Bile duct adenomas are a very rare entity, mostly located in the gallbladder and incidentally found in surgical specimens; however, they can be detected in any segment of the biliary tree [1]. The natural history of these lesions is not well established but is postulated to be similar to the adenoma-adenocarcinoma sequence existing elsewhere in the gastrointestinal tract [2].
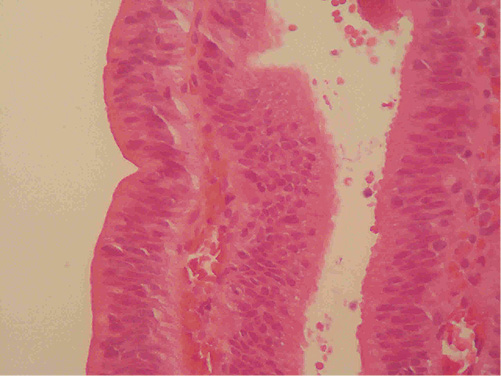
We present the case of an 87-year-old man with a history of two episodes of acute pancreatitis, with a 3-month interval between them, referred for upper endoscopic ultrasound. This study showed a 15 × 10 mm isoechoic image in the terminal portion of the common bile duct (CBD), with a heterogeneous aspect and no acoustic shadowing (Fig. 1). A subsequent endoscopic retrograde cholangiopancreatography (ERCP) was performed, revealing an enlarged and bulging papilla, with normal overlying mucosa (Fig. 2a). The cholangiogram revealed a filling defect in the distal third of the CBD, approximately 20 mm in diameter, compatible with a bile duct stone (Fig. 2b). After biliary sphincterotomy, a biliary sweepage was performed using a Dormia basket revealing a villous polypoid lesion of about 20 mm extruding from the bile duct into the duodenum (Fig. 2c). Biopsies were taken and confirmed it to be a villous adenoma with low-grade dysplasia (Fig. 3). Given the patient’s age and comorbidities, surgery was precluded, and resection was performed using a hot snare polypectomy technique, followed by ablation with argon plasma. The etiology of the acute pancreatitis was attributed to the adenoma, after exclusion of more common etiologies (gallstones, alcohol consumption, potential drugs or toxins, triglycerides, hypercalcemia, IgG4 and autoimmune pancreatitis or anatomic anomalies). Given the patient’s age and no relevant family history, genetic etiologies were not investigated.
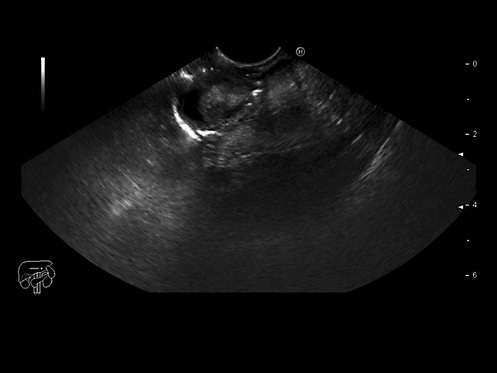
Fig. 1 Echoendoscopic image showing a 15 × 10 mm isoechoic image in the distal CBD with a heterogeneous aspect without shadow cone.
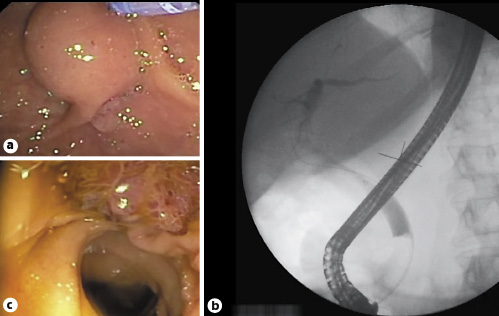
Fig. 2 ERCP images. a Endoscopic view showing a bulging papilla with normal overlying mucosa. b 20-mm filling defect in the distal CBD compatible with a biliary stone. c Biliary sweepage with a Dormia basket revealed a 20-mm villous polypoid lesion emanating from the bile duct into the duodenum.
The patient was lost to follow-up during a 4-year period and was again referred to the Gastroenterology Department because of new-onset jaundice. An ERCP was performed showing adenomatous tissue in the terminal portion of the CBD, and biopsies were compatible with adenoma with low-grade dysplasia. Given the patient’s contraindications for a surgical approach, bipolar radiofrequency (HabibTM) of the adenomatous tissue was performed with technical success. A follow-up ERCP with cholangioscopy is already scheduled.
Adenomas arising from the extrahepatic biliary tree are still poorly understood, mainly because of its very low incidence. Nevertheless, current knowledge supports the belief that these lesions may potentially evolve into carcinomas, like adenomas located elsewhere [1]. Most authors believe that removal of these adenomatous lesions may prevent the development of adenocarcinoma [1-3]. Little is known about the use of radiofrequency in biliary adenomas. In the few published case reports, a surgical approach was used. A minority of patients was maintained in surveillance without invasive treatment due to patients’ risks and poor life expectancy [1].
We highlight this case because of the rarity of this pathology, the presentation as recurrent acute pancreatitis that, to our knowledge, is not described in the small number of case series published [1], and because of the diagnostic challenge it posed.
Consult the ERCP endoscopic video available at the following link: 0