Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
GE-Portuguese Journal of Gastroenterology
Print version ISSN 2341-4545
GE Port J Gastroenterol vol.27 no.5 Lisboa Oct. 2020
https://doi.org/10.1159/000505581
RESEARCH ARTICLE
Upper Endoscopy in Patients with Extra-Oesophageal Reflux Symptoms: A Multicentre Study
Endoscopia alta em doentes com sintomas de refluxo extra-esofágicos: um estudo multicêntrico
Angelo Zulloa, Giulia Fiorinib, Gabrio Bassottic, Francesco Bachettic, Fabio Monicad, Daniele Macord, Omero Alessandro Paoluzie, Giuseppe Scaccianocef, Piero Portincasaf, Vincenzo De Francescog, Roberto Lorenzettia, Ilaria Maria Saracinob, Matteo Pavonib, Dino Vairab
aGastroenterology and Digestive Endoscopy, Nuovo Regina Margherita Hospital, Rome, Italy; bDepartment of Medical and Surgical Sciences, S. Orsola Hospital, University of Bologna, Bologna, Italy; cGastroenterology and Hepatology Section, Department of Medicine, University of Perugia Medical School, Perugia, Italy; dGastroenterology and Digestive Endoscopy, Academic Hospital Cattinara, Trieste, Italy; eGastroenterology Unit, Department of Systems Medicine, Tor Vergata University of Rome, Rome, Italy; fInternal Medicine A. Murri, Department of Biomedical Sciences and Human Oncology, University of Bari, Bari, Italy; gSection of Gastroenterology, Department of Medical Sciences, University of Foggia, Foggia, Italy
* Corresponding author.
ABSTRACT
Background: There are no evidence-based recommendations for performing upper gastrointestinal endoscopy (UGIE) in patients with extra-oesophageal symptoms of gastro- oesophageal reflux disease (GORD). However, UGIEs are often performed in clinical practice in these patients. We aimed to assess the prevalence of gastro-oesophageal lesions in patients with atypical GORD symptoms. Methods: Patients complaining of at least one extra-oesophageal GORD symptom and undergoing UGIE in seven centres were prospectively enrolled. Clinically relevant lesions (Barrett’s oesophagus, erosive oesophagitis, gastric precancerous conditions, peptic ulcer, cancer, and H. pylori infection) were statistically compared between groups regarding GORD symptoms (atypical vs. both typical and atypical), type of atypical symptoms, age, and presence of hiatal hernia. Results: Two hundred eleven patients were enrolled (male/female: 74/137; mean age: 55.5 ±} 14.7 years). Barrett’s oesophagus was detected in 4 (1.9%), erosive oesophagitis in 12 (5.7%), gastric precancerous conditions in 22 (10.4%), and H. pylori infection in 38 (18%) patients. Prevalence of clinically relevant lesions was lower in patients with only atypical GORD symptoms (28.6 vs. 42.5%; p = 0.046; χ2 test), in patients ≤50 years (20 vs. 44.8%; p = 0.004; χ2 test), and in those in ongoing proton pump inhibitor (PPI) therapy (21.1 vs. 40.2%; p = 0.01; χ2 test). No clinically relevant lesions were detected in patients ≤50 years, without alarm symptoms, and receiving PPI therapy. Hiatal hernia was diagnosed in only 6 patients with cardiologic and in 41 patients with earnose- throat symptoms (11.3 vs. 35.1%; p = 0.03; χ2 test). Conclusions: Clinically relevant lesions are uncommon among young (≤50 years) patients with extra-oesophageal GORD symptoms. Hiatal hernia is not more prevalent in patients with cardiologic symptoms and suspicion of GORD. The usefulness of UGIE in these patients is questionable.
