Introduction
Liver diseases account annually for approximately 2 million deaths worldwide [1-3], most of them potentially preventable [1]. Together, cirrhosis and liver neoplasms were responsible for 3.5% of all deaths worldwide in 2015 [2,3], and the number has been increasing [2]. Liver cirrhosis alone accounts for more than 1 million deaths per year [1,2], being the 11th cause of death [2] and the fourth cause of disability-adjusted life years in the world [1].
Europe has the largest burden of liver disease in the world [4], with an estimated prevalence of 26.0 cases per 100,000 inhabitants [3]. In Europe, alcoholic liver disease is the major cause of cirrhosis-associated death (9.2 deaths per 100,000 inhabitants), followed by hepatitis C virus infection (5.3/100,000 inhabitants) and hepatitis B virus infection (3.9/100,0000 inhabitants) [5].
In Portugal, liver cirrhosis and chronic liver disease accounted for 0.9% of all deaths occurring in 2017 (1.5% of deaths among males and 0.4% of deaths among females) [6]. The most common cause of liver cirrhosis is alcoholic liver disease, which was responsible for 63-84% of hospital admissions for liver disease or liver cirrhosis in 3 nationwide studies on data from 1993-2012 [7-9]. Hepatitis C-related liver disease was a common and increasing cause of cirrhosis, at least until recently: admissions for hepatitis C-related liver cirrhosis rose about 50% between 2003 and 2012 [9].
Some recent factors may have been changing the epidemiology of liver cirrhosis in Portugal in the last few years. Alcohol consumption has been decreasing [10]. In 2015, Portugal was one of the first countries in the world to approve universal access to direct-acting antivirals for hepatitis C [11], during the first years preferentially for patients with advanced disease, with over 18,000 patients with treatment authorized between 2015 and 2017 [12]. Nonetheless, a possible impact on the national burden of liver disease has not been evaluated yet.
An ongoing monitorization of the epidemiology of liver disease in Portugal is essential both to evaluate implemented policies and to identify areas in need for further projects.
Patients and Methods
We separately evaluated hospital admissions for liver cirrhosis, and mortality and potential years of live lost for liver cirrhosis and chronic liver disease in the present descriptive study. Data on hospital admissions were extracted (on 15th November 2019) from the Diagnosis-Related Group database from the Portuguese Health System’s Central Administration, a national database where all discharge diagnoses from public hospitals in Portugal Mainland are registered. Admissions at public hospitals represent the vast majority of admissions in the country (78.9% of all admissions in Portugal in 2012) [13]. Codifications completed up to December 2016 were registered according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) [14], and from 1st January 2017 onwards (irrespective of discharge date) are registered according to the Tenth Revision of ICD [15,16]. For every admission, data on patient demographics, type of admission, length of stay, outcome, main diagnosis, and up to 19 secondary diagnoses are collected.
We selected all admissions for liver cirrhosis, from patients aged 20 years or older, between 2010 and 2017. To specifically retrieve admissions in which the main diagnosis was cirrhosis (and not those where cirrhosis was a concurrent secondary disease), we selected admissions whose main diagnosis was cirrhosis itself, or whose main diagnosis was a complication of cirrhosis with a concomitant secondary diagnosis suggestive of cirrhosis. Specific codes were selected after a review of several coded admissions, and possible correspondences between ICD-9-CM and ICD-10 codes were extensively reviewed.
Codifications defining cirrhosis as the main diagnosis were alcoholic cirrhosis, biliary cirrhosis, and other cirrhosis of the liver (codes 571.2, 571.6 or 571.5 in ICD-9-CM or K70.3, K74.3, K74.4, K74.5 or K74.6 in ICD-10).
Complication of cirrhosis was defined as either one of the following: hepatic encephalopathy (codes 572.2 or 348.3 in ICD-9-CM or K72.9, K70.41 or G93.4 in ICD-10), portal hypertension (codes 572.3 in ICD-9-CM or K76.6 in ICD-10), esophageal varices (codes 456.0, 456.1 or 456.2 in ICD-9-CM or I85 or I86.4 in ICD-10), ascites (codes 789.59 in ICD-9-CM or R18 in ICD-10), spontaneous bacterial peritonitis (codes 567.23 in ICD-9-CM or K65.2 in ICD-10), hepatorenal syndrome (codes 572.4 in ICD-9-CM or K76.7 in ICD-10), unspecified pleural effusion (codes 511.9 or 511.89 in ICD-9-CM or J90, J91.8 or J94.8 in ICD-10), jaundice (codes 782.4 in ICD-9-CM or R17 in ICD-10), alcoholic hepatitis (codes 571.1 in ICD-9-CM or K70.1 or K70.4 in ICD-10), other sequelae of chronic liver disease/chronic liver failure (codes 572.8 in ICD-9-CM or K72.1 or K72.9 in ICD-10), acute/subacute necrosis/failure of the liver (codes 570 in ICD-9-CM or K72.0 in ICD-10), or primary liver neoplasm/liver cell carcinoma (codes 155.0 in ICD-9-CM or C220 in ICD-10).
