Introduction
Acute liver failure (ALF) describes a new (no previous cirrhosis) and rapidly evolving (≤26 weeks) liver dysfunction associated with neurologic dysfunction (hepatic encephalopathy [HE]) and coagulopathy (international normalized ratio [INR] ≥1.5) (1-3). It is a rare disease with a hospital survival rate of about 60% (1). This has been improving over the past decades due to earlier diagnosis, timely transfer to specialized centers, better management in the intensive care unit (ICU), and developments in emergency liver transplantation (ELT) (1, 2).
The clinical course of ALF depends on etiology, time from disease onset to the development of HE, and the timely diagnosis and treatment of ensuing organ failure (3, 4). ELT is the definitive treatment for patients with ALF when the potential to regenerate liver function and survival are predicted to be poor (5).
Reports on ALF epidemiology and outcomes have documented regional variability (6-8). We hypothesized that the approach to ALF in different ICUs could vary substantially. We performed a survey to characterize the approach to ALF by ICU professionals. We aimed to identify points of care that could be improved, educational goals to be enforced, and research topics to be prioritized.
Methods
This study was endorsed by the European Society of Intensive Care Medicine (ESICM). Participation was voluntary and consent implied by its completion.
Study Design, Setting, and Participants
We performed a cross-sectional survey aimed at examining current practice on ALF by ICU professionals worldwide, including physicians and nurses. The survey was conducted between November 2018 and June 2019.
Survey Development and Implementation
The survey content was based on literature about ALF (9-12) and comprised questions (online supplementary file 1, for all suppl. material, see www.karger.com/doi/10.1159/000516672) on the demographics of ICU professionals (7 questions), the characterization of patients with ALF admitted to ICU (5 questions), and management of patients (13 questions). All questions were given specific options for answers, with 10 having possible multiple answers and 15 an optional free text response (13). The survey was reviewed by authors and reviewers of the ESICM Research Committee. It underwent pilot-testing in the ICU at CCH to assess comprehension, feasibility, redundancy, and consistency (14).
