Case Report
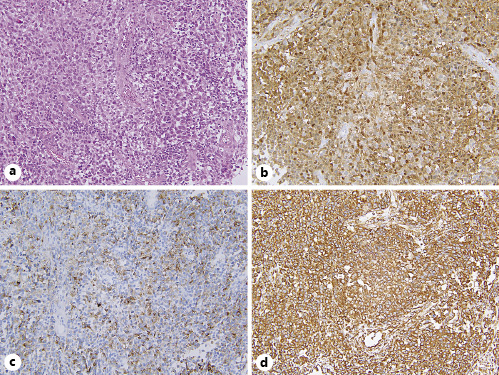
A 65-year-old man presented with a 3 months’ history of hematochezia and anal pain. Digital examination revealed a firm rectal mass. Laboratory examination revealed hemoglobin of 12.9 g/dL (normal range, 13.7-16.8 g/dL). Colonoscopy showed an anorectal tumor involving the distal 3 cm of the rectum, suggesting adenocarcinoma (Fig. 1). Endoscopic biopsies showed a round cell tumor without melanin pigmentation (Fig. 2a). Immunohistopathological examinations disclosed positive findings for S-100 (Fig. 2b), human melanin black-45 (Fig. 2c), and vimentin (Fig. 2d). A diagnosis of anorectal amelanotic melanoma was made. Computed tomography scans and positron emission tomography images disclosed multiple metastatic lesions in the lungs and liver. The patient was informed about chemotherapy options and prognosis of stage IV melanoma but refused undergoing chemotherapy. Best supportive care was offered, and the patient died 4 months later.
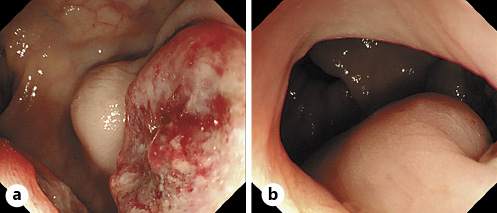
Fig. 1 Colonoscopic images of the tumor. a An ulcerated mass with submucosal invasion in the rectum. b Subepithelial invasion to the anal canal.
Discussion
Anorectal amelanotic melanoma is an extremely rare disease [1]. As amelanotic melanoma has few melanin granules, it is not easy to differentiate it from various anorectal tumors, such as adenocarcinoma, squamous cell carcinoma, lymphoma, and gastrointestinal stromal tumor. Therefore, immunostaining, as shown in this case, is the key for the definite diagnosis [1, 2]. The prognosis of anorectal melanoma remains poor, as most cases have lymph node or distal metastasis at the time of diagnosis. Although surgery remains the optimal treatment option, it is regarded as a palliative procedure, making no significant improvement in overall survival [3]. Conventionally, cytotoxic agents, such as dacarbazine and cisplatin, have been applied to stage IV melanoma, with little improvement of prognosis [2, 3]. Recent development of immunotherapy including immune-check point inhibitors, such as nivolumab and pembrolizumab, have improved the prognosis of this highly lethal malignancy [2, 3]