Codifications defining cirrhosis as a secondary diagnosis (in admissions whose main diagnosis was a complication of cirrhosis) were chronic liver disease/failure (codes 571.8, 571.9 or 572.8 in ICD-9-CM or K70.2, K70.4, K70.9, K72.1, K72.9, K74.0, K74.2 or K76.9 in ICD-10) and chronic hepatitis (codes 571.4 in ICD-9-CM or K73, K75.2, K75.3, K75.4, K75.8, K75.9 in ICD-10).
Cirrhosis was classified according to etiology considering alcoholic liver disease, hepatitis B, and hepatitis C. We have allowed single or multiple causes for cirrhosis. For example, alcoholic cirrhosis was defined in the presence of alcoholic liver disease and the absence of chronic hepatitis B or C. If both chronic hepatitis C and alcoholic liver disease were present (in the absence of chronic hepatitis B), cirrhosis was presumed to be caused by both hepatitis C and alcohol.
Codifications defining cause of cirrhosis were alcoholic liver disease (codes 571.0, 571.1, 571.2 and 571.3 in ICD-9-CM or K70.0, K70.1, K70.2, K70.4, K70.3 or K70.9 in ICD-10), chronic hepatitis B (codes 070.22, 070.23, 070.32, 070.33 or V02.61 in ICD-9-CM and B18.0, B18.1, B19.1 or Z22.51 in ICD-10), and chronic hepatitis C (codes 070.44, 070.54, 070.7 or V02.62 in ICD-9-CM or B18.2, B19.2 or Z22.52 in ICD-10). Other causes of cirrhosis were not considered in the analysis.
Data on mortality and potential years of life lost were retrieved from the National Institute for Statistics (Statistics Portugal), both from the online available metainformation and from annual reports. Available data are on liver cirrhosis and chronic liver disease in aggregation.
Statistical analysis was carried out using Microsoft Office Excel® 2010 (Microsoft Corporation®, Redmond, WA, USA), IBM SPSS Statistics 21® (IBM® Corporation, Armonk, NY, USA) and R Statistical Software for Windows® (R Foundation®, Vienna, Austria). Apvalue less than 0.05 (two-sided) was considered statistically significant. Test of time trends were performed using linear regression with time as an independent variable.
Results
Hospital Admissions for Liver Cirrhosis (All Causes)
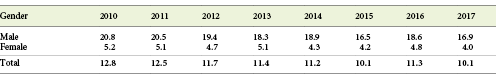
Between 2010 and 2017, there were a total of 51,438 hospital admission episodes for liver cirrhosis in Portugal, 77.7% (n= 39,967/51,438) corresponding to male patients. A cause of cirrhosis was identified in 85.0% (n= 43,704/51,438) of admissions. The most frequent cause was alcoholic liver disease, followed by chronic infection by hepatitis C virus and chronic infection by hepatitis B virus. The annual number of admissions for liver cirrhosis from all causes decreased significantly (p= 0.044) over the 8-year period, although this tendency was not observed in most etiologies when analyzed independently. Annual number and longitudinal trends of hospital admissions according to etiology of cirrhosis and year are detailed in Table 1 and Figure 1.
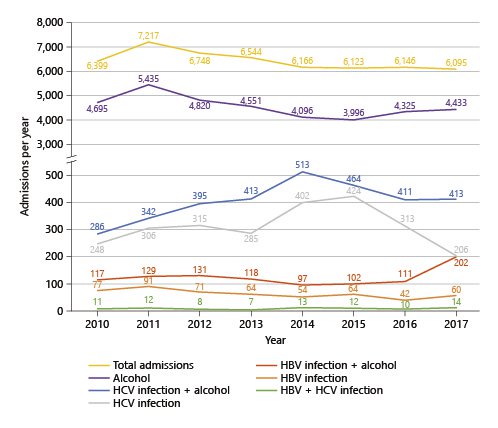
Fig. 1 Annual hospital admissions for liver cirrhosis between 2010 and 2017, by cirrhosis etiology. Total number of admissions decreased (p= 0.044). Admissions for alcoholic cirrhosis remained stable (p= 0.075). Annual admissions for cirrhosis due to hepatitis C (p= 0.861) and hepatitis C plus alcohol (p= 0.082) remained stable. Admissions for cirrhosis due to hepatitis B decreased (p= 0.023), but admissions for cirrhosis due to hepatitis B plus alcohol remained stable (p= 0.393). Admissions for cirrhosis due to both hepatitis B and hepatitis C remained stable (p= 0.395) (Diagnosis-Related Group database).
