Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
GE-Portuguese Journal of Gastroenterology
Print version ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.2 Lisboa Apr. 2019
https://doi.org/10.1159/000489721
CLINICAL CASE STUDY
Biliary Peritonitis due to a Ruptured Amebic Liver Abscess Mimicking a Periampullary Tumor and Liver Metastases with the Elevation of CA 19-9 and CA 125: A Case Report
Peritonite biliar devido a rotura de um abcesso amebiano que mimetizava um tumor periampular com metastização hepática e elevação do CA 19–9 e do CA 125: um caso clínico
Javiera Marin-Leivaa, Antoine Jeri-Yabara, Wendy Hernandez Fernandeza, Edwin Damian Bellob
aSchool of Medicine, Universidad Peruana de Ciencias Aplicadas, Lima, Peru; bDepartment of Surgery, Hospital Nacional Dos de Mayo, Lima, Peru
* Corresponding author.
ABSTRACT
Introduction: An amebic liver abscess is the most common presentation of extraintestinal amebiasis. This condition is the result of a parasite infection caused by Entamoeba histolytica. Materials and Methods: We report a case of a 53-yearold male who presented with abdominal pain in the right upper quadrant, jaundice, and a 10-kg weight loss within a 1-month span. Results and Conclusion: A wide range of symptoms and findings in the imaging tests suggestive of neoplasia, elevated levels of CA 19-9 and CA 125, and the presentation of biliary peritonitis as a complication makes this case a challenge for its approach and management.
Keywords: Amebic liver abscess, CA 19-9, CA 125
RESUMO
Introdução: O abcesso amebiano é a apresentação mais comum da amebíase extraintestinal. Esta condição é resultado da infeção pelo parasita Entamoeba histolytica. Materiais e Métodos: Reportamos um caso clínico de um homem de 53 anos com dor abdominal no quadrante superior direito, icterícia e emagrecimento de 10 kg em 1 mês. Resultados e Conclusões: Os sintomas e os achados imagiológicos sugestivos de neoplasia, os níveis elevados de CA 19-9 e CA 125 e a apresentação como peritonite biliar tornam este caso um desafio de diagnóstico e abordagem clínica.
Palavras-Chave: Abcesso hepático amebiano, CA 19-9, CA 125
Introduction
Amebiasis is caused by the protozoan Enatamoeba histolytica. Most infections are asymptomatic; there are 2 different clinical manifestations, amebic dysentery and extraintestinal disease [1]. The amebic liver abscess (ALA) is the most common extraintestinal manifestation of amebiasis, in which the E. histolytica establishes an infection in the liver by ascending through the portal venous system [2, 3]. This type of presentation is 7–10 times more frequent in adult males compared with other demographic groups and it is most commonly observed in the fourth and fifth decade of life [4]. The countries with the highest rates of amebiasis are India, Africa, Mexico, Central and South America [2].
Approximately 80% of the patients will develop symptoms in a 2-to-4-week period after infection; the most common symptoms are fever and abdominal pain in the right upper quadrant. The rupture of the ALA can occur in any contiguous space or organ. It has been reported that in up to 7% of the cases, the abscess bursts inside the peritoneum, causing peritonitis [5]. The diagnosis is based on the clinical presentation and epidemiology with concomitant radiographic studies and serologic tests. Efficient treatment includes the use of metronidazole followed by a luminal agent such as paramomycin [2].
Herein, we present a case of extraintestinal amebiasis in a 53-year-old male, originally from Ica, Peru, living in Lima, Peru, at the moment of infection.
Case Presentation
A 53-year-old male with no past medical history presented abdominal pain, nausea, jaundice, and weight loss 1 month prior to his hospital entry. The patient had an 8 out of 10 diffuse abdominal pain that was not localized and described as colic in nature. This pain was accompanied by nausea and anorexia, which lead to a 10-kg weight loss within a 1-month span. The patient described a sensation of high temperature, but it was never quantified. Upon further inquiry, the patient mentioned that he had noticed that his urine had turned brown. According to his past medical history, the patient denied having any disease or past surgeries. Family history does not include cancer. The patient worked as a peddler and lived in Lima, Peru. According to the patient, his food choices were balanced, but sometimes he had to eat street food because of the demands of his job.
Upon examination, the patient was a middle-aged male of the appropriately stated age. The patient seemed malnourished and in a state of cachexia. His vital signs were: blood pressure of 120/80 mm Hg, a temperature of 38 °C, a pulse of 88 bpm, and a rate of 18 breathes per minute. The abdomen was visually distended and tender to superficial and deep palpation. Active bowel sounds were present on auscultation (tympanic percussion on the 4 quadrants of the abdomen). The rest of the examination did not show intercurrences.
