Services on Demand
Journal
Article
Indicators
Related links
Share
GE-Portuguese Journal of Gastroenterology
Print version ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.4 Lisboa Aug. 2019
https://doi.org/10.1159/000494279
ENDOSCOPIC SNAPSHOT
Endoscopic Extraction of a Retained Surgical Drain after Esophagectomy
Extracção endoscópica de dreno cirúrgico retido após esofagectomia
Rui Moraisa, Marco Silvaa, Andreia Albuquerqueb, Filipe Vilas-Boasa, Pedro Pereiraa, Guilherme Macedoa
aGastroenterology Department – Centro Hospitalar de São João, Porto, Portugal; bHomerton University Hospital, London, UK
* Corresponding author.
Keywords: Retained surgical item, Surgical drain, Endoscopy
Palavras-Chave: Itens cirúrgicos retidos, Dreno cirúrgico, Endoscopia
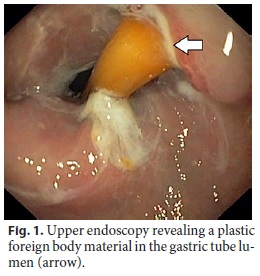
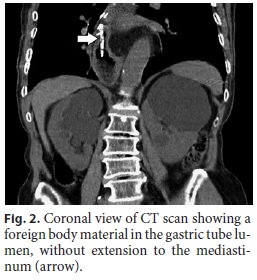
A 77-year-old woman with arterial hypertension and dyslipidemia reported progressive dysphagia. An upper endoscopy was performed and revealed an adenocarcinoma of the gastro-esophageal junction (Siewert type II). Computed tomography (CT) confirmed the presence of a lesion in the cardia with esophageal extension and identified celiac lymphadenopathy. She initially underwent esophageal stent placement and neoadjuvant chemotherapy. CT was repeated with no evidence of the lymphadenopathy and regression of the tumoral mass. After multidisciplinary discussion, the patient was submitted to an Ivor-Lewis esophagectomy. The patient remained asymptomatic and 12 months after the procedure, she was referred for a follow-up upper endoscopy. This exam revealed a plastic foreign body in the gastric tube lumen, partially penetrating the wall, compatible with a surgical drain (Fig. 1). The patient denied dysphagia, dyspnea, chest pain, or other symptoms. The physical exam was unremarkable. She underwent a thoracoabdominal CT scan that confirmed the presence of a tubular structure in the intrathoracic portion of the gastric tube, with approximately 5 cm in length, attached to the surgical suture by a metal clip, without extension to the mediastinum (Fig. 2). In this case, it is possible that during the anastomosis confection by the circular suturing machine, there was a section of a surgical drain that remained attached to the surgical suture of the gastric tube. Considering that there was no evidence of esophageal perforation and the risk of surgery due to the patients age and comorbidities, it was decided, after multidisciplinary discussion, to try to remove the surgical drain endoscopically. Upper endoscopy was then repeated and the surgical drain was removed with grasping forceps and retrieved using a snare (Fig. 3a). Gastric tube mucosa was carefully inspected revealing a congestive mucosa and self-limited bleeding in the place where the drain was previously attached, but without apparent major mucosal defects (Fig. 3b). Contrast instillation was subsequently performed, with no leakage in the fluoroscopic control. Since there was no radiographic or clinical evidence of perforation, no antibiotics were prescribed and the patient was discharged home the same day. On the follow-up, she remained asymptomatic, without evidence of complications.
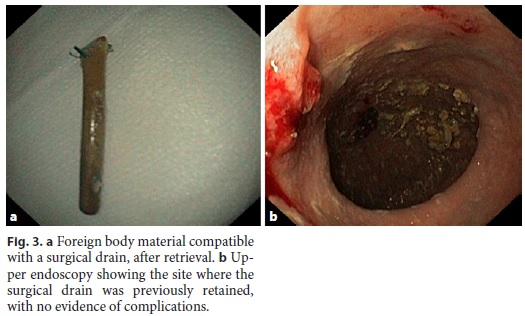
Although the incidence is unknown, it is estimated that retained surgical items (RSIs) occur in 1 of 1,000 to 1,500 abdominal operations and approximately in 1 in every 8,000 to 18,000 of all inpatient operations [1, 2]. Surgical sponges are the most commonly described RSIs [3]. RSIs frequently cause no symptoms but may cause severe complications [4], so they should be removed. In most cases, a surgical re-exploration is performed. However, there are scarce reports of endoscopic removal of RSIs [5]. To our knowledge, this is the first report of the endoscopic retrieval of a retained surgical drain. An additional safety measure could be the use of drains with markings in its extremities and checking it at the end of surgery. Nevertheless, this case highlights the potential role of endoscopy as a minimally invasive, safe, and effective method in selected cases of RSIs, being a reasonable alternative to open surgery.
References
1 Hyslop JW, Maull KI. Natural history of the retained surgical sponge. South Med J 1982;75:657e660. [ Links ]
2 Patterson P. Preventing retained surgical items: what role does technology play? OR Manager 2009;25(1):8e11. [ Links ]
3 Hempel S, Maggard-Gibbons M, Nguyen DK, Dawes AJ, Miake-Lye I, Beroes JM, et al. Wrong-site surgery, retained surgical items, and surgical fires: a systematic review of surgical never events. JAMA Surg. 2015 Aug;150(8): 96–805. [ Links ]
4 Wells HA Jr, Hyun BH, Mitchell RE Jr. A retained surgical sponge with interesting sequela. Am J Med. 1963 Sep;35(3):423–6. [ Links ]
5 Albuquerque A, Rodrigues S, Macedo G. Video of the Month: The Colonic Tug of War: Removal of a Retained Surgical Item. Am J Gastroenterol. 2016 Feb;11(2):174. [ Links ]
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors have no conflicts of interest to disclose.
* Corresponding author.
Rui Morais
Gastroenterology Department, Hospital de São João
Alameda Professor Hernâni Monteiro
PT–4200-319 Porto (Portugal)
E-Mail ruimorais20@gmail.com
Received: July 27, 2018; Accepted after revision: September 28, 2018
Rui Morais and Marco Silva contributed equally to this work.