Cirrhosis due to Alcoholic Liver Disease
Alcoholic liver disease was the single most common cause of admission for cirrhosis in Portugal between 2010 and 2017. Alcoholic cirrhosis alone, without concomitant hepatitis B or C, accounted for 70.7% (n= 36,351) of all admission episodes in the period, 82.2% (n= 29,898/36,351) of them corresponding to male patients. Globally, the number of annual admissions due to alcoholic cirrhosis remained stable (p= 0.075) during the 8-year observation period, ranging from 5,435 admissions in 2011 to 3,996 admissions in 2015. The largest number of annual admissions due to alcoholic cirrhosis was observed in 2011.
Furthermore, alcoholic liver disease was an etiological co-factor of liver cirrhosis in 55.6% of admissions for hepatitis C virus-related liver disease (n= 3,237/5,823) and in 62.3% of admissions for hepatitis B virus-related liver disease (n= 1,007/1,617). Indeed, either alone or associated with a viral etiology, alcoholic liver disease was present in 78.9% of all admissions (n= 40,595/51,438), as shown in Table 1and Figure 1.
Cirrhosis due to Chronic Infection by Hepatitis C Virus
Chronic infection by hepatitis C virus is a major cause of cirrhosis in Portugal and was present in 11.3% (n= 5,823/51,438) of all admission episodes for liver cirrhosis, 81.3% (n= 4,736/5,823) of them corresponding to male patients. Among those admissions, only 42.9% (n= 2,499/5,823) corresponded to chronic hepatitis C alone; in 55.6% (n= 3,237/5,823) there was concomitant alcoholic liver disease, and in 1.5% (n= 87/5,823) hepatitis B virus was present as an etiological cofactor.
Considering the patients with cirrhosis due to hepatitis C virus infection alone, the annual number of admissions remained globally stable between 2010 and 2017 (p= 0.861). But in detail, the annual number of admissions increased from 248 in 2010 to 424 in 2015 and then rapidly decreased to a minimum of 206 in 2017. Similar trends are observed in hospital admissions for cirrhosis due to hepatitis C plus alcoholic liver disease, with an inversion point in 2014 (Table 1; Fig. 1). Recall that wide availability of direct-acting antivirals for hepatitis C was initiated in 2015 [11].
Cirrhosis due to Chronic Infection by Hepatitis B Virus
Admissions for hepatitis B-related cirrhosis accounted for 3.1% (n= 1,617/51,438) of admission episodes for cirrhosis between 2010 and 2017, 81.8% (n= 1,322/1,617) corresponding to male patients. In most cases, a concomitant cause of liver cirrhosis was present: in 62.3% (n= 1,007/1,617) alcoholic liver disease and in 5.4% (n= 87/1,617) concomitant infection by hepatitis C virus.
Between 2010 and 2017, the number of admissions for cirrhosis due to hepatitis B decreased (p= 0.023) (Table 1; Fig. 1).
Mortality and Potential Years of Life Lost due to Liver Cirrhosis and Chronic Liver Disease
Mortality due to liver cirrhosis and chronic liver disease in Portugal decreased significantly between 2010 and 2017 (p= 0.002), from a maximum of 1,357 deaths in 2010 to a minimum of 1,038 deaths in 2017 [6,13,17-21], as shown in Figure 2.
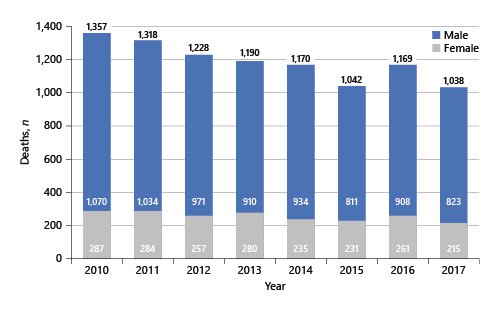
Fig. 2 Annual mortality due to cirrhosis and chronic liver disease between 2010 and 2017, per patient gender [6, 13, 17-21].
