A 76-year-old female patient presented with cholestasis. Medical history was significant for remote cholecystectomy and endoscopic retrograde cholangiopancreatography (ERCP) due to cholangitis with papillotomy and extraction of stones at an outside institution 3 months before. The ERC(P) report did not indicate intentional and/or unintentional pancreatic duct (PD) opacification, and the appearance of the papilla was not specifically mentioned apart from drainage of putrid secretions. At the time, the ERC indication was established after transabdominal ultrasound indicating bile duct dilation in the presence of laboratory and clinical signs of cholangitis. However, the recent endoscopic ultrasound nonetheless indicated marked persistent common bile duct dilation up to 18 mm still with common bile duct stone disease. Surprisingly, PD width was moderately increased up to 7 mm in the pancreatic head without intraductal vegetations and/or accompanying cystic and/or solid pancreatic lesions, consistent with intraductal papillary mucinous neoplasia (IPMN) (Fig. 1a). In line with this, the duodenoscopic view demonstrated a typical fish-mouth appearance of the papilla with the biliary orifice more cranially (Fig. 1b). After performing pancreatic juice aspiration (post hoc cytology negative), a cholangiogram revealed a complex stone burden with marked bile duct dilation and dilation-assisted stone extraction was deemed necessary. An endoscopic papillary large balloon dilation (EPLBD) to 12 mm was performed to reduce the number of mechanical lithotripsies needed. EPLBD also facilitates direct cholangioscopy (DC) if it is considered essential to confirm complete bile duct clearance or if there is a need for cholangioscopy-guided electrohydraulic lithotripsy (Fig. 1c, d). Notwithstanding that the conventional ERCP-based approach to stone clearance presumably proved successful, DC after freehand intubation using an ultra-slim upper endoscope was performed to exclude persistent bile duct stone disease and, albeit exceedingly rare, concomitant intraductal papillary neoplasia of the bile duct [1] (Fig. 1e). Of note, given the bile duct diameter, neither CO2nor saline was applied for bile duct distension with room air being contraindicated anyway due to concern of air embolism [2]. Same-session performance of direct pancreatoscopy using the 5.9-mm outer diameter upper endoscope was not considered, given the overall only moderately increased PD diameter [3]. However, given the increasing appreciation of pancreatoscopy for workup and intraluminal staging of IPMN, single-operator pancreatoscopy using the novel digital Spyglass platform might be scheduled in case endoscopic ultrasound and/or magnetic resonance CP surveillance may indicate progression in PD dilation [4,5].
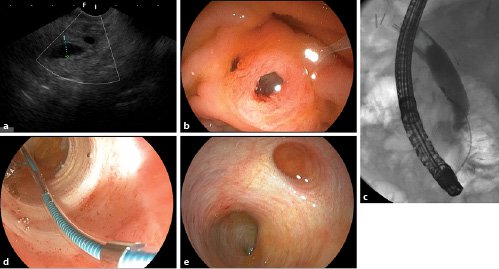
Fig. 1. a Longitudinal endoscopic ultrasound at the level of the papilla indicating pancreatic duct (PD) dilation.bDuodenoscopic view of the formerly missed fish-mouth papilla. Note the small biliary orifice at the duodenal wall at 10 o’clock.cEPLBD using a 12-mm controlled radial extension balloon.dThe papillary region after EPLBD with minor oozing and cholesterol stone material after extraction.eDirect cholangioscopy using an ultra-slim upper endoscope (outer diameter 5.9 mm) excluding persistent stone disease with normal biliary mucosa. Note cystic duct stump at 1 o’clock.
A missed diagnosis of fish-mouth papilla may seriously impact patient outcome with main duct IPMN <10 mm and lack of worrisome features warranting surveillance as perFukuokacriteria. Dilation-assisted stone extraction followed by DC for confirmation of freedom from stones and/or extraction under direct endoscopic vision is considered to represent the most powerful approach for advanced bile duct stone disease.