The survey was created using a Web-based platform (SurveyMonkey®) by ESICM staff and implemented and promoted via the ESICM website (https://www.esicm.org/research/surveys/#ALFinICU). All respondents were ESICM website spontaneous visitors.
Statistical Analysis
Continuous and categorical variables were reported as median (interquartile range) and n (%), respectively. Missing data across all variables were 1.9%, so no imputation was performed.
Univariate comparisons were performed using the Mann-Whitney U/Kruskal-Wallis test or χ2/Fisher test where appropriate. Statistical significance was defined as p < 0.05 (2-tailed). Statistical analysis was performed using SPSS v20 (IBM Corp., North Castle, NY, USA).
Results
Demographics of Participants
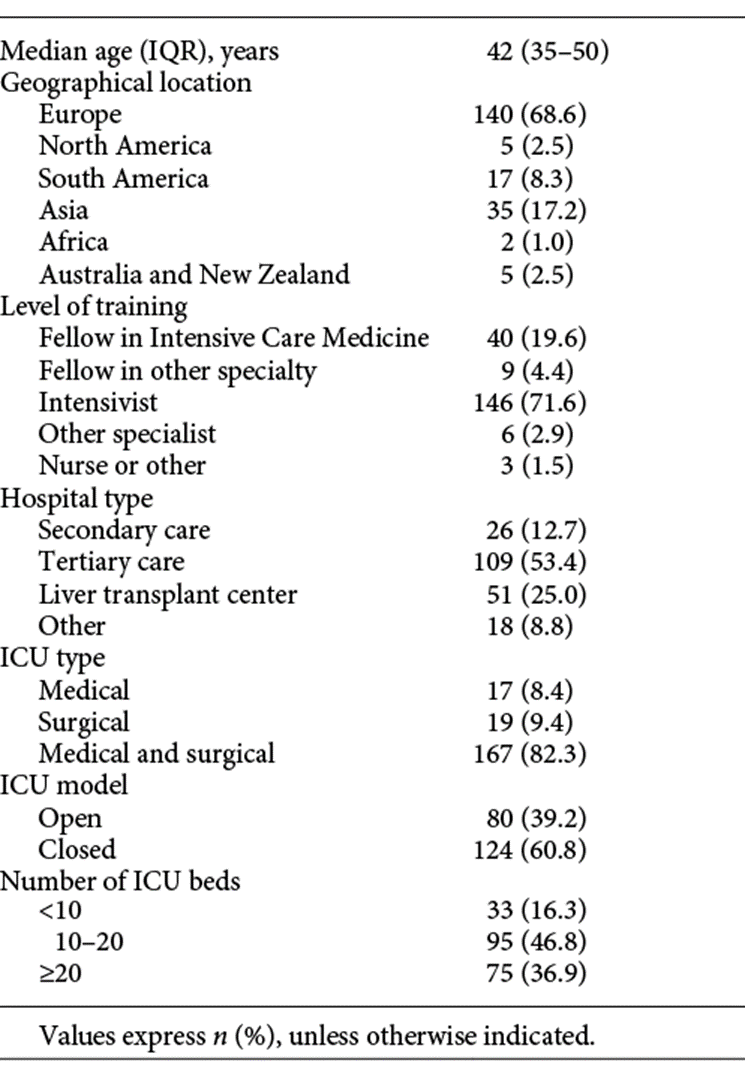
A total of 204 participants completed the survey in a median 7 (IQR 5-10) min. Median age was 42 (IQR 35-50) years, with 140 (68.6%) working in European countries (online suppl. file 2) and 146 (71.6%) as certified intensivists (Table 1). Regarding the hospital setting, 160 (78.4%) worked in tertiary care hospitals (51 25.0% with ELT) and 167 (82.3%) in medical and surgical ICUs (Table 1).
Characteristics of Patients with ALF Admitted to the ICU
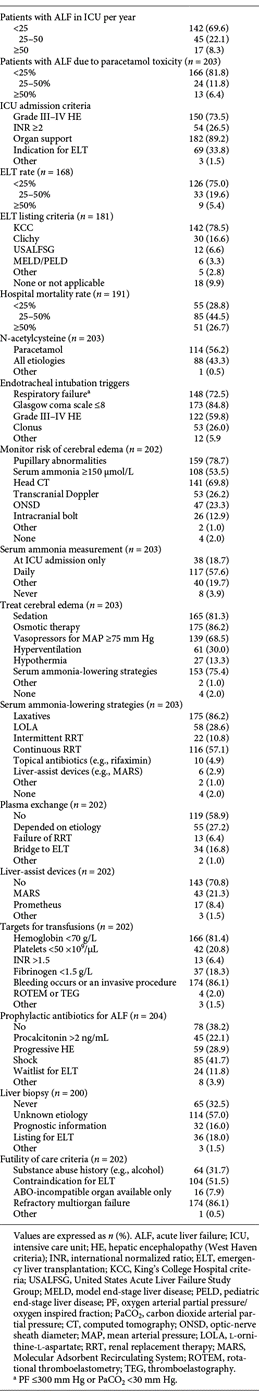
Of the respondents, 142 (69.6%) worked in ICUs admitting <25 patients with ALF per year, with 166 (81.8%) reporting that <25% of the cases were due to paracetamol toxicity (Table 2). The most frequent reasons for admitting patients with ALF to the ICU were: the need for organ support (89.2%), West Haven criteria grade III-IV HE (73.5%), a potential indication for ELT (33.8%), or an INR ≥2 (26.5%).
In total, 126 (75.0%) reported that ELT was performed in <25% of patients with ALF, with 142 (78.5%) using the King’s College Hospital criteria (KCC) for ELT listing. In terms of mortality, 140 (73.3%) estimated a hospital mortality rate <50% for their patients with ALF.