Keywords: Upper gastrointestinal endoscopy, Extra-oesophageal reflux, Gastro-oesophageal reflux, Diagnostic yield
RESUMO
Introdução: Não existem recomendações baseadas na evidência para realização de endoscopia digestiva alta (EDA) em doentes com sintomas extra-esofágicos da doença de refluxo gastroesofágico (DRGE). No entanto, EDAs são frequentemente realizadas na orientação clinica destes doentes. O nosso objectivo foi avaliar a prevalência de lesões gastro-esofágicas em doentes com sintomas atípicos de DRGE. Métodos: Doentes com pelo menos um sintoma extra-esofágico de DRGE e que realizaram EDA em 7 centros foram prospectivamente recrutados. Lesões clinicamente relevantes (esófago de Barrett, esofagite erosiva, condições pré-malignas gástricas, úlcera péptica, cancro e infecção H. pylori) foram estatisticamente comparadas entre os grupos tendo em conta sintomas de DRGE (atípicos vs. quer típicos e atípicos), tipo de sintomas atípicos, idade e presença de hérnia do hiato. Resultados: Duzentos e onze doentes foram recrutados (H/M: 74/137; Idade média: 55.5 ±} 14.7 anos). Esófago de Barrett foi detetado em 4 (1.9%), esofagite erosiva em 12 (5.7%), condições pré-malignas gástricas em 22 (10.4%) e infeção H. pylori em 38 (18%) doentes. A prevalência de lesões clinicamente relevantes foi inferior em doentes com apenas sintomas atípicos (28.6 vs. 42,5%; p = 0.046; teste de qui-quadrado), doentes com ≤50 anos (20 vs. 44.8%; p = 0.004; teste de qui-quadrado), e nos doentes medicados com iniciadores da bomba de protoes (IBP) (21.1 vs. 40.2%; p = 0.01; teste de qui-quadrado). Nenhuma lesão clinicamente relevante foi detectada nos doentes com ≤50 anos, sem sintomas de alarme e medicados com IBP. Hérnia do hiato foi diagnosticada apenas em 6 doentes com sintomas do tipo cardíaco e em 41 com sintomas ORLs (11.3 vs. 35.1%; p = 0.03; teste de qui-quadrado). Conclusões: Lesões clinicamente relevantes são incomuns em doentes jovens com sintomas extra-esofágicos de DRGE. Hérnia do hiato não e mais prevalente em doentes com sintomas do tipo cardáaco e suspeita de DRGE. A utilidade da EDA nestes doentes e discutível.
Palavras-Chave: Endoscopia digestiva alta, Refluxo extra-esofágico, Refluxo gastroesofágico, Rendimento diagnóstico
Introduction
Upper gastrointestinal endoscopy (UGIE) is a useful procedure for diagnosis, surveillance, or exclusion of relevant gastroduodenal diseases [1]. Therefore, it is widely used in clinical practice for investigating patients with different symptoms, generally scheduled as open-access procedure [2]. Different guidelines on gastro-oesophageal reflux disease (GORD) recommend endoscopy in patients > 50 years or with long-lasting (> 5 years) symptoms to screening for Barrett’s oesophagus [3]. Moreover, UGIE should be performed irrespective of age when alarm symptoms (bleeding, dysphagia, persistent vomiting, anaemia, weight loss) are present [4]. GORD is highly prevalent in the Western and its incidence is increasing [5]. Classically, GORD may present with typical (heartburn, regurgitation), extra-oesophageal (laryngeal, pharyngeal, pulmonary, and cardiac) symptoms, or both [6]. According to our knowledge, no official guidelines nor expert-based recommendations suggest performing UGIE in the diagnostic work-up of patients presenting with only extra-oesophageal GORD symptoms [7–11]. Nevertheless, UGIEs are often performed in clinical practice for this indication.
To our knowledge, there are no consistent data on the prevalence of relevant gastro-oesophageal lesions in patients with extra-oesophageal GORD symptoms. Therefore, we designed this study aiming to assess the prevalence of relevant gastro-oesophageal lesions at UGIE in patients with atypical GORD symptoms observed in clinical practice.
