Introduction
IgG4-related disease (IgG4-RD) has recently been recognized as an autoimmune systemic disorder [1]. The first reports of the disease came from Japan where it was thought that autoimmune pancreatitis associated with high serum concentration of IgG4 and extra-pancreatic manifestations might be part of a more systemic autoimmune disorder [2].
IgG4-RD is diagnosed histologically as a dense lym-phoplasmacytic infiltrate with IgG4-positive cells, fibro-sis organized in a storiform pattern and obliterative phlebitis [3]. Many organs can be involved in the disease such as the pancreas, biliary tract, salivary glands, lymph nodes, thyroid, kidneys, lung, skin, prostate, and aorta. Involve-ment of the upper gastrointestinal tract is rare, and there have only been few case reports describing IgG4-related esophageal disease [3]. We report a case of IgG4-related esophageal disease presenting as chronic esophagitis with strictures.
Case Report
A young Caucasian woman was evaluated for a very long his-tory (years of evolution) of progressive odynophagia and dysphagia. Her medical history was positive for hypothyroidism. This patient was initially followed in primary care for symptoms of heartburn and dyspepsia. The presumed diagnosis was gastro-esophageal reflux disease and she was treated with a proton pump inhibitor (PPI), at a standard daily dose. The patient maintained complaints despite treatment with PPI, and an esophagogastro-duodenoscopy (EGD) was then requested. This endoscopic examination revealed a fibrous ring/membrane, just below the upper esophageal sphincter (UES) that was not amenable to be transposed by the endoscope. After this, a cervical CT scan was performed and revealed circumferential thickening of the upper cervical esophagus, not determining obstructive phenomena to the normal progression of the administered oral contrast. Given these findings, she was then referred to the Gastroenterology Department. A new EGD with possible endoscopic dilation was proposed, and it was accepted by the patient. This examination con-firmed a circumferential membranous ring just below the UES. Dilation was performed with a through-the-scope (TTS) balloon up to 10 mm, with deep laceration after the procedure. It was then possible to further advance the endoscope, and other mucosal rings were seen distally. Biopsies were performed, and histopathology revealed a probable IgG4-associated esophagitis due to lymphoplasmacytic infiltrate with large numbers of positive IgG4 plasma cells (>200/high power field), IgG:IgG4 ratio greater than 50%, nonobliterative phlebitis, and mild fibrosis, without stori-form pattern (Fig. 1). Serum IgG4 value was within the normal range (0.52 g/L).
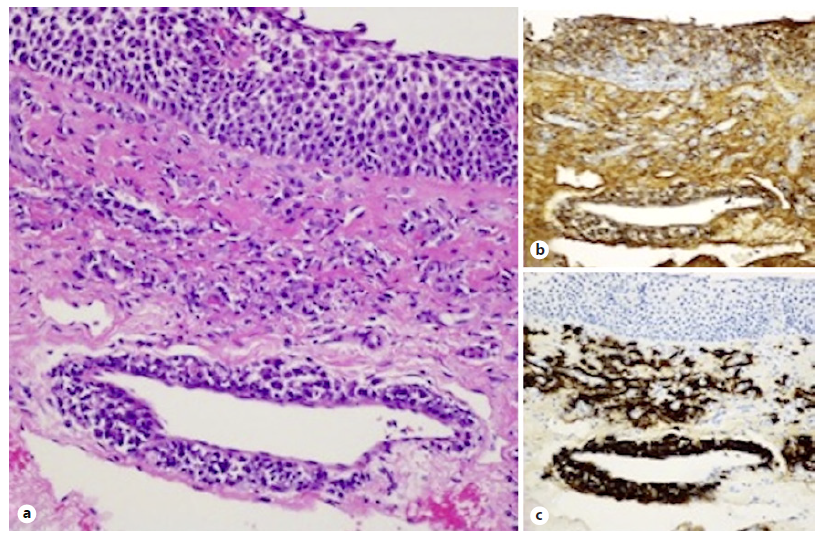
Fig. 1 a Esophageal biopsy showing a dense lymphoplasmacytic infiltrate with perivascular disposition and fibrosis. HE. ×200. Immunohistochemical staining with IgG (b, ×200) and IgG4 (c, ×200), with an IgG4/IgG ratio
Two months later, she maintained complaints of dysphagia, with only transient improvement after endoscopic dilation. Con-sidering the histological diagnosis and the possibility of a systemic disease, the following examinations were requested: blood tests to exclude autoimmune disease (immunoglobulins: IgG, IgA, IgE, IgM; antinuclear antibodies; antineutrophil cytoplasmic antibodies; tissue transglutaminase antibodies; serum protein electropho-resis; thyroid hormones) and immunoallergology evaluation to exclude possible association with food or other allergies. No changes were found in the requested exams. Liver enzymology was also normal, and there were no complaints of sialadenitis. In order to exclude the involvement of other organs, namely the pancreas, an MRI was carried out which did not reveal alterations.
Topical corticosteroids were started - oral puffs of fluticasone (220 μg/spray, four sprays daily in divided doses - twice daily) for 8 weeks.
