Small-cell lung cancer (SCLC) accounts for 15% of all lung cancer cases. It differs from non-SCLC tumors as it displays a neuroendocrine biosignature [1]. Up to two-thirds of SCLC patients present with widespread metastases at diagnosis [1]. Gastric metastases of SCLC are extremely rare and only a small number of reports have been published so far [2].
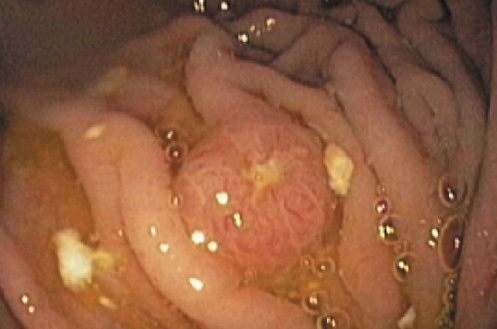
A 47-year-old male patient presented at the emergency department with persistent nonradiating pain in the right hypochondrium, nausea, anorexia, early satiety, and an 11-kg weight loss over 1 month. His past medical history was remarkable for heavy smoking, severe chronic obstructive pulmonary disease, and previous intravenous drugs use. Physical examination revealed painful hepatomegaly. Laboratory values demonstrated a microcytic normochromic anemia (Hb 7.2 g/dL), and elevated cholestasis markers (alkaline phosphatase 254 U/L, gamma-glutamyl transferase 287 U/L). Abdominal ultrasound showed an enlarged and diffusely nodular liver. Thoraco-abdominopelvic CT demonstrated a 2-cm nodule in the inferior lobe of the left lung (Fig. 1a) and signs of diffuse hepatic metastases (Fig. 1b). An upper endoscopy was performed for exploration of his abdominal symptoms and revealed a 1-cm ulcerated nodular lesion in the greater curvature of the gastric body (Fig. 2). Biopsies demonstrated submucosal infiltration of small hyperchromatic cells with scant cytoplasm (Fig. 3a). Immunohistochemistry revealed diffuse immunoreactivity to CAM5.2, synaptophysin, and chromogranin. These findings were compatible with gastric infiltration of neoplastic cells with neuroendocrine differentiation. Liver biopsy was performed and showed similar histology (Fig. 3b, c). Bronchoalveolar lavage cytology and bronchial biopsy revealed TTF-1-positive cells with similar expression of neuroendocrine markers, confirming SCLC. A diagnosis of stage IV SCLC was established, and palliative chemotherapy was initiated. The patient’s functional status rapidly deteriorated, and he died 3 months after the diagnosis.
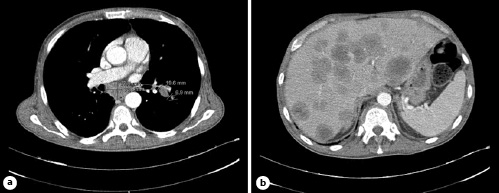
Fig. 1 a CT scan showing a 2-cm nodular lesion in the upper segment of the inferior lobe of the left lung and a 3.7 × 2.4 cm infracarinal adenomegaly. b Hepatomegaly and diffuse hepatic metastases.
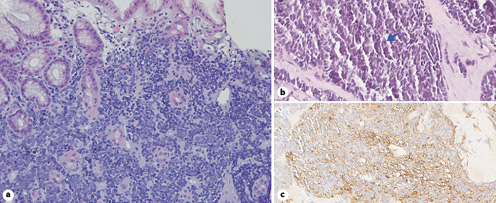
Fig. 3 a Gastric submucosal infiltration of hyperchromatic small neoplastic cells (H&E, ×20). b Liver biopsy demonstrating severe infiltration of liver parenchyma by neoplastic cells, with frequent figures of mitosis (arrow) and apoptosis. c Liver biopsy demonstrating immunohistochemical expression of chromogranin neoplastic cells.
SCLC is an aggressive form of lung cancer known for early dissemination, either lymphatic or hematogenous, to the liver, brain, bones, and adrenal glands [3]. Gastric involvement in metastatic SCLC is rare [2]. Diagnosis of gastric SCLC metastases before primary disease is extremely rare [4]. In our case, the occurrence of nonspecific upper gastrointestinal symptoms with red flag signs prompted an endoscopic evaluation. Gastrointestinal metastases become symptomatic when the metastasis has grown substantially as metastatic cells initially infiltrate deeper portions of the bowel wall [4]. Nevertheless, both clinical and endoscopic features are nonspecific, and histopathological analysis is key to a correct diagnosis. In this instance, immunohistochemical identification of neuroendocrine makers such as chromogranin and synaptophysin is critical for identification of cellular lineage [1], and in our case, immunoreactivity to chromogranin and synaptophysin strongly suggested gastric involvement by a neuroendocrine neoplasm, later confirmed as a SCLC metastasis.
The prognosis of SCLC is poor, and a median survival of 4 months after diagnosis of gastric metastasis has been estimated [5]. Treatment of metastatic disease is palliative and first-line regimens include etoposide plus carboplatin or cisplatin [1]. Nevertheless, as described in the reported case, most patients have fast progression, ultimately succumbing to the disease within a few months.