Methods
Patients
This was a prospective, multicentre study involving seven centres (Bari, Bologna, Foggia, Perugia, Rome-1, Rome-2, Trieste). Consecutive patients complaining of at least one extra-oesophageal GORD symptom, with or without typical symptoms, referred for UGIE from September to December 2018 were invited to participate. Persistent cough, hoarseness, and pharyngeal globus/throat clearing or laryngitis (i.e., ear-nose-throat [ENT] symptoms) or retrosternal pain and palpitations (cardiologic symptoms) were considered as extra-oesophageal GORD symptoms, whilst heartburn or regurgitation as typical GORD symptoms. Dysphagia, anaemia, weight loss, and vomiting were considered as alarm symptoms. Exclusion criteria were (1) age < 18 years, (2) patients with only typical GORD symptoms, (3) symptoms already investigated with a previous UGIE, and (4) contraindication to take gastric biopsies.
Methods
All patients underwent UGIE with antral, incisura angularis, and gastric body biopsies, as in routine practice. Moreover, at least 6 oesophageal biopsies were taken when patients were complaining of dysphagia and no apparent lesions were detected to rule out eosinophilic oesophagitis. Barrett’s oesophagus was diagnosed according to endoscopic and histological standard criteria [11] and erosive oesophagitis according to the Los Angeles classification [12]. Peptic ulcer was defined as a deep lesion > 5 mm in diameter on gastric or duodenal mucosa. Hiatal hernia was detected when the apparent separation between the squamo-columnar junction and the constriction formed as the stomach traverses the hiatus was greater than 2 cm [13]. The presence of gastric precancerous conditions (atrophy or intestinal metaplasia) and H. pylori infection was assessed at histological examination [14]. Oesophageal or gastric cancers were confirmed at histology. Clinically relevant lesions – that is, those affecting patient’s management – included Barrett’s metaplasia, erosive oesophagitis, erosive gastro-duodenitis, eosinophilic oesophagitis, gastric precancerous conditions, H. pylori infection, peptic ulcer, and neoplasia. The use of proton pump inhibitor (PPI) was registered and gathered as ongoing, suspended from at least 2 weeks before, past use (> 3 months), and never performed.
Statistical Analysis
Clinically relevant lesions (Barrett’s oesophagus, erosive oesophagitis, gastric precancerous conditions, peptic ulcer, cancer, and H. pylori infection) were statistically compared between groups regarding GORD symptoms (atypical vs. both typical and atypical), type of atypical symptoms, age, and presence of hiatal hernia. The rate of frequencies and mean of values were calculated, as appropriate. The χ2 test or Fisher’s exact test was used to compare differences among sub-groups, as appropriate. The odds ratio (OR) values for differences with their 95% confidence intervals (CI) and the Number-Needed-to-Scope (NNS) were calculated. A p value less than 0.05 was considered statistically significant.
Results
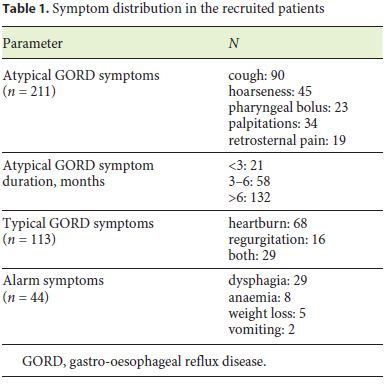
A total of 211 patients were recruited, including 74 males and 137 females, with a mean age of 55.5 ± 14.7 years, with 79 (37.5%) smokers. There were 98 patients complaining of only extra-oesophageal GORD symptoms and 113 with both atypical and typical symptoms (Table 1). A total of 52 (24.6%) patients underwent UGIE while receiving PPI therapy, 36 (17.1%) stopped therapy at least 2 weeks before, 29 (13.7%) had been treated in the past, and 94 (44.6%) never used these drugs. UGIE was prescribed by general practitioners in 86 (40.7%) cases, ENT specialists in 52 (24.6%), gastroenterologists in 54 (25.7%), and cardiologists in the remaining 19 (9%) patients.
At endoscopy, Barrett’s oesophagus was detected in 4 (1.9%) patients (C0M1: 3, C0M2: 1, all without dysplasia), erosive oesophagitis in 12 (5.7%) cases (LA-A: 10, LA-B: 1, and LA-C: 1), and hiatal hernia was diagnosed in 47 (22.3%) patients, whilst no cases of eosinophilic oesophagitis, peptic ulcers, and cancers were detected. At histological examination of gastric mucosa, precancerous conditions were present in 22 (10.4%) cases and H. pylori infection in 38 (18%) patients.
