Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.25 no.6 Lisboa dez. 2018
https://doi.org/10.1159/000487151
CLINICAL CASE STUDY
Distant Thromboembolic Disease Diagnosed by Endoscopic Ultrasound in Pancreatic Cancer: A Case Series
Doença tromboembólica distante diagnosticada por ultrassonografia endoscópica em neoplasias pancreáticas: uma série de casos
Catarina Atalaia-Martinsa, Pedro Pinto-Marquesa,b, Irina Mocanua, João Cortêz-Pintoa, David Serrab
aGastroenterology Department, Hospital Garcia de Orta, Lisbon, Portugal; bGastroenterology Department, Hospital da Luz, Lisbon, Portugal
* Corresponding author.
ABSTRACT
Thrombosis and cancer have a very well-known association. Pancreatic cancer has the highest risk for thrombotic events amongst gastrointestinal cancers and is a leading direct cause of death in cancer patients. We assessed the role of endoscopic ultrasound (EUS) in identifying distant thrombotic events in pancreatic cancer patients. We performed a retrospective review of all EUS cases for pancreatic cancer in two centers and assessed all remotely located thrombotic events diagnosed. In a period of 6 months, a total of 55 EUS for pancreatic neoplasm were performed and the following thrombotic events were identified in 4 patients (7.3%): pulmonary thromboembolism (75%) and vena cava thrombosis (25%). The authors present these 4 cases of thrombotic disease identified by EUS, 50% of them previously missed by noninvasive imaging. EUS evaluation is not seldom limited to the targeted lesion prior identified in other imaging studies. Vascular thrombus can be an incidental finding on EUS. If untreated, pulmonary embolism has a high overall mortality. This series underlines the importance of a systematic, station approach EUS technique, namely in the mediastinum, regardless of the clinical indication.
Keywords: Pancreatic cancer, Endoscopic ultrasound, Thrombosis
RESUMO
A trombose e o cancro têm uma associação bem conhecida. As neoplasias pancreáticas têm, de todos os tumores gastrointestinais, o risco mais elevado de eventos trombóticos e são uma das principais causas diretas de morte nestes doentes. Pretendeu avaliar-se o papel da ultrassonografia endoscópica (EUS) na identificação de eventos trombóticos à distância em doentes com neoplasias pancreáticas. Realizámos uma análise retrospetiva de todas as EUS realizadas por neoplasias pancreáticas em dois centros e analisámos os eventos trombóticos remotamente localizados diagnosticados. Num período de 6 meses, foram realizadas um total de 55 EUS por neoplasias pancreáticas e foram identificados estes eventos trombóticos em 4 doentes (7.3%): 75% tromboembolismo pulmonar e 25% trombose da veia cava inferior. Os autores apresentam estes 4 casos de doença trombótica identificada na EUS, sendo que metade deles não tinham sido diagnosticados pelos métodos de imagem não invasivos já realizados. Não infrequentemente, a avaliação por EUS é limitada à lesão alvo previamente identificada por outros métodos de imagem. Os trombos vasculares podem ser um achado acidental na EUS. Se não tratado, o tromboembolismo pulmonar tem uma alta taxa de mortalidade. Esta série reforça a importância de uma abordagem sistemática, por estação, na EUS, principalmente no mediastino, independentemente da indicação clínica.
Palavras-Chave: Cancro pancreático,·Ultrassonografia endoscópica,·Trombose
Introduction
Thrombosis and cancer have a very well-known association. Tumors can express procoagulant proteins [1]. Additional risk factors usually coexist including surgery, hospital admissions, immobilization, central venous access devices, chemotherapy, and new molecular targeted therapies. Evidence suggests that the absolute risk depends on the tumor type and cancer stage [2]. Pancreatic cancer has the highest risk for thrombotic events amongst all gastrointestinal cancers, with an incidence ranging from 17 to 57% [3]. Manifestations are multiple and include lower-extremity deep venous thrombosis, thrombophlebitis migrans, pulmonary embolism, disseminated intravascular coagulation, splenic vein thrombosis, mesenteric vein thrombosis, and spontaneous arterial thromboembolism. Thrombosis is a leading direct cause of death in cancer patients [4]. Recognition of vascular thrombi has thus become a cornerstone of the treatment of cancer patients. While direct vascular invasion is usually detected by computed tomography (CT) or magnetic resonance imaging (MRI) [5], these noninvasive imaging methods may fail to detect isolated vascular thrombi located remote from the primary tumor [6]. Endoscopic ultrasound (EUS) is useful in the detection of thrombi, even if previously undiagnosed by noninvasive imaging, and can be used to systematically scan the vascular system [5]. We assessed the role of EUS in identifying distant thrombotic events in pancreatic cancer patients.
