Services on Demand
Journal
Article
Indicators
Related links
Share
GE-Portuguese Journal of Gastroenterology
Print version ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.2 Lisboa Apr. 2019
https://doi.org/10.1159/000487962
ENDOSCOPIC SNAPSHOT
Rectovaginal Septum Nodule: The Key for an Unexpected Diagnosis
Nódulo do Septo Rectovaginal: A Chave para um Diagnóstico Inesperado
Marco Silvaa, Pedro Moutinho-Ribeiroa, Vítor Magno-Pereirab, Filipe Vilas-Boasa, Guilherme Macedoa
aDepartment of Gastroenterology, Centro Hospitalar de São João, Porto Medical School, Porto, Portugal; bDepartment of Gastroenterology, Centro Hospitalar do Funchal, Funchal, Portugal
* Corresponding author.
Keywords: Anal cancer, Metastasis, Endoscopic ultrasound-guided fine-needle aspiration
Palavras-Chave: Cancro anal, Metástase, Aspiração por agulha fina ultrassonográfica
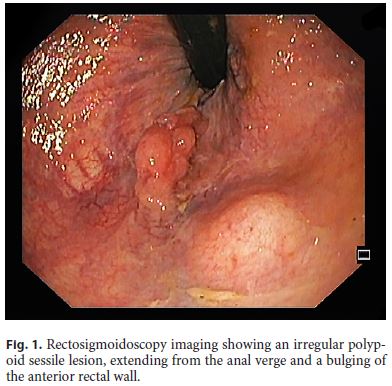
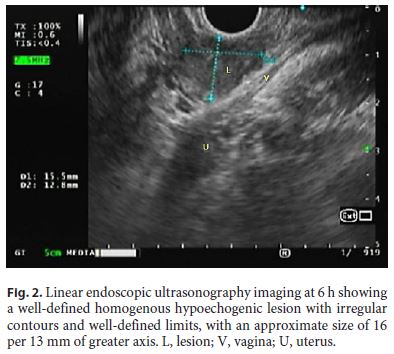
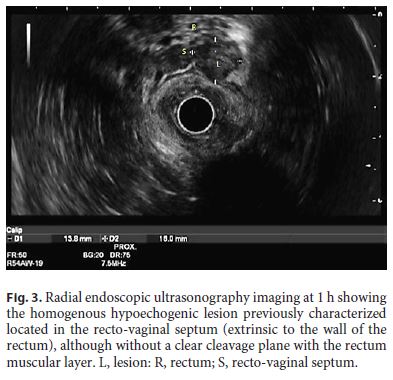
We report the case of a 54-year-old female with a 2-year history of hypertrophic cranial pachymeningitis (medicated with prednisolone 5 mg and pregabalin), a cranioencephalic traumatic accident in childhood (with a period in coma), and no other relevant medical history including immunosuppressive pathology as HIV. A Gallium-67 scintigraphy was performed for etiological evaluation, which revealed a vaginal uptake. With the exception of neurological symptoms, she had no other complaints and denied all risk factors for anal cancer. On digital rectal examination, a smooth, irregular nodule measuring 15 mm was palpated. An endovaginal ultrasonography revealed a solid mass of the rectovaginal septum in close contact with the anterior wall of the rectum, suggesting the possibility of a nodule of endometriosis. Flexible rectosigmoidoscopy was then performed and a bulging of the lower rectal wall covered by normal mucosa 15 mm in diameter was found, corresponding to the described lesion. Furthermore, during the retroflexion maneuver for complete observation of the distal rectum and anal canal, an irregular sessile polypoid lesion was found, extending from the anal verge (Fig. 1). Biopsies were taken and were consistent with a squamous cell anal carcinoma. Radial endoscopic ultrasound (EUS) was first performed to evaluate the extraluminal nodule. It corresponded to a rounded, homogenous, hypoechogenic lesion, with regular contours and well-defined borders, located in the recto-vaginal septum (extrinsic to the rectal wall) (Fig. 2, 3). No perilesional lymph nodes were detected. EUS fine-needle aspiration (22-G needle) through linear EUS was then performed and the cytological diagnosis was a metastasis of the squamous cell anal carcinoma.