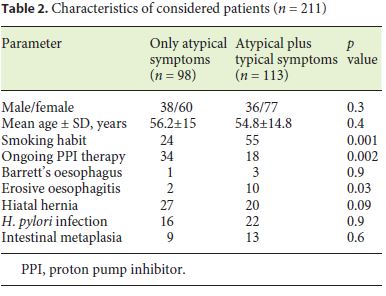
As shown in Table 2, patients with only extra-oesophageal symptoms underwent UGIE while taking PPI therapy more frequently than those with combined symptoms, whereas they were diagnosed with erosive oesophagitis less frequently. The cumulative prevalence of clinically relevant lesions was distinctly lower in patients with only extra-oesophageal GORD symptoms as compared to those with combined symptoms (28/98, 28.6% vs. 48/113, 42.5%; p = 0.046; OR: 0.54, 95% CI = 0.3–0.96), with an NNS of 15. Similarly, they were significantly lower in patients ≤50 than in those > 50 years old (15/75, 20% vs. 61/136, 44.8%; p = 0.004; OR: 0.3, 95% CI = 0.15–0.59; NNS = 22) and in patients on ongoing PPI therapy (11/52, 21.1% vs. 65/159, 40.2%; p = 0.01; OR: 0.3, 95% CI = 0.18– 0.8; NNS = 19). In detail, among patients with ≤50 years and without alarm symptoms (n = 61), there were 48 not receiving PPI and 13 in ongoing therapy. A relevant finding was detected in 12 and 0 patients, respectively (p = 0.04). Moreover, the manifest signs of GORD (erosive oesophagitis/ Barrett) was detected in 13 (11.5%) patients with combined symptoms and only in 3 (3.1%) with only extra-oesophageal symptoms (OR: 4.1, 95% CI = 1.13–14.9; p = 0.02; NNS = 10). Prevalence of clinically relevant lesions did not differ between patients with or without hiatal hernia (18/47, 38.1% vs. 42/164, 25.6%; p = 0.09). Hiatal hernia was diagnosed in only 6 (11.3%) patients with cardiologic and in 41 (35.1%) patients with ENT symptoms (p = 0.03). Moreover, patients with cardiologic symptoms showed the same prevalence of manifest signs of reflux at endoscopy when compared to the other patients (5.5 vs. 7.6%; p = 0.7).
Discussion
A recent systematic review showed that UGIEs are inappropriately prescribed in more than 20% of cases and that the diagnostic yield in inappropriate procedures is distinctly lower as compared to that of appropriate examinations [15]. In addition, inappropriate UGIEs have a negative impact on resources utilization, particularly when considering the very high number of procedures performed annually worldwide. More than 2.5 million UGIEs are performed yearly in Italy, mainly for investigating patients with dyspepsia, typical GORD reflux symptoms, or alarm symptoms [2]. To our knowledge, no guideline suggests performing UGIE in patients with extra-oesophageal GORD symptoms. Therefore, although a high rate of inappropriateness and a low diagnostic yield were foreseeable in this setting, no specific data are available at present.
There are some clinically relevant findings in our study on this topic. We found that the diagnostic yield in patients with only extra-oesophageal GORD symptoms is scarce, and it is distinctly lower than that of patients with concomitant typical symptoms. In detail, the probability of finding a clinical relevant lesion affecting patient’s management is reduced by 46% when compared to patients with simultaneous typical GORD symptoms. Similarly, our data showed that the likelihood of finding a relevant lesion is 70% lower when UGIEs are performed in patients with less than 50 years of age, as well as in those receiving PPI therapy, with 22 and 19 more UGIEs needed to discover a relevant lesion, respectively.
