Stenosis of hepaticojejunostomy (HJ) is a potentially serious postoperative complication after pancreaticoduodenectomy [1]. It causes biliary stasis leading to intrahepatic lithiasis and recurrent cholangitis.
We herein describe the case of a patient who underwent pancreaticoduodenectomy with Roux-en-Y reconstruction for an ampullary carcinoma 6 years earlier, developing late HJ stenosis. The first episode of cholangitis was 4 years after surgery. After a trial of percutaneous transhepatic dilation and drainage, the episodes of cholangitis recurred. A repeat magnetic resonance cholangiography showed a permeable HJ and development of intrahepatic lithiasis. An endoscopic retrograde cholangiopancreatography with double-balloon enteroscope [2] was unsuccessful due to a slight twisting of the Roux-en Y anastomosis, and the patient was placed with a percutaneous transanastomotic drain to prevent further episodes of cholangitis. Because of the proximity of the pancreatic anastomosis to the HJ, a surgical approach was considered technically difficult and potentially hazardous. After multidisciplinary discussion, a percutaneous transhepatic cholangioscopy (PTC) [2] was decided. Under general anesthesia and systemic antibiotic therapy, a percutaneous 12 Fr sheath was placed over a guidewire and the drain removed (Fig. 1a), allowing the introduction of a SpyGlassTM cholangioscope in the intrahepatic biliary tree (Fig. 1b) [2]. The procedure was performed with a dual-image system displaying the progression of the procedure with cholangiographic images alongside the cholangioscopic view, enabling the exact location of the cholangioscope inside the biliary tree, particularly of the most affected ducts (right posterior sector and left hepatic duct) (Fig. 2) [2]. During the procedure, the anastomosis was confirmed to be patent, and laser lithotripsy with Holmium Laser SystemTM (5Hz, minimum power - increased as needed) [3, 4] (Fig. 3) and Dormia basket lithotomy [2] of intrahepatic stones were performed. Completion cholangiogram showed absence of major filling defects. However, since some debris remained even after copious lavage, a percutaneous transanastomotic drain was left in order to prevent cholangitis. This was removed 1 week after repeat cholangiography confirmed clearance of the intrahepatic ducts and a permeable HJ. Four months after the procedure, the patient is asymptomatic, with no clinical or biochemical signs of cholangitis or cholestasis.
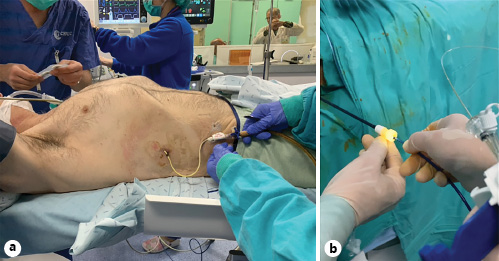
Fig. 1: a Initial patient setup in the angiography suite, with percutaneous biliary drain being replaced over a guidewire for a 12 Fr sheath. b The cholangioscope is being placed through the percutaneous sheath for the approach to the bile duct.
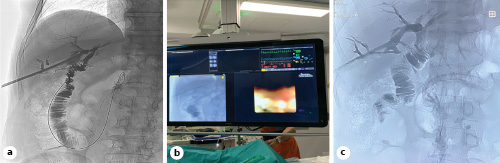
Fig. 2: a Initial cholangiography displaying the 12 Fr sheath and multiple filling defects in the right posterior sectorial duct and no filling of the left hepatic duct, but with permeable anastomosis. b, c Simultaneous radiological and endoscopic percutaneous approach of the biliary tract reflecting the importance of a multidisciplinary team approach in cases such as these. The dual monitoring system allowed for the precise confirmation of the cholangioscope, enabling the clearance of the entire intrahepatic biliary tree.
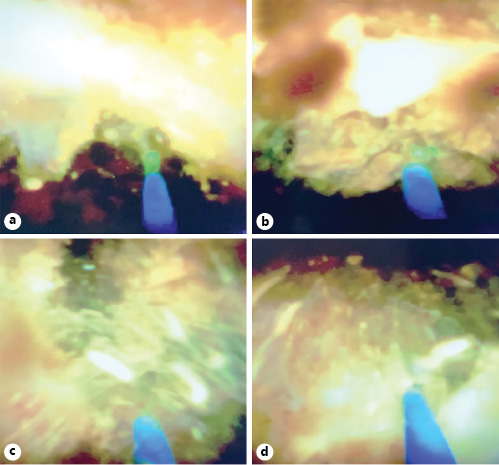
Fig. 3: Panel showing step-by-step approach of lithotomy and laser lithotripsy, with the laser being aimed (a), fired (b), and destroying a stone (c) into fragments (d).
This innovative, multidisciplinary approach ensured a clearance of the intrahepatic bile ducts without morbidity or the need for reoperation, making it a therapeutic option in cases of intrahepatic stones in patients with a previous Roux-en-Y reconstruction. It is a new technique with enormous potential to grow, but both worldwide experience and the literature on this topic are still scarce. Five cases of the PTC approach were reported with promising results; three of them were performed after Roux-en-Y HJ. In this series, just as in our case, PTC was performed given the unsuccess of the endoscopic approach - the first-line therapy for HJ dilatation [5]. PTC can offer both diagnostic and therapeutic options such as evaluation of biliary strictures, biopsies, lithotripsy, biliary stones removal, and also allow complete cleaning of the biliary ducts. Furthermore, as in the case we describe herein, in patients with a high lithiasis load, the endoscopic approach may not be feasible to achieve a complete intrahepatic clearance of stones. To the best of our knowledge, this is the first case using PTC for intrahepatic biliary lithiasis described in the Portuguese literature.














