A 21-year-old female presented for dysphagia and odynophagia with retrosternal localization for 4 days. Chest pain and/or accentuation during inspiration were not reported. Medical history included penicillin allergy and recent streptococcal pharyngitis as confirmed by microbial analysis of a throat swab diagnosed 12 days before. After prescription of cefuroxime for 5 days, antibiotic treatment was switched to a 5-day azithromycin regimen due to insufficient clinical response. Esophagogastroduodenoscopy (EGD) revealed three deep, well-demarcated esophageal ulcers estimated at 8 mm with slightly raised edges. Of note, in the absence of vesicles, all mucosal lesions were located at the same level at 27 cm from the incisors on a background of an otherwise normal esophageal mucosa (Fig. 1a). Histopathology from the ulcer bed and rim indicated bland ulceration with a dense inflammatory infiltrate with edema of squamous cell epithelium without evidence for viral and/or fungal esophagitis (Fig. 1b, c: H&E. ×5, ×10, respectively). Ancillary immunohistochemistry for herpes simplex virus type 1 and cytomegalovirus were unremarkable, respectively. Given a diagnosis of pill esophagitis for which there are no established and proven treatment options beyond stopping the offending substance, the patient was additionally treated with proton pump inhibitors and sucralfate suspension on an empirical basis. While dysphagia rapidly ceased, repeat EGD 14 days later revealed complete ulcer healing (Fig. 1d). Notwithstanding, the need for repeat endoscopy and its distinct timing may remain debatable.
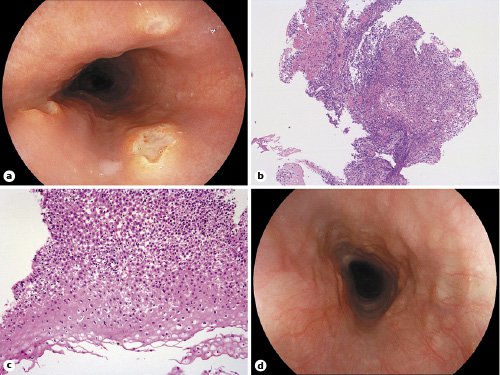
Fig. 1 a Esophagogastroduodenoscopy (EGD) demonstrating esophageal ulcers with an estimated maximum size of 8 mm and slightly raised borders. Note that all esophageal mucosal injury lesions are located at the same height within the esophagus at 27 cm from the incisors (most likely representing physiological narrowing due to the left main bronchus). b, c Biopsies from the ulcer bed and rim indicate bland ulceration with a dense inflammatory infiltrate and epithelial edema (H&E. ×5, ×10, respectively). In addition, there is no evidence for viral esophagitis as substantiated by negative herpes simplex virus type 1 and cytomegalovirus immunohistochemistry (not shown). d Complete ulcer healing on repeat EGD 14 days later.
As a newer-generation macrolide, azithromycin-related pill esophagitis presumably due to prolonged mucosal contact at physiological narrowings; e.g., as in this case the left main bronchus indentation, has only occasionally been reported in the literature, unlike for its acidic precursor substance doxycycline [1, 2]. In our personal endoscopy experience, this unique report represents the first (and up to now only) clinical case of azithromycin-induced pill esophagitis. Medication-induced esophageal injury may be prevented mainly by instructing patients to take oral medications with ample of water and avoiding immediate recumbency [3].














