Clinical Case
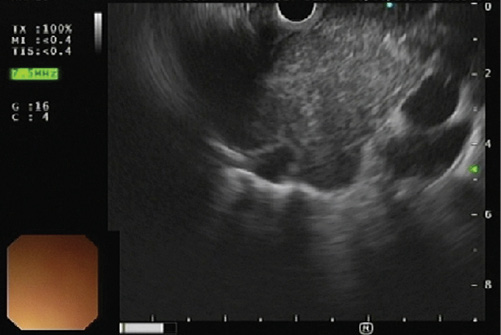
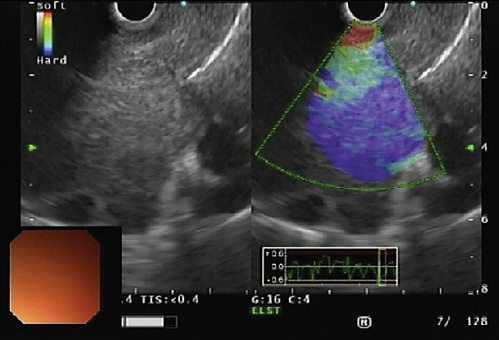
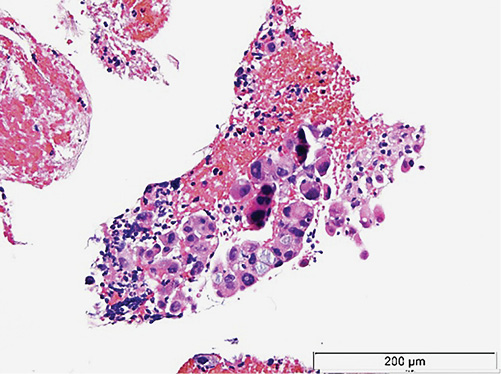
A 55-year-old man, with a past history of alcohol abuse, was admitted to hospital with hemoptysis, hoarseness, dysphagia for solids and anorexia with weight loss, with progressive worsening in the last 2 months. Thoracic computed tomography (CT) scan showed a 9 × 6 × 8-cm homogeneous mass with well-defined borders in the upper mediastinum with extension to the subcarinal region that caused apparent obliteration of the esophageal lumen (Fig. 1). A nodular liver lesion was found in abdominal plans of CT, better characterized by magnetic resonance image (MRI), showing multiple ill-defined nodular lesions in the liver, with hypervascularity and wash-out, leading to the hypothesis of multifocal hepatocellular carcinoma or metastatic lesions of an unknown primary. An upper endoscopy was performed, confirming esophageal extrinsic compression, with normal mucosa. In rigid bronchoscopy, a bilateral endobronchial mass was seen, highly friable, causing reduction of the lumen of the left main bronchus in 70% due to extrinsic compression and mucosal infiltration. Histologically, this lesion was described as compatible with a non-small cell carcinoma, with the expression of citokeratine-7, without a clear definition of its lung origin. Mediastinal radiotherapy was performed to control symptoms, namely hemorrhage. In order to obtain a definite diagnosis of the mediastinal mass, endoscopic ultrasonography (EUS) was performed, showing a hypoechoic and homogeneous mass (Fig. 2), with hypervascular pattern and with a predominantly blue elastographic pattern, suggestive of malignancy (Fig. 3). An EUS-guided fine-needle biopsy was performed (Acquire, 25G, Boston Scientific®); histology showed clusters of malignant cells (Fig. 4), with expression of Hep-par 1, findings that are compatible with metastasis of hepatocellular carcinoma (Fig. 5).~
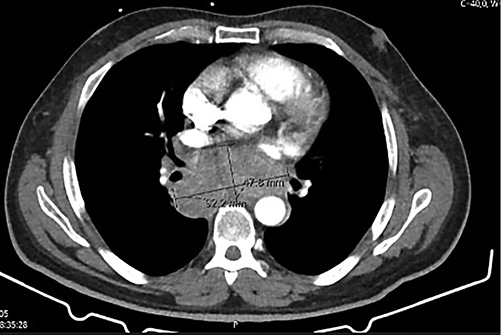
Fig. 1 Thoracic CT scan showing a mediastinal mass with apparent obliteration of the esophageal lumen.
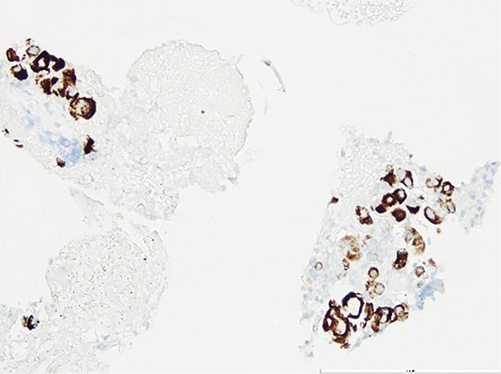
Fig. 5 Immunohistochemical expression of Hep-Par 1, compatible with metastasis of hepatocellular carcinoma.
In view of these findings and in order to stage a potential underlying chronic liver disease, an ultrasound-guided liver biopsy was performed, confirming a liver cirrhosis. Despite the patient had a compensated liver cirrhosis (Child-Pugh A, 6 points), there was a progressive deterioration of functional status that made any type of systemic chemotherapy not viable.
The incidence of endobronchial metastasis from non-pulmonary malignancies ranges from 2 to 50% and usually the breast, kidney, colorectal, uterine cervix, sarcoma and skin origin predominate [1]. When related to hepatocellular carcinoma it is very rare, with an incidence of 0.04% in an advanced stage of the disease, and only 10 cases have been reported in the literature [2].
The definition of endobronchial metastases remains heterogeneous. Kiryu et al. [4] described a classification in 4 types, which was later modified by Akoglu et al. [3]: type I, direct metastasis to the bronchus, type II, bronchial invasion by parenchymal lesions; type III, bronchial invasion by a mediastinal or lymph node metastasis; and type IV, endobronchial invasion with lymphangitis carcinomatosis [3]. Our case represents a type III as we observed an endobronchial invasion by a mediastinal mass representing an HCC metastasis.
Despite endobronchial metastases being a rare presentation of HCC and associated with a poor prognosis, its prompt diagnosis is fundamental, in order to choose the adequate therapy and promote symptomatic relief. In our case, external radiotherapy photon beam was successfully used to re-establish patient airway and hemoptysis resolution.
Nowadays, less invasive techniques than mediastinoscopy, like EUS-guided sample, are recommended to confirm the etiologic diagnosis of mediastinal masses. In this case, EUS had an important role, together with endobronchial biopsies, in determining the origin of the primary tumor. Moreover, the type of needle chosen in this case was due to the hypervascularity of the lesion, in order to minimize potential hemorrhagic complications.
We reported this case due to the rarity of this pattern of HCC presentation as well as to demonstrate the crucial role of EUS in determining the etiology of a mediastinal mass.