Although European and Italian guidelines suggest stopping PPI therapy at least 2 weeks before performing a diagnostic UGIE [3, 4], we found that as many as 1 in every 4 patients was referred for endoscopic examination while taking PPI therapy. In a previous Italian study, 1 in every 2 patients was on PPI therapy when UGIE was performed [16]. There is evidence that an ongoing PPI therapy significantly reduces the probability of finding erosive oesophagitis, gastroduodenal erosions, and H. pylori infection [17] and even that of gastric and oesophageal cancer [18]. Noteworthy, in our study, clinically relevant lesions were absent in all young patients with only extraoesophageal GORD symptoms who performed endoscopy on PPI therapy. On the other hand, we found that as many as 45% of patients were referred for UGIE without having previously performed a 2-month empiric therapy with adequate dose PPI, as suggested by experts [10, 19]. Based on all these observations, a critical reappraisal is needed for physicians in prescribing UGIE in this setting.
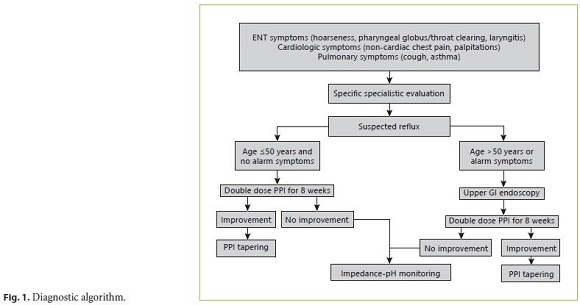
The potential role of hiatal hernia and/or GORD in triggering palpitations by stimulating heart innervations has been suggested [20]. A systematic review of 8 observational studies found that patients with GORD had an increased risk of developing atrial fibrillation, but it was impossible to establish a causal relationship based on these studies [21]. Unexpectedly, our data found that the prevalence of both hiatal hernia and endoscopic signs of GORD were not higher (if not lower) in patients referred for cardiologic symptoms. Likewise, an adequate pH-monitoring study, rather than UGIE, would be more appropriate in these patients to confirm or rule out GORD [10, 19], and a diagnostic algorithm may be proposed (Fig. 1).
Possible limitations of our study are a potential selection bias and the relatively small sample size. Indeed, the study included data of patients who were referred for UGIE in open-access Endoscopic Units, and they may be not representative of other patients with atypical GORD symptoms managed without resorting to an endoscopic examination. The number of patients with only atypical GORD symptoms was near one hundred, so that data of further larger studies might be helpful.
In conclusion, the data of this prospective, multicentre study found that clinically relevant lesions are uncommon among young (≤50 years) patients with only extraoesophageal GORD symptoms. Hiatal hernia is not more prevalent in patients with cardiologic symptoms than in other patients. Therefore, the usefulness of UGIE in these patients is questionable.
References
1 Beg S, Ragunath K, Wyman A, Banks M, Trudgill N, Pritchard DM, et al. Quality standards in upper gastrointestinal endoscopy: a position statement of the British Society of Gastroenterology (BSG) and Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland (AUGIS). Gut. 2017 Nov;66(11):1886–99.
2 Buscarini E, Conte D, Cannizzaro R, Bazzoli F, De Boni M, Delle Fave G, et al.; Italian Association of Hospital Gastroenterologists and Endoscopists (AIGO), Italian Society of Endoscopy (SIED), Italian Society of Gastroenterology (SIGE). White paper of Italian Gastroenterology: delivery of services for digestive diseases in Italy: weaknesses and strengths. Dig Liver Dis. 2014 Jul;46(7):579–89.
3 Steele D, Baig KK, Peter S. Evolving screening and surveillance techniques for Barrett’s esophagus. World J Gastroenterol. 2019 May;25(17):2045–57.
4 Caselli M, Zullo A, Maconi G, Parente F, Alvisi V, Casetti T, et al.; Working Group of the Cervia II Meeting. “Cervia II Working Group Report 2006”: guidelines on diagnosis and treatment of Helicobacter pylori infection in Italy. Dig Liver Dis. 2007 Aug;39(8):782–9.
5 El-Serag HB, Sweet S, Winchester CC, Dent J. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2014 Jun;63(6):871–80.
6 Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R; Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidencebased consensus. Am J Gastroenterol. 2006 Aug;101(8):1900–20.
