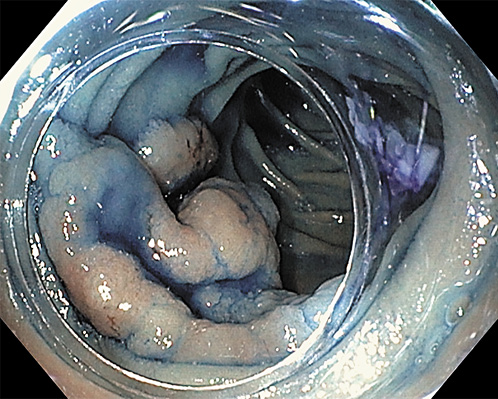
A 64-year-old woman, without relevant medical history, was referred to our department due to a 5-cm adenoma in the distal part of the second portion of the duodenum (Fig. 1). Due to the instability of the endoscope, the lesion size and localization, a complete resection by piecemeal-EMR was unlikely. Therefore, ESD was offered.
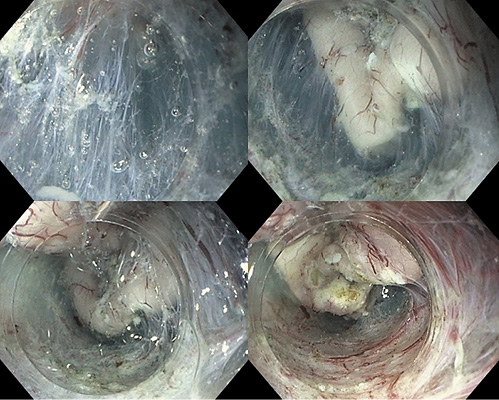
We used hydroxyethylamide with methylene blue for submucosal injection, and dual- and IT-nano knives (Olympus, Tokyo) for submucosal dissection. We started in the oral side by a small incision in the mucosa and then performed underwater ESD using a total of nearly 1 L of saline, creating a pocket beneath the lesion, with the uneventful en bloc resection of the entire lesion.
One of the major challenges in duodenal ESD is the absence of the contraction of the lesion after mucosal incision, which prevents an easy access to submucosa; at the same time, the muscle layer is very thin and the submucosal injection does not last long. Underwater technique allowed us to have an easier access to the submucosa, by pushing the mucosal flap away from the scope, and providing a clean visualization during the entire procedure. Once in the submucosa, pocket technique [1] allowed us to have a better scope stabilization throughout the procedure (Fig. 2); after dissecting the submucosa, we finished by cutting the remaining mucosa circularly.
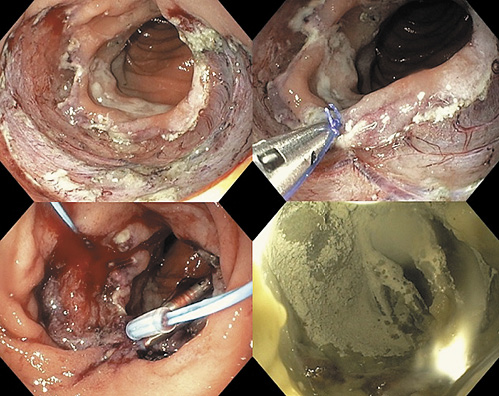
Besides the high-risk of adverse events during the procedure, duodenal ESD has a high risk of late adverse events, due to the exposure of the muscular layer to biliary and pancreatic juices. Therefore, we attempted to close the defect by the string-clip suturing method [2]. First, a clip with a string was passed into the endoscopic channel and displaced in the anal side of the ulcer. Then, a second clip was hooked in the string and displaced in the opposite (oral) side, and the two clips were gathered by pulling the string. After approaching the two margins, we tried to achieve the complete closure. Unfortunately, we were only able to close half of the defect, due to the poor mobility of the duodenum. In order to offer some protection to the muscle layer, we decided to prophylactically apply hemospray in the open area of the ulcer (Fig. 3).
The lesion measured 60 × 40 mm and the procedure took 150 min. The patient was admitted to the hospital and stayed there for 1 week to address possible late adverse events related to the inability of complete closure of the defect, with double-dose proton pump inhibitor, that maintained for 8 weeks, and a stepwise progression to a normal diet. No late adverse events were observed.
Histological evaluation showed a high-grade dysplastic lesion, with free margins. Follow-up endoscopy showed a scar with some regenerative tissue; biopsies confirmed the absence of dysplasia.
Duodenal submucosal dissection has, in the West, limited indications due to the high rate of adverse events [3]. No previous Portuguese ESD series included underwater duodenal ESD [4-7]. However, when EMR is not possible, and considering the potentially aggressive surgeries, this can be attempted by experienced endoscopists in ESD.