Introduction
Choledocholithiasis is estimated to be seen in 1-15% of patients with cholelithiasis [1, 2]. The prevalence of choledocholithiasis was found to be 9.6 % in southern India [3]. The prevalence of cholelithiasis during pregnancy varies in different population settings, with some studies showing a prevalence of 1% and others showing a prevalence as high as 5% [4, 5]. The appropriate treatment depends on the size of the stones, the patient’s choice, and the symptoms. Endoscopic retrograde cholangiopancreatography (ERCP) is the treatment of choice for choledocholithiasis in the nonpregnant population [6, 7]. It is useful in pregnant patients and has a high level of technical success in clearing the common bile duct of gallstones, with very low rates of maternal and fetal complications [8, 9]. Recently, the SpyGlassTM DS II Access and Delivery Catheter (Boston Scientific, Marlborough, MA, USA) was developed with an increased resolution and high-dynamic range processing for improved visibility. This device has been successfully used to treat choledocholithiasis in a pregnant woman [10]. However, the utility of this device in choledocholithiasis among pregnant woman remains explored to a lesser extent.
Methods
This is a retrospective analysis of prospectively collected data of patients who underwent ERCP procedures at a single tertiary care referral center from October 2019 to November 2020. Patient records were reviewed for indication, endoscopic interventions, post-procedure complications, and outcomes.
Choledocholithiasis was assessed in all patients with a radiological modality - endoscopic ultrasound or magnetic resonance cholangiopancreatography (MRCP). All of the patients had previously undergone routine laboratory investigations including liver and renal parameters. The procedures were done by two senior endoscopists. A senior anesthesiologist was always present during the procedures. All of the patients received total intravenous anesthesia. All of the patients were maintained nil per os for 8 h. After written informed consent, endoscopic procedures were performed using the duodenoscope (TJF-160R; Olympus, Japan) in the left lateral position. CBD was selectively cannulated by insertion of a hydrophilic guidewire (0.032-in J Angled Tip; Terumo Medical Corp., USA) and confirmed by aspiration of bile. Biliary endoscopic sphincterotomy was done by cutting the ampulla at 11 o’clock. A SpyScopeTM (Boston Scientific) was used to visualize the common bile duct and the cystic duct. The cholangioscope was advanced over a guidewire (Dreamwire; Boston Scientific) into the bile duct wherein intraductal stones were identified. Depending on the size and location of the stones, we used 3 different modalities. Holmium LL (Medilas H20; Dornier Medtech, Munich, Germany) was delivered via a 365-µm-diameter fiber, with energy levels set at 800-1,500 mJ at a frequency of 8-15 Hz, for large impacted stones; the balloon extraction technique (Extractor Pro; Boston Scientific) was used for multiple stones wherein the duct was adequately dilated, and the SpyGlass retrieval basket (286 cm × 15 mm; Boston Scientific) was used for single solitary stones. The retrieval basket was passed just proximal to the stone and then opened. Upon distal withdrawal of the cholangioscope, the stones were easily captured in the retrieval basket. The SpyScope and the basket were then retrieved into the duodenum (Fig. 1a-f ). A prophylactic 7-Fr plastic stent was placed in all of the patients. All of the procedures were uneventful. In patients with biliary pancreatitis, procedures were performed between 72-96 h after the onset of pain. The patients were managed as per the appropriate guidelines [11]. All of the patients received intravenous antibiotics (Cefotaxime at 1,000 mg) prior to the procedure. Oral antibiotics (Cefixime at 200 mg b.i.d.) were continued for 5 days in patients with cholangitis. All of the patients were discharged after 24-48 h of observation. These patients subsequently underwent laparoscopic cholecystectomy. Stent removal was performed after 2 weeks of laparoscopic cholecystectomy.
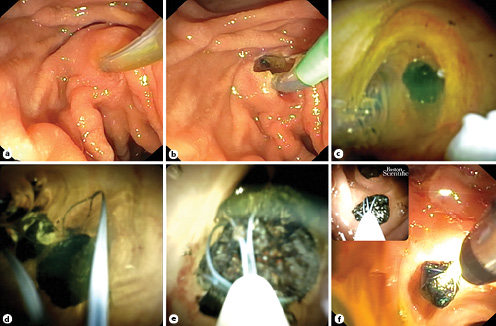
SpyGlass retrieval basket passed just proximal to the common bile duct stone. e Common bile duct stones were easily captured in the retrieval basket. f Common bile duct stones were then retrieved into the duodenum.
The demographics of all of the patients undergoing endoscopic procedures were entered into Excel (Office 2019 Professional for Windows; Microsoft). The statistical analysis was performed using the IBM Statistical Package for the Social Sciences (SPSS) Statistics for Windows (version 23.0, Professional; IBM Corp., Armonk, NY, USA). Categorical variables were reported as frequency and percentages. For continuous variables, descriptive statistics were used.