Since there was no apparent symptomatic response, a new EGD was then proposed. There were two stenotic rings just below the UES and another one at the distal esophagus. Endoscopic dilation with a TTS balloon up to 10 mm was performed at both locations, and superficial lacerations were visible after treatment. It was then possible to advance the endoscope to the stomach. However, shortly after this endoscopic maneuver, the patient developed chest and cervical pain with subcutaneous emphysema. A CT scan confirmed an esophageal perforation, but since there were no signs of systemic toxicity, a conservative treatment was implemented after surgical consultation. The patient tolerated parenteral nutrition and antibiotics. A later water-soluble contrast showed a slight decrease in distensibility of the distal esophagus, with slow and intermittent passage of contrast to the stomach, but without extravasation or retention of contrast.
After full recovery, the patient was still symptomatic concerning dysphagia, and systemic corticoid therapy was proposed. However, the patient refused this medical option and decided to maintain the current status until her condition worsens.
Discussion
We report a 30-year-old woman with IgG4-related esophageal disease presenting as esophagitis with chronic strictures. Little is known about IgG4-RD-associated dysphagia.
In 2011, Lee et al. [4] described the first case of IgG4-related sclerosing esophagitis. Their patient had progressive dysphagia and weight loss, and the diagnosis was made by the histological study of the esophagectomy specimen.
The presentation of IgG4-RD is nonspecific because the symptoms depend on the affected organ. The reported symptoms of esophageal involvement include dysphagia, odynophagia, and weight loss. Endoscopy can reveal simple esophagitis, ulceration, stricture formation, sub-mucosal tumors, or even evidence of malignancy. The duration from the 1st symptom to diagnosis ranges from 11 months to 10 years [1, 4, 5].
The microscopic diagnosis of IgG4-RD requires both the typical histological appearance and increased numbers of IgG4 plasma cells or an elevated IgG4/IgG ratio. The three major histopathological features are: dense lymphoplasmacytic infiltrate; fibrosis, at least focally with a storiform pattern; and obliterative phlebitis. As the last two features are difficult to access in biopsy specimens, and a reliable pathological diagnosis requires the pres-ence of two of the three major histopathological features, the diagnosis rendered was of probability. Other two histopathological features are phlebitis without obliteration of the lumen, as seen in our case, and increased numbers of eosinophils. However, none of these findings, on their own, are either sensitive or specific for the diagnosis [6].
Corticosteroids are used as initial therapy for IgG4-related disease. Initial dosage of 0.6 mg/kg has been suggested in a 2012 Japanese consensus for treatment of symptomatic autoimmune pancreatitis, which included patients with symptomatic extra-pancreatic manifestations [7]. After 2-4 weeks, the dose is gradually tapered every 1-2 weeks until a maintenance dose of 2.5-5 mg of prednisolone is achieved. Corticosteroids can be stopped completely after a few months if the patient does not have residual active disease, but there is a high rate of relapse.
Immunomodulators such as azathioprine, methotrex-ate, and mycophenolate mofetil can be used as maintenance therapy and as a steroid-sparing strategy in patients refractory to or dependent on corticosteroid thera-py. Rituximab, a monoclonal antibody directed at CD20 antigen on B-lymphocytes, has recently been used in a few patients with disease refractory to standard treatment [8, 9].
In the present case, we had no opportunity to ascertain whether oral corticosteroid therapy could result in resolution of symptoms due to patient refusal. However, it is noticeable that topical corticosteroids, unlike in most cas-es of eosinophilic esophagitis, do not allow reversal of the symptoms, perhaps due to the high fibrotic component involved [10]. It is also clear that repeated dilation is not a therapeutic option to be taken into account in these patients with high fibrotic component and friable mucosa because of the complications that may be associated with it.
There are only two cases described in the literature that have undergone endoscopic dilation (prior to treatment with corticosteroids), with no mention of complications associated with the procedure. Until now, this is the first reported case in which an endoscopic dilation was performed in an IgG4-RD patient with associated complications.
Complications include pulmonary aspiration, bleeding, perforation, risks of sedation, and chest pain; the last of these being more common in patients with eosinophilic esophagitis [11]. According to the currently available literature, factors associated with a higher risk of perforation include complex stricture, stricture from eosinophilic esophagitis, malignancy-associated stricture, radiation-induced stricture, and limited experience of the practitioner performing the endoscopic procedure [12]. Strictures can be simple or complex. Simple strictures are short (<2 cm), concentric, straight, and allow the passage of a normal diameter endoscope. Complex strictures are usually longer (≥2 cm), angulated, irregular or have a severely narrowed diameter. These are more difficult to treat and have a tendency to be refractory or to recur despite dilatation [11].
There is nothing in the literature saying that patients with IgG4-RD have a higher risk of complications when performing endoscopic dilation. However, due to diffuse mucosal friability and ulceration with fibrotic changes, often ending up in complex strictures, these patients may be more predisposed to complications associated with endoscopic dilations. Therefore, medical therapy should be the first line of treatment to reduce the need for multiple esophageal dilations which can carry associated risks.
In conclusion, although IgG4-related sclerosing disease rarely manifests in the esophagus, clinicians and pathologists should consider this condition in the differential diagnosis of unexplained esophagitis with strictures in order to avoid unwarranted esophagectomies and failed medical treatment due to lack of recognition of this rare entity.