7 Katz PO, Gerson LB, Vela MF. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2013 Mar;108(3):308–28.
8 Hom C, Vaezi MF. Extra-esophageal manifestations of gastroesophageal reflux disease: diagnosis and treatment. Drugs. 2013 Aug;73(12):1281–95.
9 Pearson JP, Parikh S, Orlando RC, Johnston N, Allen J, Tinling SP, et al. Review article: reflux and its consequences – the laryngeal, pulmonary and oesophageal manifestations. Conference held in conjunction with the 9th International Symposium on Human Pepsin (ISHP) Kingston-upon-Hull, UK, 21-23 April 2010. Aliment Pharmacol Ther. 2011 Apr;33 Suppl 1:1–71.
10 Vaezi MF, Katzka D, Zerbib F. Extraoesophageal symptoms and diseases attributed to GERD: where is the pendulum swinging now? Clin Gastroenterol Hepatol. 2018 Jul;16(7):1018–29.
11 Shaheen NJ, Falk GW, Iyer PG, Gerson LB; American College of Gastroenterology. ACG Clinical Guideline: diagnosis and management of Barrett’s esophagus. Am J Gastroenterol. 2016 Jan;111(1):30–50.
12 Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999 Aug;45(2):172–80.
13 Roman S, Kahrilas PJ. The diagnosis and management of hiatus hernia. BMJ. 2014 Oct 23;349:g6154. [ Links ]
14 Rugge M, Correa P, Di Mario F, El-Omar E, Fiocca R, Geboes K, et al. OLGA staging for gastritis: a tutorial. Dig Liver Dis. 2008 Aug;40(8):650–8.
15 Zullo A, Manta R, De Francesco V, Fiorini G, Hassan C, Vaira D. Diagnostic yield of upper endoscopy according to appropriateness: a systematic review. Dig Liver Dis. 2019 Mar;51(3):335–9.
16 Lahner E, Zullo A, Hassan C, Perri F, Dinis- Ribeiro M, Esposito G, et al.; MAG-Study Group. Detection of gastric precancerous conditions in daily clinical practice: a nationwide survey. Helicobacter. 2014 Dec;19(6):417–24.
17 Zullo A, Esposito G, Ridola L, Hassan C, Lahner E, Perri F, et al.; AIGO-SIED study group; AIGO-SIED study group. Prevalence of lesions detected at upper endoscopy: an Italian survey. Eur J Intern Med. 2014 Oct;25(8):772–6.
18 Bramble MG, Suvakovic Z, Hungin AP. Detection of upper gastrointestinal cancer in patients taking antisecretory therapy prior to gastroscopy. Gut. 2000 Apr;46(4):464–7.
19 Perotin JM, Launois C, Dewolf M, Dumazet A, Dury S, Lebargy F, et al. Managing patients with chronic cough: challenges and solutions. Ther Clin Risk Manag. 2018 Jun;14:1041–51.
20 Linz D, Hohl M, Vollmar J, Ukena C, Mahfoud F, Böhm M. Atrial fibrillation and gastroesophageal reflux disease: the cardiogastric interaction. Europace. 2017 Jan;19(1):16–20.
21 Roman C, Bruley des Varannes S, Muresan L, Picos A, Dumitrascu DL. Atrial fibrillation in patients with gastroesophageal reflux disease: a comprehensive review. World J Gastroenterol. 2014 Jul;20(28):9592–9.
Statement of Ethics
The study was performed according to the guidelines for Good Clinical Practice and the Declaration of Helsinki (1996 version, amended October 2000). Each patient consented to anonymously use clinical data. Since no experimental drugs were administered, no adjunctive costs or procedures for the patients were required, no identification of patients was allowed, and no funds were received, our Investigational Review Board waived formal review and approval, deeming the study to be an extension of existing clinical practice.
Disclosure Statement
The authors have no conflicts of interest to declare.
* Corresponding author.
Dr. Angelo Zullo
Gastroenterologia ed Endoscopia Digestiva
Ospedale Nuovo Regina Margherita
Via Emilio Morosini, 30, IT–00153 Rome (Italy)
Received: October 7, 2019; Accepted: December 9, 2019














