Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.6 Lisboa dez. 2019
https://doi.org/10.1159/000496943
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
Double Trouble: Spontaneous Duodenal Hematoma of Pancreatic Origin
Duplo Problema: Hematoma Duodenal Espontâneo de Origem Pancreática
Luísa Martins Figueiredo, David Valadas Horta, Jorge A. Reis
Gastroenterology Department, Hospital Professor Doutor Fernando Fonseca, Amadora, Portugal
* Corresponding author.
Keywords: Duodenal hematoma, Acute pancreatitis, Gastric outlet obstruction
Palavras-Chave: Hematoma duodenal, Pancreatite aguda, Obstrução da saída gástrica
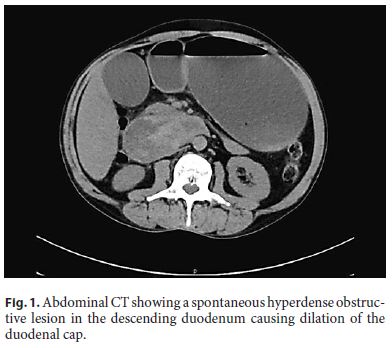
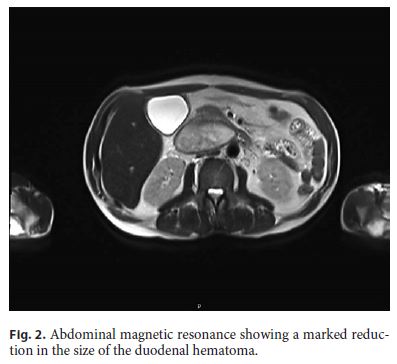
A 55-year-old alcohol-dependent man presented to the hospital for a 6-day history of epigastric pain radiating to the back, associated with nausea and uncontrollable vomiting. He denied any known coagulation disorder, recent abdominal trauma, or endoscopic/surgical intervention. Physical examination revealed scleral icterus, abdominal distention, and epigastric tenderness. Investigation identified hyperamylasemia (441 IU/L), high creatinine (6.02 mg/dL), and total serum bilirubin (2.89 mg/dL). Abdominal computed tomography (CT) performed without intravenous contrast enhancement showed duodenal distension with spontaneously hyperdense obstructive lesion in the descending duodenum and changes suggesting the presence of acute pancreatitis (Fig. 1). This was suggestive of an obstructive intramural duodenal hematoma (IDH) in the descending duodenum. A nasogastric decompression was performed, and the patient was kept on nil by mouth and treated with intravenous fluid hydration, parenteral nutrition, and proton pump inhibitor. The patient improved with remission of abdominal pain and vomiting as well as recovery of renal function. Three weeks later, abdominal magnetic resonance imaging demonstrated a marked reduction in the size of the IDH (Fig. 2).
Spontaneous IDHs of pancreatic origin are rare. IDH was first described by McLauchlan in 1838 [1, 2]. The reason why the duodenum is rarely involved in spontaneous intramural small bowel hematoma remains unclear. Since the duodenum is the shortest part of the small intestine and is fixed and compressed by surrounding extraluminal organs, a duodenal intramural hematoma may be more easily absorbed compared to those in the jejunum or ileum [3].
IDH usually occurs secondary to blunt abdominal injury, but spontaneous nontraumatic cases have been linked to coagulopathy, coagulating drugs, and endoscopic procedures [1, 2, 4]. However, there are many reports regarding the association of IHD with acute pancreatitis and pancreatic malignancy [2].
In general, CT is the imaging choice for diagnosis of spontaneous intramural small bowel hematoma [2]. Reassessment of the status of the hematoma is generally recommended in 2 weeks following diagnosis and conservative management [2, 4]. Conservative management constituted bowel rest, continuous nasogastric decompression, parenteral nutrition, blood transfusion, and correction of coagulopathy when needed. Surgical intervention is only indicated if there is significant intraluminal hemorrhage, bowel perforation, or an identifiable risk of ischemia [2, 4].
Both short-term and long-term outcomes are important in the absence of any other concurrent condition [4]. We presented a rare case of a giant IDH of pancreatic origin complicated with gastric outlet obstruction solved with conservative therapy.
References
1 Eurboonyanun C, Somsap K, Ruangwannasak S, et al. Spontaneous intramural duodenal hematoma: pancreatitis, obstructive jaundice, and upper intestinal obstruction. Case Rep Surg. 2016;2016:5321081. [ Links ]
2 Eichele DD, Ross M, Tang P, Hutchins GF, Mailliard M. Spontaneous intramural duodenal hematoma in type 2B von Willebrand disease. World J Gastroenterol. 2013 Nov;19(41):7205–8. [ Links ]
3 Kang EA, Han SJ, Chun J, Lee HJ, Chung H, Im JP, et al. Clinical features and outcomes in spontaneous intramural small bowel hematoma: cohort study and literature review. Intest Res. 2018. https://doi.org/10.5217/ir.2018.00085. [ Links ]
4 Bayraktar A, Ercan LD, Bakkaloğlu H, Gök AF, İlhan M, Aydın AE. Duodenal intramural hematoma due to early postoperative anticoagulant treatment after a renal transplant: A case report. Ulus Travma Acil Cerrahi Derg. 2018 Nov;24(6):594–6. [ Links ]
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors have no conflicts of interest to declare.
* Corresponding author.
Maria Luísa Martins Figueiredo
Gastroenterology Department
Hospital Professor Doutor Fernando Fonseca, IC19
PT-2720-276 Amadora (Portugal)
E-Mail luisa_mmfigueiredo@hotmail.com
Received: December 7, 2018; Accepted after revision: January 10, 2019
Author Contributions
All listed authors contributed meaningfully to the study, as follows: Luísa Martins Figueiredo drafted the article; David Horta and Jorge Reis critically revised the article; and all authors approved the final version for publication. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.