Patients and Methods
We performed a retrospective review of all EUS cases for pancreatic cancer in two centers and assessed all remotely located thrombotic events diagnosed. In a period of 6 months, a total of 55 EUS for pancreatic neoplasm were performed. Thrombotic events were identified in 4 patients (7.3%) (male/female ratio 1: 1, mean age 67 years). Indications were pancreatic cancer staging (n = 3) and an abdominal mass of unknown origin (n = 1). In all of them, EUS-guided fine needle aspiration (FNA) was performed for the primary mass but not for the thrombi. In 2 patients CT staging had previously been performed with no evidence of thrombotic event and, after EUS-guided FNA, it was confirmed to be a thrombotic event.
Case 1
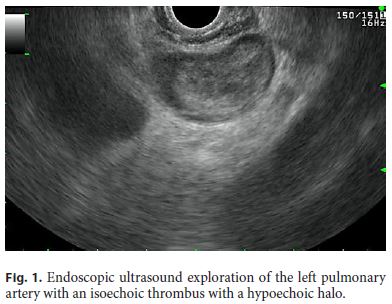
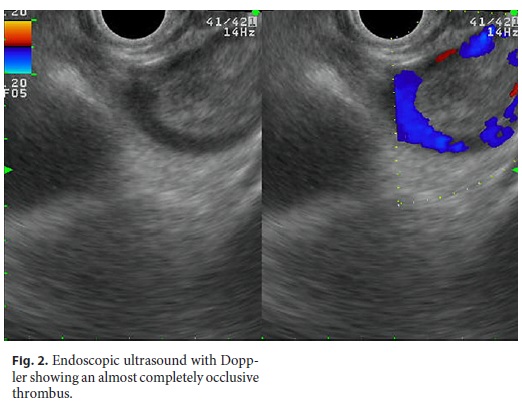
An 81-year-old woman was admitted with a diagnosis of deep vein thrombosis and bilateral pulmonary thromboembolism. Regarding her past medical history, she had undergone surgical resection of a retroperitoneal leiomyosarcoma 16 years prior. Thoracic-abdominal-pelvic CT identified a pancreatic body mass. EUS exploration confirmed a pancreatic neck mass with no vascular involvement. A left pulmonary artery thrombus was identified (Fig. 1, 2). Cytology and immunohistochemical evaluation were consistent with pancreatic leiomyosarcoma metastasis.
Case 2
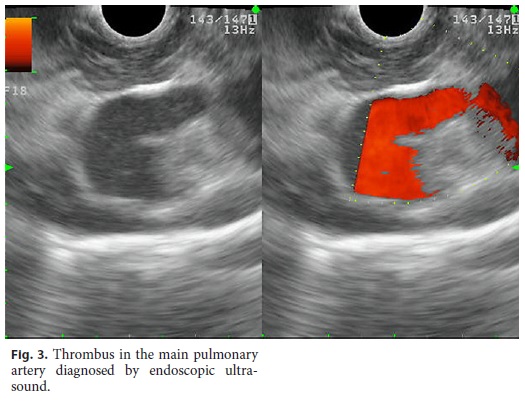
A 70-year-old man was referred from another hospital for EUS evaluation of a pancreatic tail mass previously seen on full-body CT imaging. EUS identified an ill-defined pancreatic tail mass in contact with the splenic artery. Mediastinal exploration revealed a main pulmonary artery thrombus (Fig. 3). Cytology was consistent with pancreatic adenocarcinoma. The reported finding was not diagnosed by thoracic CT, but only confirmed after CT pulmonary angiography protocol.
Case 3
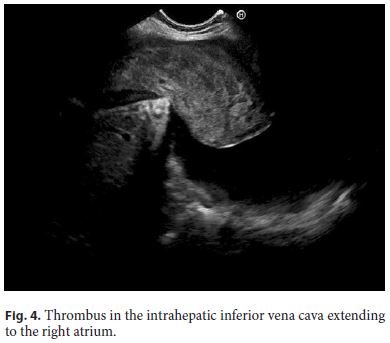
A 46-year-old woman was referred for EUS evaluation of an abdominal mass seen on thoracic-abdominal-pelvic CT which had also revealed inferior vena cava thrombosis and hepatic and pulmonary metastasis. EUS identified a voluminous heterogeneous hypervascular abdominal mass and a large thrombus filling the intrahepatic inferior vena cava with right atrial extension (Fig. 4). Cytology and immunohistochemical analysis were consistent with a pancreatic neuroendocrine tumor.
Case 4
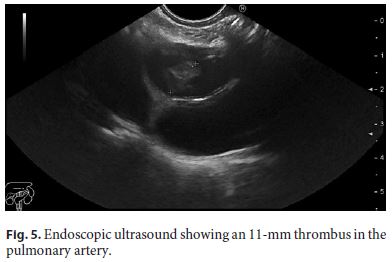
A 72-year-old man was referred for EUS evaluation of a pancreatic mass with hepatic metastasis identified in thoracic-abdominal-pelvic CT. EUS exploration showed a left pulmonary artery 11-mm thrombus (Fig. 5) associated with a multimetastatic liver and uncinated process mass. This finding was later confirmed by CT pulmonary angiography. Cytology was consistent with pancreatic adenocarcinoma.