Management of Patients with ALF in the ICU
Eighty-eight (43.3%) reported prescribing N-acetylcysteine (NAC) for all etiologies of ALF (Table 2). As for the triggers used for endotracheal intubation (ETI), the most common were coma (84.8%), respiratory failure (72.5%), and grade III-IV HE (59.8%).
In terms of monitoring the risk of cerebral edema, the most frequent indicators used were pupillary abnormalities (78.7%), head computed tomography (CT; 69.8%), or serum ammonia (53.5%). Regarding serum ammonia, 117 (57.6%) performed daily measurements.
Concerning the treatment of cerebral edema, the most common interventions used were osmotic therapy (86.2%), sedation (81.3%), serum ammonia-lowering strategies (75.4%), and vasopressors (68.5%).
The most frequent serum ammonia-lowering strategies used were laxatives (86.2%), continuous renal replacement therapy (CRRT; 57.1%), or L-ornithine-L-aspartate (LOLA; 28.6%). As for other extracorporeal devices, 83 (41.1%) used plasma exchange and 59 (29.2%) used liver-assist devices (e.g., Molecular Adsorbent Recirculating System).
The most common thresholds used for transfusing blood products were bleeding or invasive procedure (86.1%), hemoglobin <70 g/L (81.4%), platelets <50 × 109/µL (20.8%), and fibrinogen <1.5 g/L (18.3%).
One hundred and twenty-six (61.8%) used prophylactic antibiotics for ALF with specific triggers, namely, shock (41.7%), progressive HE (28.9%), and procalcitonin >2 ng/mL (22.1%).
Liver biopsy was reported to be requested by 135 (67.5%) respondents, especially in cases of unknown etiology (57.0%), for ELT listing (18.0%), or for prognosis (16.0%).
The most prevalent criteria regarding futility of care were refractory multiorgan failure (86.1%), contraindication for ELT (51.5%), or a history of substance abuse (e.g., alcohol; 31.7%).
Management of Patients with ALF in the ICU: Study of Associations
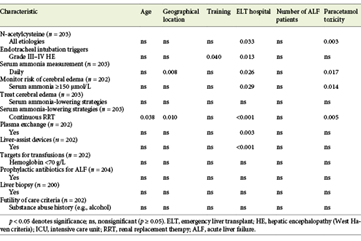
The prescription of NAC for all etiologies of ALF was more frequent in respondents that admitted a higher number of patients with paracetamol toxicity (Table 3: 38.8% if <25% admitted vs. 54.2% if 25-50% admitted vs. 76.9% if ≥50% admitted; p = 0.003) and those working at ELT centers (58.8 vs. other 38.2%; p = 0.033).
ETI for grade III-IV HE was more common among fellows of intensive care medicine or intensivists (ICU 67.5 vs. other 33.3%; intensivists 61.6 vs. other 22.2%; p = 0.040) and those working at ELT centers (74.5 vs. other 54.9%; p = 0.013).
Daily serum ammonia measurements were more frequently performed by individuals from North America (Europe 62.6% vs. North America 80.0% vs. other 44.1%; p = 0.008), those that admitted a lower number of patients with paracetamol toxicity (59.4% if <25% admitted vs. 45.8% if 25-50% admitted vs. 53.8% if ≥50% admitted; p = 0.017), and those working at ELT centers (ELT center 74.5% vs. other 52.0%; p = 0.026). The use of a serum ammonia level ≥150 µmol/L to monitor the risk of cerebral edema was more common among participants that admitted a higher number of patients with paracetamol toxicity (50.6% if <25% admitted vs. 50.0% if 25-50% admitted vs. 92.3% if ≥50% admitted; p = 0.014) and those working at ELT centers (ELT center 66.7% vs. other 49.0%; p = 0.029).
The use of CRRT to decrease serum ammonia was more frequent among older respondents (44 vs. 39 years; p = 0.038), those from North America (Europe 64.7% vs. North America 80.0% vs. other 37.3%; p = 0.010), those working at ELT centers (ELT center 78.4% vs. other 50.0%; p < 0.001), and those that admitted a higher number of patients with paracetamol toxicity (52.1% if <25% admitted vs. 79.2% if 25-50% admitted vs. 84.5% if ≥50% admitted; p = 0.005).
