Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.27 no.6 Lisboa dez. 2020
https://doi.org/10.1159/000507205
ENDOSCOPIC SNAPSHOT
Infectious Proctitis due to Chlamydia trachomatis: Venereal Diseases in Proctology
Proctite infeciosa por Chlamydia trachomatis: Doenças venéreas em proctologia
João Carlos Silva, Adélia Rodrigues, João Carvalho
Department of Gastroenterology, Centro Hospitalar Vila Nova de Gaia e Espinho, Vila Nova Gaia, Porto, Portugal
* Corresponding author.
Keywords: Chlamydia trachomatis, Infectious proctitis, Homosexuality, Sexually transmitted diseases
Palavras-Chave: Chlamydia trachomatis, Proctite infeciosa, Homossexualidade, Doenças sexualmente transmissíveis
A 51-year-old man, with no relevant past medical history, was admitted to the emergency department due to intermittent bright red hematochezia and pain in the lower abdomen. His sexual history was remarkable for unprotected anal intercourse. Laboratory findings included a hemoglobin level of 12.8 g/dL and elevated C-reactive protein (3.51 mg/dL).
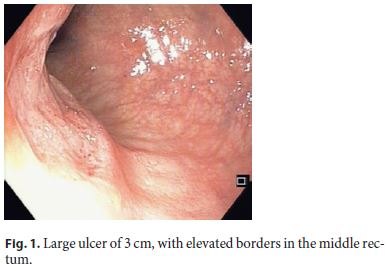
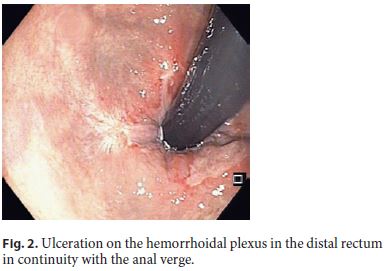
A hard and irregular ulcer was documented in the digital rectal examination, and flexible sigmoidoscopy allowed the identification of a large ulcer in the middle rectum (Fig. 1) as well as ulceration of the distal rectum (Fig. 2). No active bleeding or stigmata of recent bleeding were observed. Proctitis was therefore considered to be the cause of the gastrointestinal bleeding.
The following differential diagnosis was made: sexually transmitted proctitis (most commonly caused by Chlamydia trachomatis, Neisseria gonorrhoeae, herpes simplex virus [HSV], and Treponema pallidum) and inflammatory bowel disease. Acute proctitis in men who have sex with men (MSM) who practice receptive anal intercourse usually represents a sexually transmitted infection (STI). Empiric antibiotic therapy for gonorrhea and chlamydial infection was therefore initiated (ceftriaxone 250 mg intramuscularly as a single dose and doxycycline 200 mg/day for 7 days), while diagnostic study results were pending.
Histology was suggestive of a viral cytopathic effect with positive immunohistochemistry for HPV-p16. Cytology of the anal canal was negative for intraepithelial lesion or malignancy (NILM). Serology was negative for HIV, HAV, HBV, and HCV. Antibody testing for anti-T. pallidum came back negative. However, serology for C. trachomatis (IgM) was equivocal (17 RU/mL).
Positivity for C. trachomatis in molecular biology (polymerase chain reaction) from an anal swab confirmed the diagnosis of infectious proctitis. Results came back negative for gonorrhea and HSV. The patient was advised to notify his sexual partners and explain the need for a medical evaluation. Taking the C. trachomatis positivity into consideration, treatment with doxicillin was extended to 3 weeks and this led to the resolution of symptoms.
Anoscopy after 2 weeks showed no rectal lesions. Ileocolonoscopy performed 3 months later confirmed healing of the rectal lesions. No further lesions were observed. The patient was followed for 12 months and remained asymptomatic.
Infectious proctitis is an increasing diagnosis in MSM [1]. The differential diagnosis between infectious causes (C. trachomatis, gonorrhea, HSV, and syphilis) and noninfectious causes (inflammatory bowel disease and cancer) is difficult in many cases [2, 3].
References
1 Bissessor M, Fairley CK, Read T, Denham I, Bradshaw C, Chen M. The etiology of infectious proctitis in men who have sex with men differs according to HIV status. Sex Transm Dis. 2013 Oct;40(10):768–70.
2 Levy I, Gefen-Halevi S, Nissan I, Keller N, Pilo S, Wieder-Finesod A, et al. Delayed diagnosis of colorectal sexually transmitted diseases due to their resemblance to inflammatory bowel diseases. Int J Infect Dis. 2018 Oct;75:34–8.
3 Santos AL, Coelho R, Silva M, Rios E, Macedo G. Infectious proctitis: a necessary differential diagnosis in ulcerative colitis. Int J Colorectal Dis. 2019 Feb;34(2):359–62.
Statement of Ethics
Informed consent was obtained from the patient.
Disclosure Statement
The authors declare there are no conflicts of interest for this article.
Funding Sources
No grant support was provided for this article.
* Corresponding author.
João Carlos Silva
Department of Gastroenterology, Centro Hospitalar Vila Nova de Gaia e Espinho
Rua Conceição Fernandes
PT–4434-502 Vila Nova Gaia, Porto (Portugal)
Received: November 26, 2019; Accepted: January 18, 2020
Author Contributions
J. Carvalho: revised the paper critically for important intellectual content. A. Rodrigues: patient’s follow up and decisive intervention in therapeutic strategy. J.C. Silva: evaluation of the patient at admission and endoscopic study; analysis and interpretation of the case and drafting of the article.