Mortality rates decreased from 12.8/100,000 inhabitants in 2010 to 10.1/100,000 inhabitants in 2017 [13]. Mortality rates were higher in male patients ranging from 20.8 deaths/100,000 inhabitants in 2010 to 16.9 deaths/100,000 inhabitants in 2017. In females, the mortality rate in 2012 was 5.2 deaths/100,000 inhabitants and decreased to 4.0 deaths/100,000 inhabitants in 2017 (Table 2). Most deceased patients were aged 65-74 years [13].
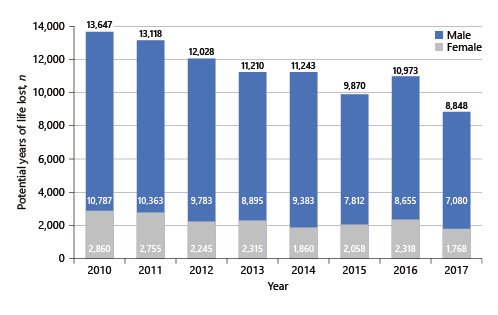
In close accordance with mortality trends, the potential years of life lost due to liver cirrhosis and chronic liver disease in Portugal decreased significantly between 2010 and 2017 (p= 0.001). A maximum of 13,647 years lost were observed in 2010, decreasing to 8,848 years lost in 2017 [13]. A male prevalence was once again observed in all the evaluated years, as shown in Figure 3.
Discussion
We observed a significant decrease in the burden of liver cirrhosis in Portugal between 2010 and 2017, evaluated both by hospital admissions for liver cirrhosis and by mortality and potential years of life lost due to cirrhosis and chronic liver disease. Alcohol-related liver disease remains, by far, the major cause of liver cirrhosis in Portugal. Alcohol alone accounts for over 70% of admitted cirrhosis and is a cofactor in over 50% of cirrhosis related either to hepatitis C or hepatitis B virus.
Admissions for alcoholic cirrhosis remained stable during the evaluated period, even though alcohol consumption decreased in the period (13.5 L of pure alcohol/year per capita in 2010 to 12.3 L/year in 2016) [10]. Alcohol beverage sales decreased between 2012 and 2015 in the country as well [10].
We may speculate on an apparent decrease in hospital admissions during the latter half of the analysis period, although statistically the number of admissions remained stable, with a possible contribution from an outlier value in 2011 that we were not able to justify.
The predominance of alcoholic cirrhosis among males is in accordance with alcohol consumption patterns: in Portugal, consumption per capita is much higher among men (20.5 L pure alcohol/year) than among women (5.1 L/year) (data from 2016) [10].
Chronic hepatitis C is an important cause of liver disease in the world. In the European Union, there was an estimated prevalence of more than 3.2 million infected patients in 2015 [22,23] and 342,243 deaths in 2017 [5,24]. In Portugal, seroprevalence for hepatitis C was estimated to range from 0.46 to 1.5% [25-27]. Estimates for the whole Portuguese population are frail and difficult to obtain as infection tends to cluster in high-risk groups, such as people who use drugs, whose seroprevalence is higher (59% in individuals undergoing treatment for drug abuse, and over 80% among people who inject drugs) [28-30].
Continuing a rising trend since 2003 that we already described in a previous work [9], we observed an increase in annual admissions for hepatitis C-related cirrhosis (either alone or associated with alcoholic liver disease) until 2014-2015, followed by a steady decrease thereafter. The short period of observation does not allow for an absolute conviction, but those are encouraging data suggesting a decrease in the burden of hepatitis C-related liver disease in the country since 2014-2015.
In fact, since 2015, there is universal access to direct-acting antivirals for treatment of hepatitis C in the country. Although all patients with hepatitis C virus infection are eligible nowadays to start therapy with direct-acting antivirals, during the first 2 years priority was given to patients with advanced liver disease (F3/F4) and a few other prioritizing factors [31]. The successful treatment of patients with more advanced disease was expected to prevent decompensation [32-34] with impact already in the short term [35,36].
Up to December 2015, 8,650 treatments were authorized, 57.3% (n= 4,954/8,650) of them for patients with advanced liver fibrosis or cirrhosis (F3/F4). Since 2016, the proportion of treated patients with lower grades of fibrosis has been increasing. Up to June 2018, a total of 20,367 treatments were started, about one half of them - 45.5% (n= 9,256/20,367) - for patients with advanced fibrosis and cirrhosis [37]. Up to January 2020, 24,926 patients started treatment, with a cure rate of 96.5% (n= 15,200/15,755): over 15,200 patients were cured in 5 years [38].