The use of plasma exchange (ELT center 58.8% vs. other 35.1%; p = 0.003) or liver-assist devices (ELT center 56.9% vs. other 19.9%; p < 0.001) was more common among individuals working at ELT centers.
The prescription of prophylactic antibiotics was more frequently made by those working in secondary care hospitals (secondary care 76.9% vs. tertiary care 61.5% vs. ELT center 64.7%; p = 0.031).
Discussion
Key Results and Comparisons with the Previous Literature
The majority of individuals admitted <25 patients with ALF per year (69.6%) and <25% had paracetamol toxicity (81.8%). The incidence of ALF is ≤10 cases per million people per year in developed countries, so only ELT centers within highly populated areas may treat a high volume of cases (4). In the UK, North America, and Australia/New Zealand, paracetamol overdose has been the leading etiology of ALF (1, 2, 15). In continental Europe, the most common causes of ALF have been non-paracetamol drug-induced liver injury, seronegative liver injury, and hepatitis B (8, 16, 17). Consequently, ICU professionals outside the UK, North America, and Australia/New Zealand (>80.0%) are expected to deal mostly with non-paracetamol ALF.
Most of the respondents reported an ELT rate <25% (75.0%) and an in-hospital mortality rate <50% (73.3%). As the majority admitted patients with non-paracetamol ALF, we would have expected a higher ELT rate. Although the decision to list patients with ALF for ELT is complex, clinicians have been relying more on prognostic systems, such as the KCC (78.5%), to select patients for ELT. However, jurisdiction-specific legislation on organ donation may have influenced organ availability in different regions. Nevertheless, the in-hospital mortality rate reported by the majority of the participants was comparable to the literature (1, 8, 16-19). This suggests that patients are being better managed with medical treatment alone.
A minority prescribed NAC for all etiologies of ALF (43.3%); this was more frequent among ICU professionals working with a higher volume of patients with paracetamol toxicity or at ELT centers. NAC is the antidote for paracetamol toxicity via its action of replenishing glutathione, a crucial molecule for paracetamol detoxification in the liver (20). However, NAC has also improved transplant-free survival in patients with non-paracetamol ALF (21). This may be related to its improvement of hemodynamics and oxygen use or the decrease in the risk of cerebral edema (22, 23). Therefore, current management of ALF should consider prescribing NAC for all etiologies of ALF (9, 10, 21, 24).
Around 59.8% respondents intubated patients with ALF due to grade III-IV HE, with this being more common among intensive care fellows, intensivists, and ICU professionals from ELT centers. Patients with ALF may be at risk of developing cerebral edema due to astrocyte swelling, a complex process in which ammonia and lactate are involved (25). ETI for grade III-IV HE is recommended to prevent aspiration and allow for the early treatment of cerebral edema (11, 12).
The majority of respondents monitored the risk of cerebral edema using pupillary abnormalities (78.7%), head CT (69.8%), or serum ammonia (53.5%), with a minority using transcranial Doppler (TCD; 26.2%), optic-nerve sheath diameter (ONSD; 23.3%), or intracranial bolt (12.9%). Frequent pupillary exam is mandatory to detect signs of intracranial hypertension. Moreover, these signs present often late on head CT. TCD or ONSD still lack validation in ALF (26). Measurement of intracranial pressure with a bolt may be useful but its effect on patients’ outcomes has been controversial (27). Therefore, even if the prevalence of cerebral edema in ALF has been decreasing over the past decades, a coherent strategy to monitor the risk of intracranial hypertension (ICH) is still lacking (28).
Hyperammonemia (≥150 µmol/L) has been associated with an increased risk of ICH, so frequent measurement may help to prevent this (29). However, only 57.6% of the respondents measured serum ammonia daily, this being more frequent among ICU professionals working with a higher volume of patients with paracetamol toxicity or at ELT centers. Frequent measurement of arterial blood ammonia should be further encouraged as a means to monitor the risk of developing neurological complications (9, 11).
