Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.1 Lisboa fev. 2017
https://doi.org/10.1159/000450871
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
Spleen Endoscopy: A sui generis Diagnosis of Colon Cancer
Esplenoscopia: Um Diagnóstico sui generis de Neoplasia do Cólon
Ana Torres Oliveira, Paulo Souto, Carlos Sofia
Gastroenterology Department, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal
* Corresponding author.
Keywords: Abscess; Colonic neoplasms; Splenic diseases
Palavras-Chave: Abcesso; Neoplasias do cólon; Doenças do baço
Clinical Case
A 55-year-old man was hospitalized with fever of unknown origin associated with nonspecific complaints of anorexia, tremors, myalgia and lower back pain. He had no gastrointestinal or genitourinary symptoms. Physical examination was normal. He had a history of microcytic anemia with 3 months of evolution medicated with oral iron supplementation. He also had arterial hypertension medicated with an antihypertensive, and radical prostatectomy had been performed 7 months earlier for cancer. No known epidemiological context was observed and the patient had a good socioeconomic status.
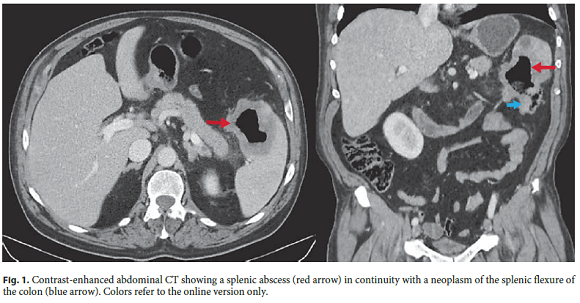
The initial analytical profile revealed anemia with a haemoglobin level of 8.7 g/dL and elevation of inflammatory parameters (white cell count of 18.6 × 10 9 /L and C-reactive protein of 20.0 mg/dL). Blood and urine cultures, infectious disease serology, serum protein electrophoresis and prostate-specific antigen were negative. Abdominal ultrasound performed in the urgency setting was normal. Given the persistence of complaints and the inconclusive laboratory study, an abdominal computed tomography (CT) scan was performed. In the spleen, there was a hypodense, 6.3-cm lesion with a central liquid component and peripheral contrast enhancement suggesting an abscess. This lesion was continuous with the colon splenic angle whose wall was thickened suggesting an expansive neoplasm (Fig. 1). It also revealed multiple infracentimetric pulmonary nodules that could be related to metastases.
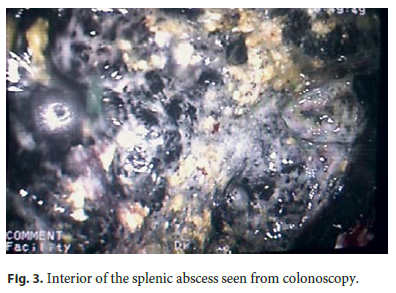
Colonoscopy was performed and at the splenic flexure, it revealed an exophytic, irregular and stenotic lesion followed by a dark-colored cavity corresponding to the interior of a splenic abscess allowing the direct visualization of the spleen (Fig. 2, 3). The biopsies taken on the colonic border of the lesion corresponded to an adenocarcinoma. The multidisciplinary team (encompassing oncologists and surgeons) opted for surgery; thus, the patient was admitted for left hemicolectomy with splenectomy.

The histopathological analysis of the surgical specimen revealed a low-grade adenocarcinoma of the splenic flexure of the colon (G2), with infiltration of all the wall layers and in continuity with the spleen (pTMN T4b N1b). Patient recovery was ordinary and he started adjuvant chemotherapy.
Discussion
The various presentations of colon carcinoma are well known, but splenic abscess is a rare presentation, with only a few case reports in the literature [1, 2]. Splenic abscess can occur due to trauma, hematogenous spread or direct invasion. Diagnosis is often delayed since the clinical manifestations are nonspecific and include fever, abdominal pain, and leukocytosis [3]. Although CT scan of the abdomen is the most common tool for the diagnosis of splenic abscess, in our case the endoscopic examination was imperative for the histological diagnosis of splenic flexure neoplasm. It also allowed the exceptional visualization of the spleen pulp. Treatment of pTMN T4 colon cancer involves en bloc resection of the tumor and the involved tissue or organ. The overall survival is similar to that of tumors not requiring resection of additional organs, if complete resection is accomplished [4]. Additional adjuvant chemotherapy might be indicated depending on the nodal status [5].
References
1 Kawamoto K, Teramoto T, Watanabe M, Kase S, Shatari T, Hasegawa H, et al: Splenic abscess associated with colon cancer: a case report. Jpn J Clin Oncol 1993;23:384–388. [ Links ]
2 Shinhar S, Nobel M, Rosso Y, Shimonov M, Entebi E: Splenic abscess as a presenting sign of colonic carcinoma. Dig Surg 1997;14:426–428. [ Links ]
3 Anuradha S, Singh NP, Agarwal SK: Splenic abscess – A diversity within. JIACM 2000;1:280–281. [ Links ]
4 Cartanese C, Carbotta G, Di Candia L, De Marini F, Girau Antonio, Zocchi G: A rare case of colon cancer with splenic abscess. Ann Ital Chir 2013;84:201–204. [ Links ]
5 Vezeridis MP: Colon cancer with splenic abscess. Arch Surg 2011;146:116. [ Links ]
Statement of Ethics
Protection of Human and Animal Subjects
The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of Data
The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to Privacy and Informed Consent
The authors declare that no patient data appear in this article.
* Corresponding author.
Dr. Ana Torres Oliveira
Gastroenterology Department, Centro Hospitalar e Universitário de Coimbra
Praceta Prof. Mota Pinto
PT–3000-075 Coimbra (Portugal)
E-Mail ana_t_oliveira@hotmail.com
Received: April 3, 2016; Accepted after revision: July 3, 2016