Each successful hepatitis C treatment means individual liver-related and non-liver-related benefits for the treated patient, including reductions/benefits in liver stiffness, portal hypertension, risk of decompensation, hospitalizations, incidence of hepatocellular carcinoma, need for liver transplant, extrahepatic manifestations, liver-related and all-cause mortality [33-36,39]. But furthermore, each hepatitis C cure contributes to lower disease transmission in the population [39], ultimately promoting a decrease in incidence and prevalence of the disease [40-42].
A favorable cost-effectiveness of direct-acting antivirals was anticipated [43] and has been confirmed [44]. Our results suggest a decreasing burden of hepatitis C-related liver disease in Portugal, as has been recently described in Spain until 2015 [45]. Further monitorization of epidemiology of hepatitis C in Portugal is needed for more solid interpretations.
The burden of admitted hepatitis B-related cirrhosis is low. The present results are generally overlapping with a previous observation, where hepatitis B virus accounted for 2.9% of all cirrhosis-related admissions between 2003 and 2012 [9]. The prevalence of hepatitis B in Portugal is low and has been decreasing in the last decades (HBsAg prevalence was 1.13-2.0% in studies carried out in 1980-1989 and 0.02-1.45% in studies carried out in 1990-2014, although higher in some population subgroups [46]), probably reflecting the efficacy of vaccination programs adopted in Portugal since 1994 [28] and the access to antiviral therapies. Furthermore, long-term treatment with nucleos(t)ide analogues induces cirrhosis regression [47] and reduces the risk of decompensation and hepatocellular carcinoma [2,3], allowing the vast majority of these patients to be followed up on an ambulatory basis without need for hospital admissions.
The decrease in mortality and, accordingly, in the years of potential life lost is encouraging and corroborates a decreasing burden of liver cirrhosis in Portugal during this 8-year period. In fact, a decrease in mortality due to liver cirrhosis in Portugal has been observed at least since the 1980s (e.g., in 1986, there were 2,953 deaths due to liver cirrhosis in the country, corresponding to mortality rates of 43.2/100,000 inhabitants among men and 17.2/100,000 inhabitants among women) [13].
The present results contribute to an update on the burden of liver cirrhosis in Portugal in the last few years. Analysis of hospital admissions was based on a prior report from our team [9]. Data on the overlapping years (2010-2012) are similar although not exactly equal, in our opinion essentially due to updates of the databases that occurred in the meanwhile. Aware of this limitation, and as the most recent data are more susceptible to updating, we decided not to consider data corresponding to 2018 (data extraction from database performed on 2019). We highlight that the burden of hospital admissions was analyzed through the number of admission episodes, rather than the number of admitted patients, and, therefore, direct extrapolation of prevalences of the different causes of cirrhosis is hampered.
Another potential limitation is the transition in codification of the admissions database, from ICD-9-CM to ICD-10, for codifications performed from 1st January 2017 onwards. In order to minimize this potential susceptibility, we performed an extensive review of both ICD-9 and ICD-10 codes to establish the best possible correspondences for each ICD-9-CM code.
As every coding-based report, results are directly dependent on the correct codification of the admission files, which may be suboptimal [9]. Furthermore, there is no specific code for viral hepatitis [9,48,49], which may therefore be underreported. At last, we only considered 3 causes of liver cirrhosis, impairing the analysis of other causes of liver disease, including non-alcoholic fatty liver disease (which was not analyzed as it lacks a specific code in ICD-9-CM).
Nonetheless, and keeping these limitations in mind, we believe that the present results are solid and credible. We are also convinced that the analysis of longitudinal trends is not severely affected by possible defective reporting as these errors are not expected to change over time. Nevertheless, continuing analysis in Portugal as well as similar studies in other countries, particularly in southern Europe, are needed.
Conclusion
There was a significant reduction in the overall burden of liver cirrhosis in Portugal between 2010 and 2017, evaluated by the decrease in hospital admissions and, more importantly, by the decreasing mortality and of potential years of life lost.
During the analyzed period, reduction in alcohol consumption was not followed by a significant decrease in alcohol-related cirrhosis admissions. On the other hand, there was an apparent decrease of hepatitis C-related admissions after the wide availability of direct-acting antivirals. Admissions for hepatitis B cirrhosis also decreased during the evaluated period.