To lower serum ammonia, the majority of the respondents administered laxatives (86.2%) or CRRT (57.1%). A minority used LOLA (28.6%), intermittent renal replacement therapy (IRRT; 10.8%), topical antibiotics (4.9%), or liver-assist devices (2.9%). In ALF, while lactulose may reduce ammonia, time to effect is long and there is the added risk of bowel distention (30-34). The case for LOLA or topical antibiotics still lacks evidence, and they are also frequently unavailable (11, 12, 35). CRRT, more frequently used by older ICU professionals and those from North America, working at ELT centers, or admitting a higher volume of patients with paracetamol toxicity, has been shown to decrease serum ammonia and improve survival, effects that are lacking with IRRT (36).
Liver-assist devices were used by 29.2% of the respondents for ALF, this being more common among ICU professionals at ELT centers. In fact, the case for use of these devices still lacks evidence (37). Plasma exchange for ALF was performed by 41.1% of all respondents, also mainly ICU professionals at ELT centers. While there is evidence to support the use of plasma exchange, the timing, dose, and interaction with ELT listing decisions remain uncertain (38).
Regarding the use of extracorporeal devices, CRRT should be the first option to treat metabolic imbalance and control hyperammonemia (36). For patients with ALF progressing to multiorgan failure, especially with high-dose vasopressors or if ELT is not an option, plasma exchange may be considered (39).
The majority of respondents prescribed prophylactic antibiotics for ALF (61.8%), with this being more common among ICU professionals from secondary care hospitals. In ALF, prophylactic antibiotics have not been found to improve survival (40). However, the development of grade III-IV HE or systemic inflammatory response syndrome has been associated with infection and worse outcomes (41, 42). Therefore, high clinical suspicion and frequent screening for sepsis remain fundamental to initiate antimicrobials (11, 12).
The majority of participants requested liver biopsy for patients with ALF (67.5%). Often, liver biopsy does not provide information about etiology due to sample error, or else the extent of necrosis precludes a thorough evaluation. It may help to exclude cirrhosis, alcoholic hepatitis, or malignancy (43, 44). Furthermore, submassive or massive patterns of necrosis have been associated with a lower likelihood of liver function regeneration (45). Therefore, liver biopsy remains a controversial intervention in ALF.
The majority of respondents considered refractory multiorgan failure (86.1%) or contraindication for liver transplant (51.5%) as criteria for futility of care. A small number also accepted substance abuse history (31.7%) or ABO-incompatible organ availability (7.9%). It seems reasonable that patients with ALF and multiorgan failure unresponsive to treatment may be considered for end-of-life discussions. Deciding contraindications for ELT is often complex. Psychosocial factors such as mental health, substance dependence, or presumed compliance with treatment are difficult to assess in an acute context. Therefore, comprehensive case-specific discussion within a multidisciplinary team is likely the best course of action (11). Regarding ABO-incompatible ELT, these patients can show worse outcomes, but this intervention may, at times, be their only chance of survival (46, 47). Overall, decisions about futility of care in ALF still lack evidence.
Limitations
Our study has the following limitations that warrant consideration. Firstly, while our survey underwent pilot testing, this was a novel online instrument of research in ALF. Secondly, as it was implemented via the ESICM website, this may have contributed to selection bias, as ESICM members or frequent online visitors were more likely to respond to it. Thirdly, the survey relied on answers from individuals, which may have led to recall bias or other types of response bias. Despite these limitations, we consider that our findings may help to identify points-of-care reflected in recent guidelines that may benefit from further education and research activities (11, 12). Although many diagnostic and therapeutic interventions in ALF still lack high-quality evidence, professionals from ELT centers seem to have implemented more of such recommend interventions. Cross-collaboration between referral and ELT centers may therefore continue to be one way to enforce better management of patients with ALF.