Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
GE-Portuguese Journal of Gastroenterology
Print version ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.1 Lisboa Feb. 2019
https://doi.org/10.1159/000487277
ENDOSCOPIC SNAPSHOT
LAMS to the SEMS Rescue!
LAMS ao resgate da SEMS!
Inês Pitaa, Diogo Libânioa, Ana Ponteb, Pedro Pimentel-Nunesa, Mário Dinis-Ribeiroa, Pedro Bastosa
aDepartment of Gastroenterology, Portuguese Institute of Oncology Francisco Gentil, Porto, Portugal; bDepartment of Gastroenterology, Centro Hospitalar de Vila Nova de Gaia/Espinho, Vila Nova de Gaia, Portugal
* Corresponding author.
Keywords: Echoendoscopy, Endoscopic retrograde cholangiopancreatography, Endoscopic ultrasoundguided biliary drainage, Choledochoduodenostomy, Biliary obstruction
Palavras-Chave: Ecoendoscopia, Colangiopancreatografia retrograde endoscópica, Drenagem biliar guiada por ecoendoscopia, Coledocoduodenostomia, Obstrução biliar
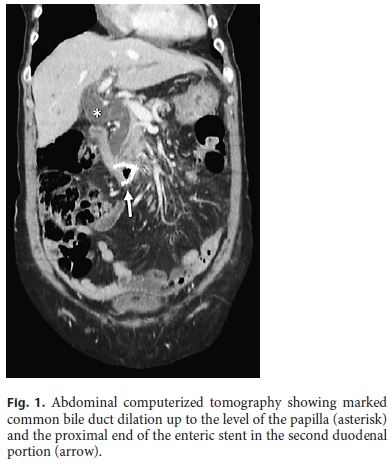
We present the case of an 80-year-old woman with gastric outlet obstruction syndrome due to colorectal cancer metastasis in the distal duodenum. A 9-cm luminal uncovered self-expandable metal stent (SEMS) (Wallstent ®, Boston Scientific, Marlborough, MA, USA) was inserted, with the proximal flange located in D2. The obstructive symptoms resolved but the patient was admitted a week later due to jaundice (total bilirubin 4.07 mg/dL, direct 2.84 mg/dL). Abdominal computerized tomography revealed marked dilation of the common bile duct (CBD) up to the level of the papilla (Fig. 1).
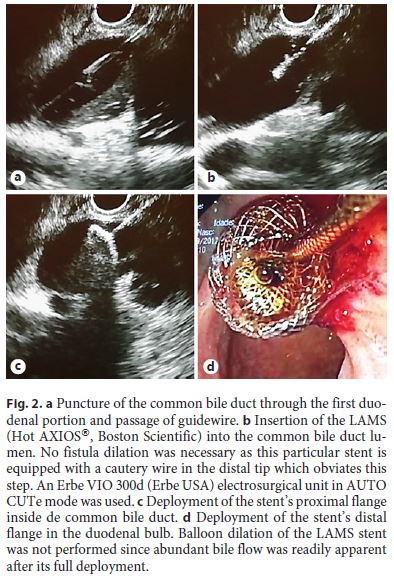
An endoscopic retrograde cholangiopancreatography (ERCP) was scheduled. Anticipating difficulties in accessing the duodenal papilla, an endoscopic ultrasoundguided biliary drainage (EUS-BD) was also planned in advance. As suspected, the metal mesh in the duodenum hindered duodenoscope progression, precluding any attempt at biliary cannulation. Since the duodenal bulb was free, we decided to perform a choledochoduodenostomy using a 6 × 8 mm lumen-apposing metal stent (LAMS) (Hot AXIOS®, Boston Scientific, Marlborough, MA, USA). A therapeutic echoendoscope was advanced to the duodenal bulb and a 19-gauge needle was used to puncture the dilated CBD and aspirate bile. A 0.035-inch guidewire was then inserted into the CBD and the LAMS was deployed following the manufacturer’s instructions (Fig. 2).