The patient was discussed in a multidisciplinary oncological meeting and proposed for radiochemotherapy. Follow-up at 3 months revealed a good tolerance except for limited oral mucositis, pending radiological evaluation of therapy response.
Extensive evaluation including brain magnetic resonance imaging excluded signs of carcinomatous meningitis. The final diagnosis was metastatic squamous cell anal carcinoma and idiopathic hypertrophic cranial pachymeningitis cortico-responsive of probable fibrocicatricial nature. In fact, to date, there have been no other reports of an association of these two diagnoses.
Squamous cell carcinoma of the anus is a relatively rare malignancy, accounting for less than 2% of gastrointestinal cancers [1]. The median age of diagnosis is 60 years and there is a slightly higher incidence in women [2]. However, its incidence has been increasing, especially in certain populations with high-risk behavior and in those with HIV [3]. Metastatic presentation accounts for only 10–20% of cases, and patients usually have a poor prognosis, with 5-year median overall survival rates of 10% in men and 20% in women [3, 4]. A high index of suspicion and knowledge of the relevant anatomy and pathophysiology are essential to avoid misdiagnosis and provide proper management. On the other hand, cancer of the recto-vaginal septum is an extremely rare entity and in most cases it is associated with endometriosis foci [5]. In the literature, only 2 cases of fallopian tube cancer in this location have been reported [5]. To the best of our knowledge, this is the first report of a metastatic spread of squamous cell anal carcinoma to the recto-vaginal septum.
References
1 Elorza G, Saralegui Y, Enríquez-Navascués Jm, Placer C, Velaz L: Anal intraepitelial neoplasia: a narrative review. Rev Esp Enferm Dig 2016;108:31–39. [ Links ]
2 Osborne MC, Maykel J, Steele SR: Anal squamous cell carcinoma: an evolution in disease and management. World J Gastroenterol 2014;20:13052–13059. [ Links ]
3 Dewdney A, Rao S: Metastatic squamous cell carcinoma of the anus: time for a shift in the treatment paradigm? ISRN Oncol 2012;2012:756591. [ Links ]
4 Glynne-Jones R, Nilsson Pj, Aschele C, Goh V, Peiffert D, Cervantes A, et al: Anal cancer: ESMO-ESSO-ESTRO clinical practice guidelines for diagnosis, treatment and follow-up. Eur J Surg Oncol 2014;40:1165–1176. [ Links ]
5 Lopez N, Grabowski J, De Santiago J, Zapardiel I: Carcinoma of the recto-vaginal septum. comprehensive literature review. J Obstet Gynaecol 2016;36:450–454. [ Links ]
Statement of Ethics
All rules of the local ethics committee (“Comissão de Ética para a Saúde do Centro Hospitalar São João/Faculdade de Medicina da Universidade do Porto”) were followed, preserving patient identity and confidentiality.
Disclosure Statement
The authors declare that they have no conflict of interest.
Funding Sources
The authors declare that there was no source of founding.
* Corresponding author.
Dr. Marco Silva
Department of Gastroenterology, Centro Hospitalar de São João Alameda
Professor Hernâni Monteiro PT–4200-319 Porto (Portugal)
E-Mail marcocostasilva87@gmail.com
Received: November 19, 2017; Accepted after revision: February 23, 2018
Author Contributions
M.S.: responsible for the collection and interpretation data and drafting of the manuscript. P.M.-R.: performed endoscopic ultrasonography; critical revision of the manuscript. V.M.-R.: responsible for the data collection and drafting of the manuscript. F.V.-B.: performed endoscopic ultrasonography and rectosigmoidoscopy; critical revision of the manuscript. G.M.: critical revision of the manuscript, final approval of the paper.














