone, laxatives and two weeks of oral metronidazole the complaints disappeared as well as PI on abdominal CT three months later. PI is a rare clinical entity that can be associated with several diseases including intestinal ischemia and bowel perforation.1 In 15% of the cases is idiopathic, occurring in a benign context1,2 and medical therapy can induce remission3–5 as illustrated here.
References
1. Lassandro F, Valente T, Rea G, Lassandro G, Golia E, Brunese L, et al. Imaging assessment and clinical significance of pneumatosis in adult patients. Radiol Med. 2015;120:96-104. [ Links ]
2. Blair HA, Baker R, Albazar R. Pneumatosis intestinalis an increasingly common radiological finding, benign or life-threatening? A case series. BMJ Case Rep. 2015;18. [ Links ]
3. Tseng C, Yen C, Chen M. Pneumatosis cystoides intestinalis. Formos J Surg. 2011;44:192-5. [ Links ]
4. Ellis BW. Symptomatic treatment of primary pneumatosis coli with metronidazole. Br Med J. 1980;280:763. [ Links ]
5. Adar T, Paz K. Pneumatosis intestinalis. N Engl J Med. 2013;368:e19. [ Links ]
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Conflicts of interest
The authors have no conflicts of interest to declare.
Acknowledgement
The authors would like to acknowledge Dr. A. Marques (Gastroenterology Department of University Hospital Santa Maria/CHLN) for the important collaboration.
* Corresponding author.
E-mail address: mariaffraga@gmail.com (M. Fraga).
Received 8 November, 2015; accepted 10 January 2016