Results
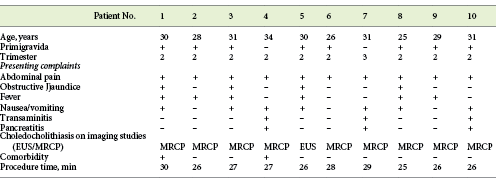
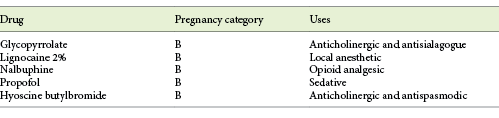
A total of 10 (100% female) patients underwent ERCP with a mean (±SD) age of 29.5 (±2.5) years (Table 1). Abdominal pain was the commonest presenting symptom in all of the patients. Four (40%) patients had cholangitis and 3 (30%) had pancreatitis. The majority of the patients (9; 90%) were in the second trimester. MRCP was the commonest radiological entity, used in 9 (90%) patients. Two patients had premorbidities; 1 had type 2 diabetes mellitus and the other had hypertension. Premorbidity medications were continued in these patients. All of the anesthetic agents used for ERCP in pregnancy were pregnancy risk category B (Table 2). Stones were present in CBD in 7 (70%) patients (largest: 1.5 cm) and in the cystic duct in 3 (30%) patients (largest: 0.8 cm). ERCP was technically successful in all of the patients. Stones were removed from all of the patients in a mean (±SD) time of 30 (±3.5) min. LL was used successfully in 4 (40%) patients, balloon extraction in 3 (30%), and SpyGlass retrieval basket in 3 (30%). There were no pre- or postprocedural complications. The pre- and postprocedural fetal heart sounds were normal. All of the patients had an uneventful childbirth at term, after which they underwent cholecystectomy and subsequent stent removal two weeks later.
Discussion
By retrospectively analyzing cases of pregnant woman who underwent ERCP for choledocholithiasis without fluoroscopy, we found that extraction of stones with the SpyScope and the retrieval basket is feasible. The first series of ERCP in pregnancy for choledocholithiasis was published in 1990. ERCP has been routinely performed with minimal complications [12]. The majority of births after therapeutic ERCP are full term and have been found to be healthy [13].
ERCP in the usual population is performed with the patient in the prone position. However, this position should be avoided in pregnancy [14]. The choice of medication may need to be altered during pregnancy, as certain medications may pose an additional risk to the fetus. Indomethacin/diclofenac suppositories are category C drugs and hence were not used in our patients. Propofol is considered the safest and hence was used in these patients. Glycopyrrolate negates bradycardia induced by propofol and also serves as an antisialagogue. Lignocaine reduces the pain associated with propofol intravenous injection, reduces the cough reflex, and prevents laryngospasm. Hyoscine butylbromide was used to reduce duodenal contractions. Nalbuphine was used as an opioid analgesic. Cefotaxime had been used as a prophylactic antibiotic. The second trimester is considered safer for elective ERCP procedures. The majority of our patients were in the second trimester, with 1 patient at the beginning of the third trimester. An experienced endoscopist minimizes the overall procedural time, thereby reducing the anesthesia dosages. The study site has an experienced endoscopist with more than 30 years of experience and an experienced senior anesthesiologist. The site is a high-volume center for ERCP procedures, and enough studies for single-operator cholangioscopy-guided laser lithotripsy (LL) for CBD and cystic stones have been routinely performed [15,16,17]. All of these factors including appropriate patient selection could be possible reasons for the absence of complications in these patients.
MRCP is a useful radio imaging tool for detection of choledocholithiasis, with a reported sensitivity of 93% [18]. EUS is invasive but safe [19], though it increases the overall cost of the procedure and requires adequate expertise. EUS does help to assess the CBD diameter and the number and size of gall stones. MRCP was commonly used and was very useful among our patients. Endosonography was used in the diagnosis of 1 patient since MRCP was inconclusive. Computed tomography is not recommended in pregnant patients.
In a retrospective study of 65 pregnancies, 11 patients (16%) developed pancreatitis after ERCP. ERCP performed during the first trimester had relatively worse fetal outcomes. Mothers undergoing ERCP during the first trimester had only 73% of deliveries at term [20]. In a series of 20 patients, 1 neonatal death after delivery was reported for a patient who underwent 3 therapeutic ERCP [14]. A systematic review in 2011 showed that ERCP during pregnancy is relatively safe [13]. Among 296 pregnant patients, fetal outcomes were reported in 254 (86%) patients. There were prematurely born infants with a low birth weight in 11 cases, late spontaneous abortions in 3, infant death soon after birth in 2, and a voluntary abortion in 1; the perinatal mortality was about 1% [13]. The risks versus the benefits should be assessed for every patient [21]. For cases which are semiemergencies, it is generally deferred until postpartum.
ERCP can be performed by using a wire-guided cannulation technique without the need for fluoroscopy. Aspiration of bile is used to confirm selective cannulation of the CBD, followed by biliary sphincterotomy and balloon extraction of stones [22]. A standard sphincterotomy was done up to the roof of the ampulla so that a 10-Fr SpyScope catheter could be introduced over the guidewire, but this technique cannot differentiate between cannulation of the cystic and the common hepatic duct. It may be difficult to exclude residual stones or debris. Long, complicated procedures, with impacted, large, or multiple CBD stones, may be difficult to perform in pregnant patients. Biliary stents must be placed for decompression with the intent of repeating the procedure postpartum. With the advent of new generation cholangioscopes, these newer techniques to minimize or even eliminate the use of fluoroscopy should be used in future studies. In patients with cystic duct lithiasis, SpyGlass-guided LL was feasible as the cystic duct was dilated (but not tortuous), which allowed easy passage of the SpyGlass system and LL to be carried out.
The present study does have some inherent limitations. First, the results are from a single center, and it has a small sample size and a retrospective design. The results may not be generalizable outside of this environment. An element of selection bias may be present. The patient details were available only up to 2 months post-delivery. Nevertheless, this study has laid a foundation for future studies and can act as a reference.
To summarize, the use of the SpyGlass DS II system during ERCP appears to be safe and effective for the treatment of choledocholithiasis among pregnant woman with birth at full-term. SpyGlass does seem to be a good prospect for future research. There remains a need for the study results to be reproduced in prospective trials.