An 81-year-old male patient presented for ileocolonoscopy for anemia workup. While smaller polypoid lesions in the remaining colon were resected without complications, an estimated 50-mm, complex pedunculated (Paris Ip) lesion with a unique multinodular, uneven sur-face was observed in the sigmoid (Fig. 1a). However, dedicated optical assessment of large areas of the lesion indicated adenomatypical vessel and surface pattern, albeit full optical assessment of the large and floppy lesion was not feasible (EC760R-V/I; Fuji, Düsseldorf, Germany) (Fig. 1b). More intriguingly, the 25-mm-long and 10-mm-wide stalk demonstrated marked varices originating from adjacent flat sigmoid mucosa (Fig. 1c). Given concerns as to whether adequate placement of a snare and/or prophylactic loop would be feasible in consideration of the large head and markedly uneven surface, in this unique setting we opted for an individual approach, implementing stalk transection after endoscopic band ligation. To this end, we provided the insertion point at 35 cm with two rubber bands as per standard procedure (Fig. 1d, e). Alternatively, clip application at the stalk base might have been discussed for prophylactic hemostasis. However, this was decided against due to, among others, concerns for thermal injury. Capfitted gastroscope reinsertion exposed the edematous stalk with the ligations at 6 o’clock and the polyp head at 12 o’clock (Fig. 1f).
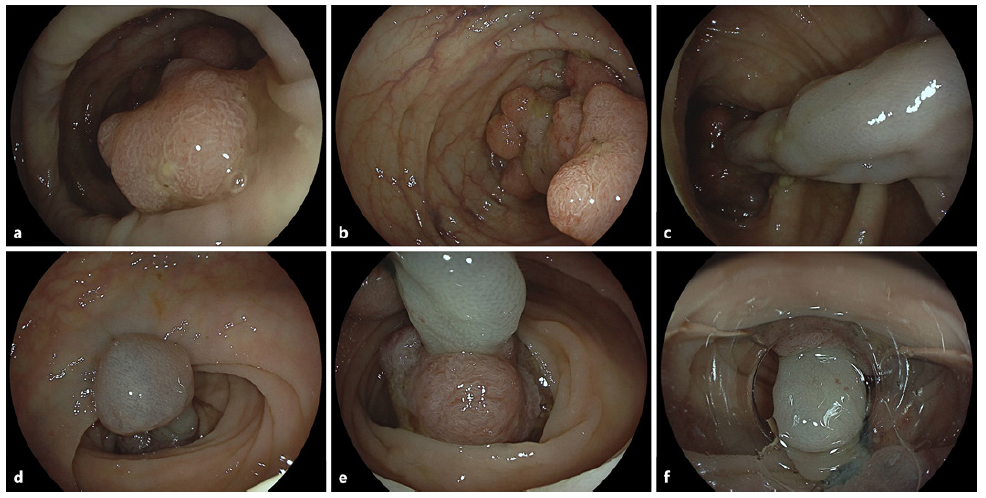
Fig. 1 a, b Endoscopic illustration of a large pedunculated Paris Ip lesion estimated at 50 mm in the sigmoid colon with an uneven, multinodular surface. Limited optical assessment suggested adenoma-typical regular surface and vessel pattern. c Of note, the estimated 25-mm stalk exhibited prominent stalk varices. d, e Visualization of the first anal side endoscopic band ligation (d) and the second one at upper left (e) (note marked traction-relat-ed stalk shortening). f Capfitted visualization of the operative situs with the two ligations at 6 o’clock and the polyp head at 12 o’clock.
Next, we completed an uncomplicated forceps scissor transection of the highly fibrotic stalk, using a scissor-type knife device, only at the first cut resulting in self-limited bleeding from ligated varices (Fig. 2a, b). Electrosurgical settings were as follows: transection (mucosa and submucosa): Endocut Q, effect 2, duration 3, interval 1; hemostasis (not needed): soft coagulation, effect 5, 100 W (VIO 200D; Erbe Elektromedizin, Tübingen, Germany) Postinterventional assessment of the resection site excluded hemorrhage with the two bands still in situ (Fig. 2c). The specimen was retrieved by a Roth net. Final pathology confirmed R0 resection of low-grade intraepithelial neoplasia (Fig. 2d).
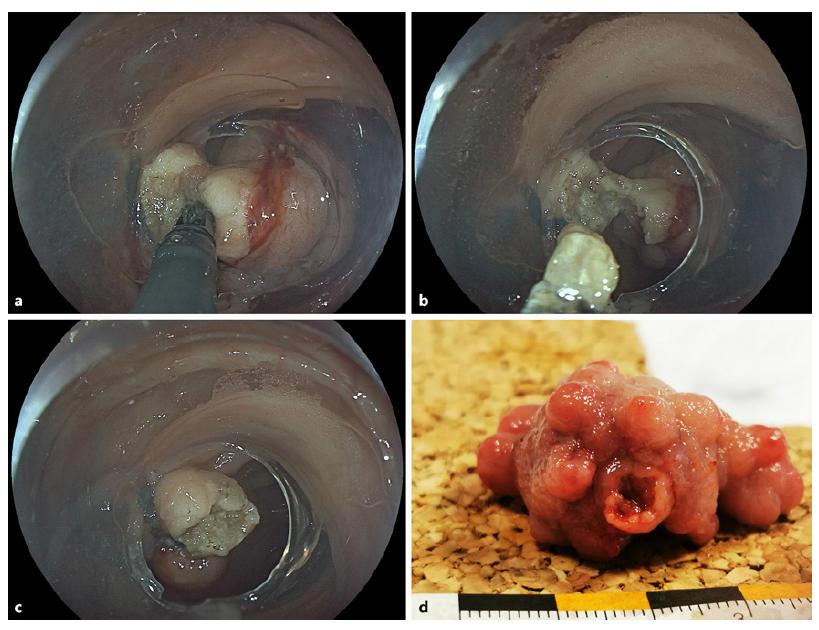
Fig. 2 a Stalk transection using a scissor-type knife (3.5-mm ClutchCutter, Fuji) utilizing an 18.1-mm large-diameter oblique transparent cap (D-206-5; Olympus, Hamburg, Germany) for improved intracap device rotation. b Progression of transection prior to the final cut; note lack of hemorrhage during the procedure. c Final endoscopic result with the two ligations still in situ and lack of bleeding. d Ex vivo representation of the specimen after Roth net retrieval.
While stalk transection of large pedunculated lesions has been well documented in the literature, a combinatorial approach involving band ligation of associated stalk varices is altogether novel [1, 2]. A literature review identified a similar case involving band ligation of adjacent cirrhosis-related varices in a unique patient undergoing rectal endoscopic submucosal dissection [3]. In addition, a recent pilot study has pioneered endoscopic band ligation of longer stalks combined with standard snare-based polypectomy [4]. In the absence of portal hypertension and more widespread dilated veins throughout the colon, stalk varices were considered to be directly related to the giant head of this pedunculated lesion.