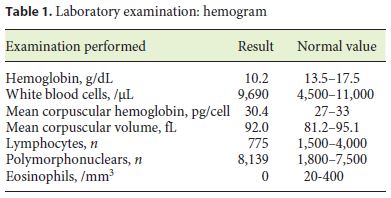
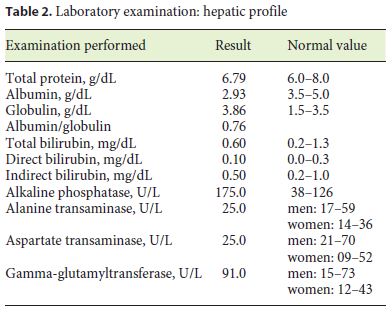
A complete blood count, urinalysis, hepatic laboratory tests, and computed tomography (CT) scan of the abdomen were ordered. The urinalysis showed a severe leukocyturia, hence why the first diagnosis made was a complicated urinary tract infection. The patient was admitted and treatment was given, but the symptoms were still increasing in intensity (Tables 1, 2).
The CT scan suggested the presence of a tumor of 7.7 cm in diameter on the left hepatic lobule, suggestive of hepatic cancer; it also showed multiple small nodular appearances on the liver. The CT also suggested a left pleural effusion and ascites with the presence of multiple intra-abdominal cysts that were reported as possible peritoneal pseudomyxomas. The intrahepatic biliary conducts were increased in size, as well as the choledocus (15 mm), because of a distal obstruction caused by an intraluminal infiltrative mass. The gallbladder was distended (Fig. 1a, b).
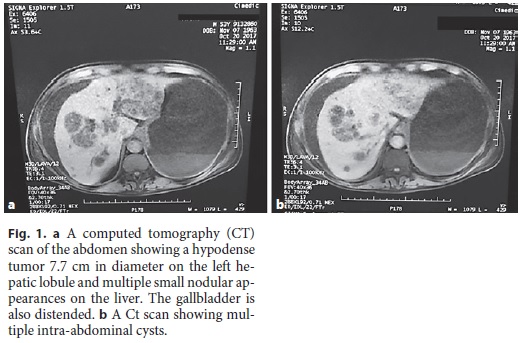
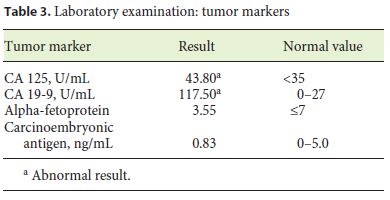
Upon the abnormal CT scan, tumor markers were ordered, andCA 19-9 and CA 125 results were abnormal. Furthermore, an endoscopic retrograde cholangiopancreatography (ERCP) was scheduled (Table 3).
Before an ERCP could be done, the patient entered the operating room since he had developed an acute cholangitis and septic shock. The preoperatory diagnosis was acute cholangitis and possible periampullary neoplasm, but when the doctors in charge performed an exploratory laparotomy, the correct diagnosis became biliary peritonitis from an abscessed hepatic mass. During the operation, about 2 L of purulent bile was collected. The doctors also performed a peritoneal cavity lavage, cholecystectomy, biliary duct exploration, and a hepatic biopsy, leaving behind a percutaneous biliary drainage (Kehr). The hepatic biopsy showed amoebic trophozoites.
After the operation and antibiotic treatment, the patient evolved well. A control MRI was done before the patient left, which showed a subtraction image on the common bile duct which is why the ERCP was finally performed to rule out the minimal possibility of a periampullary neoplasm. The biopsy came back negative.
Discussion
The most common manifestation of extraintestinal amebiasis is an ALA. Extraintestinal amebiasis, especially amoebic liver abscess, is most commonly seen in patients aged between 20–40 years [6]. The most common clinical picture of ALA is fever, weight loss, and right upper quadrant abdominal pain; although, in some cases it is possible that patients present with hepatomegaly, jaundice (4%), and weight loss (29%) [7]. Furthermore, most patients have symptoms for < 13 days; the patient reported herein had the symptoms for about a month [8].
Various laboratory examination abnormalities were observed in patients with ALA, the most consistent being leukocytosis, while the liver aminotransferase, alkaline phosphatase, and bilirubin levels were within the normal range [8]. Our patient did not have leukocytosis but did have abnormal levels of liver aminotransferases and bilirubin.
The rupture of an ALA is a frequent complication of hepatic amebiasis, which can lead to peritonitis, pleural and pericardial involvement, and gastric rupture [9]. In the case reported, there were complications such as biliary peritonitis because of an initial misdiagnosis of a possible periampullary tumor and possible hepatic metastases since the CT scan showed possible infiltrations of the liver, peritoneum, and biliary conducts, which turned out to be bile from the ruptured ALA. There were several signs and symptoms, which suggested that the patient had a periampullary tumor, such as losing 10 kilograms in < 1 month, jaundice, diffuse abdominal pain, and loss of appetite; abnormal tumor marker values such as CA 19-9 and CA125 also sustained this possible diagnosis.
