Biliary decompression in cases of hilar obstruction is challenging, and the intrahepatic approach is often necessary [1]. We describe a case of endoscopic ultrasound-guided biliary drainage (EUS-BD) for unresectable hilar malignant obstruction, using lumen-apposing metal stent (LAMS).
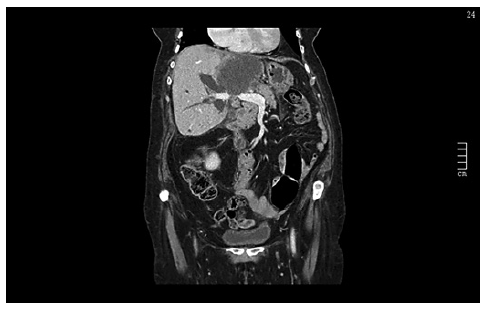
A 85-year-old woman was admitted due to abdominal pain, jaundice, and choluria. From the personal history, it is worth noting a rectovaginal septum gastrointestinal stromal tumor (GIST), treated surgically in 2002 and with imatinib for 2 years. She was also being followed for pulmonary nodules, suspected of malignancy. Abdominal computed tomography showed a 76 × 57 × 61 mm mass on the left hepatic lobe, with irregular borders, and central necrosis, suggestive of metastasis. This mass compressed the biliary tree at the hilar plaque and led to intrahepatic biliary dilatation (Fig. 1). She had portal vein invasion, pulmonary and peritoneal metastasis. Biochemical workup showed a cytocholestase pattern and total bilirubin of 26 mg/dL. The patient refused liver biopsy. After multidisciplinary discussion it was decided for an endoscopic palliative treatment. Transpapillary access through endoscopic retrograde cholangiopancreatography (ERCP) was attempted but failed due to impossibility of biliary cannulation.
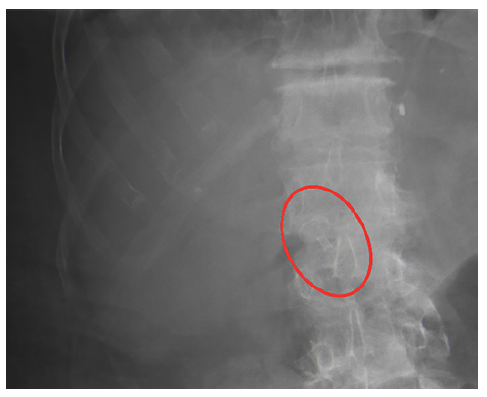
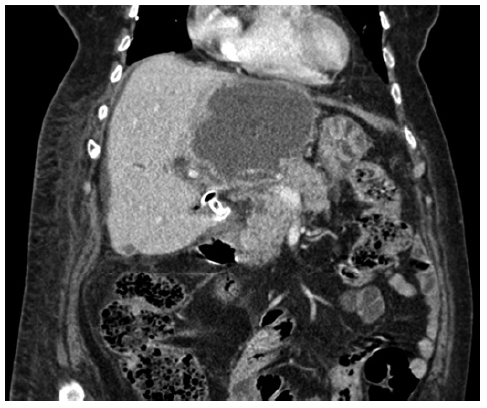
The procedure was performed under deep sedation. A linear echoendoscope (GF-UCT260; Olympus Medical Systems, Tokyo, Japan) was used. There was a significant intrahepatic biliary dilation (12.8 mm), and the right intrahepatic biliary duct was close enough to the duodenal bulb (5 mm), without intervening vessels (as confirmed by color doppler). As so, we performed an hepaticoduo-denostomy using a 6 × 8 mm LAMS (HotAxiosTM, Boston Scientific®, Marlborough, MA, USA): under ultrasound control, the right intrahepatic biliary duct was punctured through the duodenal bulb. After deployment of the stent, we assisted to an abundant drainage of bile (online supplementary video, available at https://www.karger.com/doi/10.1159/000522578). Position of the stent was confirmed at the end of the procedure by fluoroscopy (Fig. 2). The patient showed a clinical and laboratory improvement, with a total bilirubin of 7.37 mg/dL 72 h after the procedure. Control abdominal CT showed an improvement in intrahepatic biliary dilatation (Fig. 3). She was followed in palliative care, remained asymptomatic and without complications related to the LAMS. She died 33 days after the procedure, due to disease progression.
The ease of deployment, lumen apposition configuration, and wider diameter of LAMS led to its use in an expanding variety of clinical scenarios, with a good safety profile [2]. Nevertheless, there are risks associated with its use, most commonly misdeployment of the distal or proximal flange and massive bleeding during fistulotomy [3]. Long-term complications described with the use of LAMS are stent migration or obstruction due to tumor progression or food impaction [4].
Although EUS-BD with LAMS has been extensively reported at the extrahepatic duct, LAMS may be an option to intrahepatic EUS-BD when there is enough intrahepatic duct dilation, no intervening vessels, and a stable access route [5]. We describe one of the first cases of hepaticoduodenostomy using LAMS.