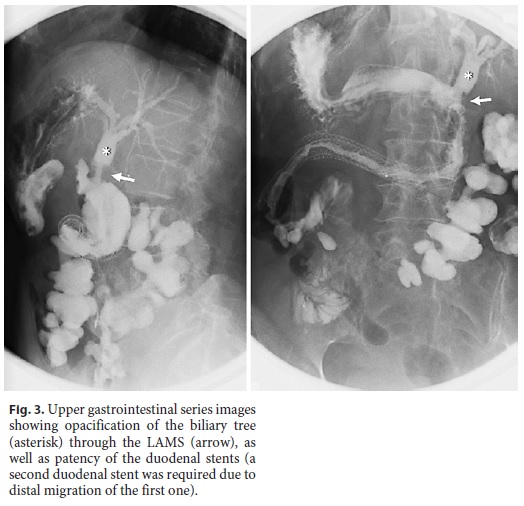
After the procedure, jaundice resolved and the patient was able to resume the palliative chemotherapy prescribed, with no recurrence of obstructive symptoms or jaundice in 4 months of follow-up. Figure 3 shows a predischarge gastroduodenography, revealing patency of the duodenal stents and oral contrast opacifying the biliary tree through the LAMS.
This case highlights biliary obstruction as an uncommon adverse effect of endoscopic SEMS placement. We attributed jaundice to the procedure and not to malignant invasion due to the close temporal association between the two events. The situation was further complicated because the SEMS itself impeded papillary access and ERCP.
EUS-BD has emerged in the last decade as a valid alternative to percutaneous or surgical drainage in cases of ERCP failure or unfeasibility, with success and complication rates of 90 and 19%, respectively [1]. EUS-BD comprises a heterogeneous group of procedures that utilize the echoendoscope for biliary drainage. Access to the biliary tree may be achieved at intra- or extrahepatic sites and drainage can be accomplished through a transmural, antegrade, or rendez-vous method [1].
A recent meta-analysis comparing all EUS-BD techniques with percutaneous transhepatic biliary drainage (PTBD) found similar rates of technical success but better clinical outcomes, a better safety profile, and a lower rate of re-intervention for EUS approaches [2].
There is currently no consensus on the preferred EUSBD method and only recently have decision algorithms been proposed [3, 4]. In general, rendez-vous or antegrade drainage methods have lower success rates and longer procedure times, while transhepatic puncture site has more complications when compared to transduodenal access [1].
Bile leak is the most common complication of EUS-BD [2]. Recently, dedicated LAMS have been used instead of regular metal stents to create a choledochoduodenostomy. These are short, fully covered stents with wide flanges, developed specifically for EUS-guided drainage. This particular type of stent may reduce the risk of biliary leak and tends to make the procedure simpler and faster. A recent multicenter series of 57 choledochoduodenostomies in malignant biliary obstruction using AXIOS® or Hot AXIOS® stents reported excellent technical (98.2%) and clinical (94.7%) success rates, with re-intervention rates of 9.3% during a mean follow-up of 151 days. All reinterventions were endoscopic and biliary drainage was maintained through the LAMS [5].
EUS-BD, when performed by an experienced echoendoscopist, should be preferred to PTBD in malignant biliary obstruction after ERCP failure, and may become the first-line drainage procedure in the near future [4].
References
1 Dhir V, Isayama H, Itoi T, et al: Endoscopic ultrasonography-guided biliary and pancreatic duct interventions. Dig Endosc 2017;29:472–485. [ Links ]
2 Sharaiha RZ, Khan MA, Kamal F, et al: Efficacy and safety of EUS-guided biliary drainage in comparison with percutaneous biliary drainage when ERCP fails: a systematic review and meta-analysis. Gastrointest Endosc 2017;85:904–914. [ Links ]
3 Tyberg A, Desai AP, Kumta NA, et al: EUSguided biliary drainage after failed ERCP: a novel algorithm individualized based on patient anatomy. Gastrointest Endosc 2016;84:941–946. [ Links ]
4 Hara K, Yamao K, Mizuno N, et al: Endoscopic ultrasonography-guided biliary drainage: Who, when, which, and how? World J Gastroenterol 2016;22:1297–1303. [ Links ]
5 Kunda R, Perez-Miranda M, Will U, et al: EUS-guided choledochoduodenostomy for malignant distal biliary obstruction using a lumen-apposing fully covered metal stent after failed ERCP. Surg Endosc 2016;30:5002–5008. [ Links ]
Disclosure Statement
The authors have no conflicts of interest to declare.
* Corresponding author.
Dr. Inês Pita
Department of Gastroenterology, Portuguese Institute of Oncology Francisco Gentil
Rua Dr. António Bernardino de Almeida
PT–4200-072 Porto (Portugal)
E-Mail neispita@hotmail.com
Received: January 2, 2018; Accepted after revision: January 27, 2018