CA 19-9 is a very sensitive marker for pancreatic, gastric, and hepatobiliary malignancies. In their study, Pavai and Yap [10] found that this tumor marker was elevated mostly in malignancies of the pancreas, colorectum, lung, liver, and ovary, and less frequently in cases of non-malignant causes such as hepatobiliary system disease, pneumonia, pleural effusion, renal failure, and systemic lupus erythematosus. An increase in CA 19-9 of > 40 U/mL is rare in patients with benign diseases [11]; our patient had a value of 117.50 U/mL, which made the possibility of a benign disease to be the cause unlikely. This antigen can also be highly elevated in acute cholangitis with levels up to 192 U/mL, or less commonly in a liver abscess as in our patient, but only a few case reports have been found [10, 12].
CA 125 is a tumor marker for ovarian cancer and has also been found increased in peritoneal tuberculosis [13]. To our knowledge, an elevated CA 125 has only been reported once in a patient that was mistaken to have a livertumor and instead was diagnosed with a ruptured ALA. This is not a typical occurrence of the disease, but in our patient, a slight increase of this tumor marker was found, with a value of 43.80 U/mL when the normal range stated is < 35 U/mL [11]. This second report could spark an investigation as to why CA 125 would elevate in ALAs.
Conclusion
This case report reveals the troublesome task of diagnosing a ruptured ALA, since the list of differential diagnoses for the signs and symptoms presented is lengthy. In addition, this case shows that the elevation of CA 19-9 and CA 125 can occur in amebic abscesses and biliary peritonitis.
References
1 Haque R, Huston CD, Hughes M, Houpt E, Petri WA Jr: Amebiasis. N Engl J Med 2003;348:1565–1573. [ Links ]
2 Prakash V, Bhimji SS: Abscess, amebic liver (Updated May 15, 2017); in StatPearls (Internet). Treasure Island, StatPearls Publishing, 2017. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430832. [ Links ]
3 Aikat BK, Bhusnurmath SR, Pal AK, Chhuttani PN, Datta DV: The pathology and pathogenesis of fatal hepatic amoebiasis – a study based on 79 autopsy cases. Trans R Soc Trop Med Hyg 1979;73:188. [ Links ]
4 Maltz G, Knauer CM: Amebic liver abscess: a 15-year experience. Am J Gastroenterol 1991;86:704. [ Links ]
5 Adams EB, MacLeod IN: Invasive amebiasis. I. Amebic dysentery and its complications. Medicine (Baltimore) 1977;56:315. [ Links ]
6 Nordestgaard AG, Stapleford L, Worthen N, et al: Contemporary management of amebic liver abscess. Am Surg 1992;58:315–320. [ Links ]
7 Seeto RK, Rockey DC: Amebic liver abscess: epidemiology, clinical features and outcome. West J Med 1999;170:104–109. [ Links ]
8 Hoffner R, et al: Common presentations of amebic liver abscess. Ann Emerg Med 1999;34:351–355. [ Links ]
9 Suchitra R, et al: Hepatic amebiasis: a reminder of the complications. Curr Opin Pediatr 2010;21:145–149. [ Links ]
10 Pavai S, Yap SF: The clinical significance of elevated levels of serum CA 19–9. Med J Malaysia 2003;58:667–672. [ Links ]
11 Kopanakis N, et al: Elevated levels of CA 19–9 and CA 125 in an amoebic cyst mimicking liver cancer. Hellenic J Surg 2011;83:210. [ Links ]
12 Yoshino Y, et al: Liver abscess with a markedly high level of carbohydrate antigen 19–9. Gastroenterology Res 2012;5:205–207. [ Links ]
13 Bilgin T, Karabay A, Dolar E, Develioglu O: Peritoneal tuberculosis with pelvic abdominal mass, ascites and elevated CA 125 mimicking advanced ovarian carcinoma: a series of 10 cases. Int J Gynecol Cancer 2001;11:290–294. [ Links ]
Statement of Ethics
This study did not require informed consent nor review/approval by the appropriate ethics committee.
Disclosure Statement
The authors report no conflicts of interest.
* Corresponding author.
Antoine Jeri-Yabar
School of Medicine, Universidad Peruana de Ciencias Aplicadas
Av. Alameda Sur
Chorillos, Lima 9 (Peru)
E-Mail Antoine_jeri@hotmail.com
Received: February 24, 2018; Accepted after revision: April 21, 2018














