We present the case of a 52-year-old male with a past medical history of double-lung transplantation in the context of alpha-1 antitrypsin deficiency, complicated by chronic lung allograft dysfunction (bronchiolitis oblite rans syndrome), and two perianal interventions (fistulotomy and hemorrhoidectomy) 5 years before. The patient was admitted to our hospital due to acute-on-chronic respiratory failure as a result of respiratory infection.
In the intermediate care unit, he started noninvasive ventilation, broad-spectrum antibiotherapy, and thromboprophylactic enoxaparin 40 mg daily. Due to constipation, even taking osmotic laxatives, daily docusate sodium and sorbitol enemas were initiated as well. Five days later, the patient had new-onset rectal bleeding, without abdominal or anal pain. Laboratory data showed a hemoglobin level of 6.4 g/dL. He required intravenous fluids and blood transfusions for resuscitation. Due to persistent rectal bleeding with associated hemodynamic instability, a flexible sigmoidoscopy was performed after cleansing enema administration.
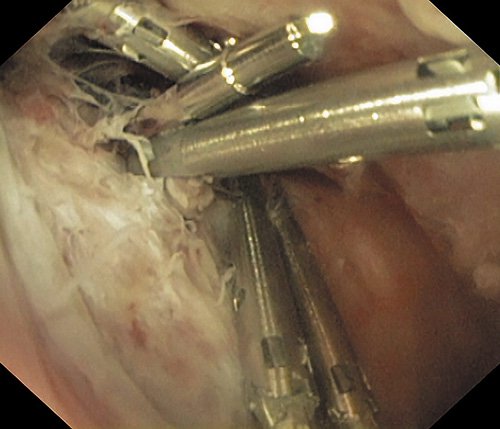
An extensive tear of the distal rectum with exposure of the muscular layer was evident (Fig. 1a), as well as two fistula openings with many clots and associated spurting bleeding (Fig. 1b). Hemostasis was achieved after the injection of 9 mL of diluted adrenaline (1:10,000) and placement of 6 hemoclips (Fig. 2). Computed tomography angiography was performed immediately after the procedure, which showed parietal thickening of the terminal portion of the rectum, with associated fistulous tracts containing gas (Fig. 3). There was no evidence of active bleeding, perforation, or intra-abdominal collections. No further episodes of bleeding occurred after endoscopic therapy. However, the respiratory failure gradually worsened and the patient was refused for retransplantation. He died a week later.
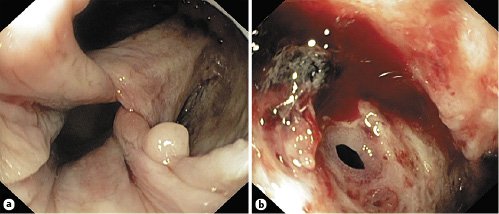
Fig. 1: Flexible sigmoidoscopy revealing an extensive rectal tear (a) and two fistula openings (b) in the area of ulceration, with associated active spurting bleeding.

Fig. 3: Coronal (a) and axial (b) view by abdominopelvic computed tomography angiography revealing parietal thickening of the distal rectum with associated fistulous tracts containing gas (arrows) and adjacent high-density material related to previous clip application.
Besides the previous perianal interventions, there was no history of recent trauma, anal intercourse, or endoscopic or surgical procedures. Therefore, the rectal tear was probably caused by the administration of a cleansing enema to a debilitated patient with reduced complaints of discomfort during the procedure, facilitated by premorbid perianal pathologies and chronic constipation. In fact, injuries to the anorectum, such as perforations, fistulae, and rectal burn, have already been described after enema administration [1-4]. Additionally, severe lower gastrointestinal bleeding has also been reported. The severity of the rectal bleeding can be explained by exposure of a submucosal vessel due to the rectal tear and the inpatient anticoagulation that was started on admission.
Cleansing enemas are widely used, especially in the treatment of chronic constipation. In the majority of cases, they produce the desired effect without any accompanying problems. However, the administration of a cleansing enema is not a risk-free procedure. Careless enema application, long rigid tips, and extant anorectal pathology have all been implicated as factors contributing to rectal injuries [1]. Therefore, any pre-existing perianal pathology must be identified, complaints of pain during the procedure require special attention, and oral laxatives may be preferred.
We reported a case of rectal tear with associated severe lower gastrointestinal bleeding, a potentially life-threatening complication of enema administration. This case emphasizes the need for careful application of enemas and highlights the importance of endoscopy as a potentially successful treatment of severe rectal bleeding.