A 46-year-old man presented with progressive dysphagia (to both solids and liquids), retrosternal chest pain, and low backache for 8 months. He also complained of significant weight loss and anorexia. There was no history of chronic or new medication use, consumption of tobacco or alcohol, and there were no comorbidities. His physical examination was normal except for mild tenderness in the sacral region. Laboratory results and chest X-ray were normal. Serology for HIV was negative. Upper gastrointestinal endoscopy revealed an ulcero-proliferative growth in the esophagus starting at 25 cm from incisors and resulting in stricture (Fig. 1a, arrow). The stricture was tight and irregular and was not transposable by the endoscope, hence the stomach could not be evaluated. Histopathological examination of biopsies taken from the lesion showed infiltration with sheets of atypical lymphoid cells with scattered mitotic figures suggestive of lymphoma (Fig. 2a, arrows). Immunohistochemistry (IHC) showed diffuse positivity for CD-20 and MUM-1 (Fig. 2b, c) and negativity for CD-3 and CD-23, suggesting the diagnosis of diffuse large B-cell type non-Hodgkin’s lymphoma. Contrast-enhanced abdominopelvic and chest computed tomography (CT) scan showed long segment circumferential thickening involving the distal 15 cm of the esophagus (Fig. 3a, b, arrow) with few small para-esophageal lymph nodes, and lytic lesions involving S1-S3 vertebrae suggestive of metastases (Fig. 3b, arrowhead). Magnetic resonance imaging of the spine also showed lytic lesions in the sacrum (Fig. 3c, arrowhead). Positron emission tomography with CT and bone marrow biopsy from the sacral region confirmed metastasis. Since dysphagia was severe, a self-expandable fully covered 18 mm × 150 mm esophageal metal stent was placed for palliation (Fig. 1b), and the patient was referred to the Oncology Department where he received R-CHOP (rituximab-cyclophosphamide, doxorubicin, vincristine, and prednisone) regimen. He also received external beam radiotherapy for sacral metastasis. His dysphagia improved and oral intake was satisfactory on follow-up at 8 weeks.
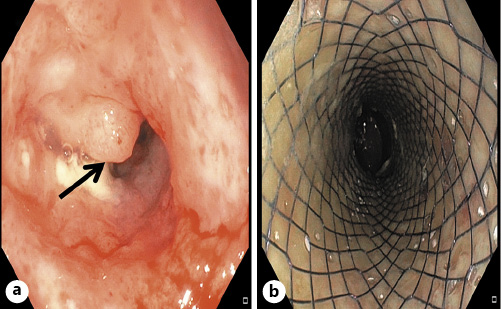
Fig. 1 a Endoscopy showing ulcero-proliferative growth (arrow) in the esophagus resulting in stricture. b A self-expandable esophageal metal stent placed across the esophageal growth.
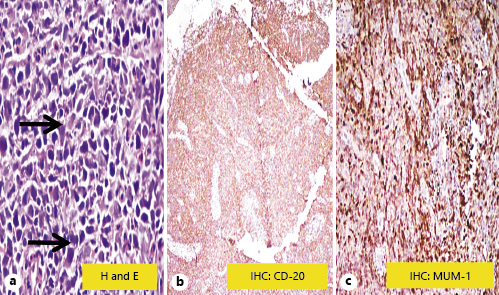
Fig. 2 a Histopathological examination showing infiltration with sheets of atypical lymphoid cells (arrows) with scattered mitotic figures suggestive of lymphoma. b IHC showing diffuse positivity for CD-20. c IHC showing positivity for MUM-1.
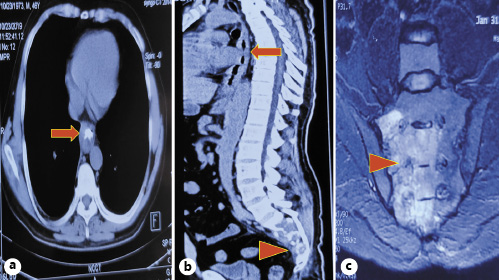
Fig. 3 a, b CT scan showing circumferential thickening (arrow) involving the distal 15 cm of the esophagus and sacral metastasis (arrowhead). c Magnetic resonance imaging scan showing sacral metastasis (arrowhead).
The esophagus represents a rare location of primary gastrointestinal lymphoma, and lymphoma accounts for less than 1% of all esophageal malignancies [1, 2]. Endoscopic mucosal resection has higher sensitivity than routine endoscopic pinch biopsies. Management usually involves chemotherapy, radiation, surgery, or a combination approach [3]. IHC in addition to conventional histopathology is important in establishing the diagnosis of this unusual malignancy [4].