Discussion
EUS evaluation is not seldom limited to the targeted lesion prior identified in other imaging studies. Vascular thrombus can be an incidental finding on EUS. This is a privileged method for vascular evaluation by its proximity to abdominal and mesenteric vessels. In cancer patients, EUS can diagnose thrombotic events previously unidentified by other imaging methods, such as contrast CT or MRI, with major prognostic and therapeutic implications. Several case reports describe thrombi detection by EUS in cancer patients in various locations, namely the renal vein [7], splenic vein [8], portal vein [9], vena cava [7, 9], and pulmonary artery [10]. Pulmonary embolism, which was the major thrombotic event in our study, remains a potentially fatal disease [11]. If untreated, it has an overall mortality of up to 26% [12]. Anticoagulation reduces mortality and recurrence of pulmonary embolism [13]. All our patients were asymptomatic, and all of them had undergone a prior staging contrast-enhanced CT that missed the thrombotic disease in half of them because of the inadequacy of the CT protocol, which should have been a CT pulmonary angiography. The 2 patients newly diagnosed by EUS promptly initiated anticoagulation after diagnosis confirmation by CT pulmonary angiography, highlighting the role of EUS in the reduction of short-term mortality in these patients. In spite of not being widely used, additionally, intravascular FNA of the thrombus can confirm its malignancy [6]. We emphasize the risk of thromboembolic disease in patients with pancreatic cancer and highlight the importance of performing a CT pulmonary angiography if there is any suspicion of pulmonary embolism. This series underlines the importance of a systematic, station approach EUS technique, namely in the mediastinum, regardless of the clinical indication.
References
1 Ansari D, Ansari D, Andersson R, et al: Pancreatic cancer and thromboembolic disease, 150 years after Trousseau. Hepatobiliary Surg Nutr 2015;4:325–335. [ Links ]
2 Elyamany G, Alzahrani A, Bukhary E: Cancer-associated thrombosis: an overview. Clin Med Insights Oncol 2014;8:129–137. [ Links ]
3 Shah M, Saif M: Pancreatic cancer and thrombosis. J Pancreas 2010;11:331–333. [ Links ]
4 Khorana A, Fine R: Pancreatic cancer and thromboembolic disease. Lancet 2004;5:655–663. [ Links ]
5 Vilmann P: EUS targeting of vascular thrombosis: risky business? Gastrointest Endosc 2017;86:156–160. [ Links ]
6 Rustagi T, Gleeson FC, Chari S, et al: Remote malignant intravascular thrombi: EUSguided FNA diagnosis and impact on cancer staging. Gastrointest Endosc 2017;86:150–155. [ Links ]
7 Mangiavillano B, Arcidiacono PG, Pasta A, et al: Could EUS be useful for evaluating right renal vein and inferior vena cava thrombosis due to renal cell carcinoma? Report of 3 cases. Gastrointest Endosc 2007;66:154–156. [ Links ]
8 Delconte G, Bhoori S, Milione M, et al: Endoscopic ultrasound-guided fine needle aspiration of splenic vein thrombosis: a novel approach to the portal venous system. Endoscopy 2016;48:40–41. [ Links ]
9 Kayar Y, Turkdogan KA, Baysal B, et al: EUSguided FNA of a portal vein thrombus in hepatocellular carcinoma. Pan Afr Med J 2015;21:86. [ Links ]
10 Tee C, Harn C, Segarajasingam D, et al: Pulmonary embolism diagnosed with EUS on a patient with adenocarcinoma of the pancreas. Gastrointest Endosc 2013;78:542–543. [ Links ]
11 Laporte S, Mismetti P, Décousus H, et al: Clinical predictors for fatal pulmonary embolism in 15,520 patients with venous thromboembolism: findings from the Registro Informatizado de la Enfermedad TromboEmbolica venosa (RIETE) Registry. Circulation 2008; 117:1711–1716. [ Links ]
12 Barritt DW, Jordan SC: Anticoagulant drugs in the treatment of pulmonary embolism. A controlled trial. Lancet 1960;18:1309–1312. [ Links ]
13 Smith SB, Geske JB, Maguire JM, et al: Early anticoagulation is associated with reduced mortality for acute pulmonary embolism. Chest 2010;137:1382–1390. [ Links ]
Statement of Ethics
Informed consent was obtained from the patients for publication of their case histories and images.
Disclosure Statement
The authors have no competing interests to declare.
* Corresponding author.
Dr. Catarina Atalaia-Martins
Department of Gastroenterology, Centro Hospitalar Leiria
Rua das Olhalvas
PT–2410-197 Leiria (Portugal)
E-Mail catarinatalaiamartins@gmail.com
Received: November 24, 2017; Accepted after revision: January 18, 2018
Author Contributions
C. Atalaia-Martins designed the study, drafted the article, and is the article guarantor. I. Mocanu and J. Cortêz-Pinto analyzed the data. P. Pinto-Marques designed the study and critically reviewed the article for intellectual content. D. Serra approved the article.














