Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.1 Lisboa fev. 2019
https://doi.org/10.1159/000487276
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
Megaesophagus in a Patient with Achalasia
Megaesófago numa Doente com Acalásia
João Pinto, Flávio Pereira, António Banhudo
Gastroenterology Department, Amato Lusitano Hospital, Castelo Branco, Portugal
* Corresponding author.
Keywords: Esophageal achalasia, Esophageal motility disorders,·Megaesophagus, Radiography
Palavras-Chave: Acalásia esofágica, Perturbações motoras do esófago,·Megaesófago, Radiografia
A 84-year-old female with a history of achalasia presented to the emergency department with worsening dysphagia for solids and liquids, regurgitation, and substernal chest pain after meals for the previous 48 h. The real onset of dysphagia had been 40 years before, but due to her resiliency regarding symptoms, the diagnosis of achalasia was established only at 72 years of age. Then, she rejected surgery and thus received 4 treatments with botulinum toxin after an equal number of episodes of food impaction and was medicated with nifedipine. The patient had developed strategies to circumvent dysphagia and maintained a good nutritional status, seeking medical care only in case of complete esophageal obstruction such as in this episode.
On physical examination, she presented good general status, was afebrile and hemodynamically stable with peripheral oxygen saturation of 92% while breathing ambient air. Thoracic auscultation revealed decreased vesicular breath sounds in the upper right hemithorax. Blood tests were unremarkable except for mild elevation of the inflammatory markers.
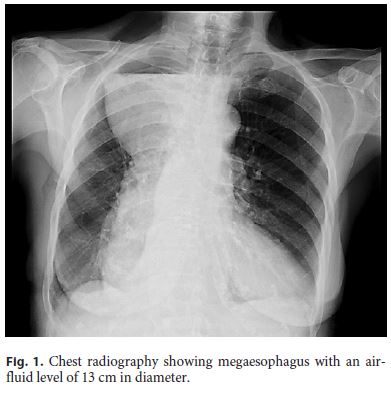
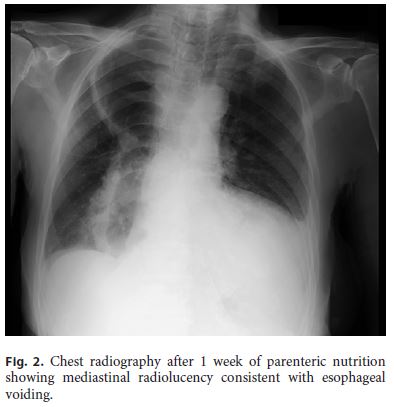
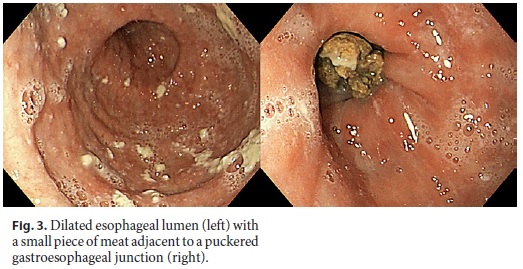
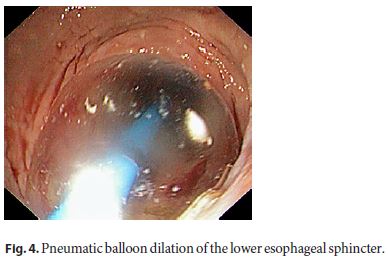
A chest radiography revealed an air-fluid level of 13 cm in diameter, occupying the whole apex of the right hemithorax, actually being the most superior segment of a diffusely enlarged mediastinum (Fig. 1). These findings were consistent with a megaesophagus filled with food in the context of protracted achalasia [1–3]. After 1 week of fasting with parenteral feeding, radiological re-evaluation demonstrated mediastinal radiolucency compatible with complete esophageal voiding (Fig. 2). Upper gastrointestinal endoscopy showed a dilated and tortuous esophageal lumen with colon-like morphology; a small piece of meat was identified adjacent to a puckered gastroesophageal junction (Fig. 3) and removed using a net. With the consent of the patient and aspiring a more durable treatment with disruption of the lower esophageal sphincter [3–5], endoscopic balloon dilation until 30 mm was performed uneventfully (Fig. 4). After 2 years, the patient still maintains some dietary restrictions but presents a good nutritional status, has had no episodes of regurgitation, and is generally satisfied with her quality of life.
Achalasia is a primary motility disorder of the esophagus characterized by insufficient relaxation of the lower esophageal sphincter and absence of esophageal peristalsis [3, 5]. Patients usually present with slowly progressive dysphagia for solids and liquids, regurgitation, weight loss, and occasionally retrosternal chest pain [2, 3]. The findings of an aperistaltic and dilated esophagus with retained saliva or undigested food and minimal opening of the lower esophageal sphincter or “bird-beak” appearance on endoscopic and radiological studies suggest the diagnosis that is confirmed by esophageal manometry [5].
A more definitive treatment requires disrupting the lower esophageal sphincter through endoscopic pneumatic balloon dilation, surgery or per-oral endoscopic myotomy [3–5]. Botulinum toxin injection usually has a temporary effect, being used in patients who are not good candidates for definitive therapies [3, 5]. Oral pharmacological therapies (e.g., nifedipine) are reserved for patients unfit or unwilling to undergo definitive therapies [5].
In patients with longstanding achalasia left untreated or managed with non-definitive approaches, progressive dilation occurs, producing a megaesophagus morphology. In such cases, the organ becomes an inert food reservoir and massive food impaction can develop [1, 2].
References
1 Liang C-Y, Lin M-S: Achalasia. N Engl J Med 2009;360:801. [ Links ]
2 Okwara C, Cangemi D: Achalasia with megaesophagus. N Engl J Med 2015;373:25. [ Links ]
3 Stavropoulos S, Friedel D, Modayil R, Parkman H: Diagnosis and management of esophageal achalasia. BMJ 2016;354:i2785. [ Links ]
4 Moonen A, Annese V, Belmans A, et al: Longterm results of the European achalasia trial: a multicentre randomised controlled trial comparing pneumatic dilation versus laparoscopic Heller myotomy. Gut 2016;75:732–739. [ Links ]
5 Vaezi M, Pandolfino J, Vela M: ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol 2013;108:1238–1249. [ Links ]
Statement of Ethics
This study did not require informed consent or review/approval by the appropriate ethics committee.
Disclosure Statement
The authors have no conflicts of interest to declare.
* Corresponding author.
Dr. João Pinto
Gastroenterology Department, Amato Lusitano Hospital
Avenida Pedro Álvares Cabral
PT–6000-085 Castelo Branco (Portugal)
E-Mail jsdiaspinto@gmail.com
Received: December 4, 2017; Accepted after revision: January 27, 2018














